Translate this page into:
Spirometry-based prevalence of chronic obstructive pulmonary disease & associated factors among community-dwelling rural elderly
For correspondence: Dr Ravneet Kaur, Centre for Community Medicine, Old OT Block, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110 029, India e-mail: ravneetk08@gmail.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Chronic obstructive pulmonary disease (COPD) is a major public health problem in India. Its magnitude is particularly high among the elderly. Old age and comorbidity may lead to misdiagnosis and under treatment of this condition. COPD is not curable; however, various forms of treatment can help control symptoms and improve the quality of life. Most of the earlier studies lacked uniformity in definitions, designs, methodology and reporting techniques. Studies based on spirometry are only a few. Understanding the current prevalence and associated factors of COPD is important for planning control strategies. Hence, this study was conducted to determine the prevalence of COPD and associated factors among the elderly.
Methods:
In this community-based study among 449 elderly persons in a rural area, information regarding socio-demographic details, selected health conditions and exposure to risk factors was recorded. The assessment of airway obstruction was done by using a portable spirometer (MIR Spirolab). The diagnosis of COPD was based on the GOLD criteria. The association of COPD with sociodemographic and other variables was analysed by the multivariate logistic regression.
Results:
Acceptable spirometry findings were available for 392 (87.3%) participants. The prevalence of COPD was 42.9 per cent (95% confidence interval 37.9-47.7%). The prevalence was 54.5 per cent among men and 33.4 per cent among women. Smoking, higher age group and low body mass index were significantly associated with COPD.
Interpretation & conclusions:
The prevalence of COPD was found to be high among the rural elderly in this study. Interventions aimed at cessation of smoking and preparedness of health systems for diagnosis and management of COPD are hence required.
Keywords
COPD
community-based
community-dwelling
elderly
rural
spirometry
The burden of chronic respiratory diseases is increasing worldwide. Globally, 235 million people have asthma; 64 million people have chronic obstructive pulmonary disease (COPD) while millions have other underdiagnosed chronic respiratory diseases1. The COPD burden is projected to increase in coming decades because of continued exposure to COPD risk factors and ageing of the population. As reported by the World Health Organization (WHO), COPD was the third leading cause of death in WHO-SEAR (South-East Asia Region) in 20152. Besides death, COPD is associated with significant morbidity and an economic burden due to hospitalization, medical expenditure for home-based care and loss of productivity. In 2013, COPD was the fifth leading cause of Disability Adjusted Life Years (DALYs) lost3. In India, as reported by the India State-level Disease Burden Initiative (2017), COPD was responsible for 8.7 per cent of total deaths and 4.8 per cent of total DALYs in 20164.
Although community-based studies on COPD are available; however, existing COPD prevalence data vary widely due to differences in study design, diagnostic criteria, methodology and reporting techniques. Moreover, studies measuring airflow obstruction by using pulmonary function tests are few in India. The reported prevalence of COPD varies from 2 to 22 per cent in different studies, conducted among different age groups5. The magnitude of COPD is much higher among elderly persons. As per the 2011 census, 103.2 million people in India were of the age of 60 yr or more, accounting for 8.6 per cent of the total population6. COPD is associated with a number of co-morbidities among elderly persons. Old age and comorbidity may lead to misdiagnosis and under treatment of COPD among the elderly78. COPD is not curable; however, various forms of treatment can help control symptoms and improve the quality of life for elderly people with the disease58.
Understanding the current prevalence of COPD and identification of the associated factors is important for planning sustainable prevention and management strategies. This study was conducted among the elderly in a rural community to determine the prevalence of COPD, wherein airflow obstruction was assessed by spirometry. The factors associated with COPD among the elderly were also studied.
Material & Methods
This community-based study was conducted in the Ballabgarh block of Faridabad district of Haryana. The study area consisted of 28 villages in the rural field practice area of the research institute and had a population of nearly 98,000 individuals in the year 20169. There was a computerized database of all individuals residing in the area, and the same was updated annually. The study was conducted among persons aged 60 yr or more, residing in the area for more than one year.
Sample size: The sample size calculation was guided by the findings of a multi-centric study conducted by Jindal et al10, where the prevalence of chronic respiratory diseases in the population aged 15 yr and above was reported to be 8.5 per cent. The review of literature suggests that the prevalence among persons aged 60 yr or more is two to three times higher than the general population7.
Hence, the prevalence among elderly persons in the present study was assumed to be 20 per cent. Taking a relative precision of 20 per cent, the sample size was calculated to be 400. Considering non-response rate of 15 and 5 per cent for death and migration, respectively, the calculated sample size was increased to 500 elderly.
Data collection: A list of persons aged 60 yr or more was taken from the computerized database. Out of total 6765 individuals aged 60 yr and above, 500 participants were selected by simple random sampling using computer-generated random numbers.
Data collection was undertaken from October to December 2017. House-to-house visit was done for all 500 elderly. In case a participant was not found at home despite three visits, he/she was categorized as a non-respondent.
Seriously-ill elderly, those not able to comprehend, or having conditions that affect safety during spirometry (viz. any surgery or severe injury in the abdomen, chest or eye in the last three months, myocardial infarction in the last three months, hospitalization due to heart disease within the past month or currently on treatment for TB) were excluded from the study.
Survey methodology: The study was conducted after taking approval from the Institutional Ethics Committee of All India Institute of Medical Sciences, New Delhi. Written informed consent was taken from all the participants. The results of the examination were communicated to the participants on the same day. All information collected was kept confidential. Participants found to be having COPD were referred to appropriate OPD at the nearest health facility.
The elderly who were currently suffering or had suffered from acute respiratory infections in the past two weeks were rescheduled to a later date. Elderly taking medications (bronchodilators and/or steroids) were asked to withhold medication overnight for 12 h and early morning examination was done for such cases.
A pre-tested semi-structured interview schedule was administered and information was collected regarding socio-demographic details, history of chronic respiratory symptoms or disease, family history of chronic respiratory disease, consumption of tobacco, exposure to tobacco smoke or biomass fuel (indoor air pollution), self-reported or physician-diagnosed illness (diabetes, hypertension and arthritis) for which the patient was under medication for at least the preceeding six months.
Arm span (AS) and weight of participants was recorded, and body mass index (BMI) was calculated as BMI = weight (in kg)/(AS in meter)11.
Assessment of functional disability was done by using Barthel’s Activity of Daily Living Index (ADL)12.
For assessment of airway obstruction, spirometry was performed. A hand-held portable spirometer-MIR (Medical International Research) Spirolab® (Roma, Italy) was used. The measurements were done according to the standard guidelines (American Thoracic Society and European Respiratory Society)13.
For each participant, information of weight and height was entered in the spirometer. The participant was asked to sit comfortably. Two measurements – one each of pre- and post-bronchodilator (salbutamol inhalation - 4 puffs of 100 mcg each), were performed at least 20 min apart, according to standard ATS/ERS guidelines13.
The diagnosis of COPD was based on the GOLD guidelines 201914. History of exposure to risk factors such as tobacco smoking, exposure to environmental tobacco smoke, biomass fuel or occupational exposure to dust, along with the presence of airflow limitation that was not fully reversible, (with or without the presence of symptoms), i.e. the ratio of post-bronchodilator forced expiratory volume in first second of expiration, and the forced vital capacity (FEV1/FVC) <70 per cent on spirometry, was considered as COPD14. ERS-93 was used to predict normal FEV115. The severity of COPD was measured according to the GOLD guidelines14. The values of FEV1 from 50 to 79.9 per cent of the predicted value indicated moderately severe disease, FEV1 30-49.9 per cent specified severe disease, while FEV1 <30 per cent indicated very severe disease.
The results were printed and communicated to the participants at the end. ‘Quality A’ meant three acceptable tests, i.e. the variation of the two highest FEV1 values less than or equal to 150 ml16.
Quality assurance: The spirometer used for the study (MIR Spirolab) complied with the ATS/ERS criteria for accuracy. The investigator (AK) was trained in the pulmonary laboratory of the research institute for 150 h under the supervision of a faculty member of the department of Pulmonary Medicine & Sleep Disorders AIIMS, New Delhi, who had more than 10 yr of experience in this area (VH). During this period AK performed 50 spirometry tests, among patients of all age groups, with the assistance of a pulmonary laboratory technician, and 50 unassisted spirometry tests among elderly patients in the pulmonary laboratory.
Before data collection, the investigator (AK) performed the spirometry among elderly patients with the portable MIR spirolab spirometer, the findings of which were confirmed by the spirometer at the institutional pulmonary laboratory. All the tests were re-read by the expert for interpretation.
The spirometer was standardized and calibrated at the pulmonology laboratory and the diagnosis of COPD was made according to the GOLD guidelines for spirometry. Standard operational definitions were used for rest of the parameters.
Statistical analysis: Data were entered and managed in MS Excel 2016, and statistical analysis was carried out using Stata 12.0 (Stata Corp LLC 4905, Texas, USA)17. Mean, standard deviation (SD) and frequency (percentage) were reported for the continuous and categorical variables, respectively. The prevalence of chronic respiratory diseases was reported as percentage with 95 per cent confidence interval (CI). Contingency table analysis was done using the Chi-square results. The association of socio-demographic and various risk factors with COPD was analysed using the logistic regression analysis. Univariable analysis followed by multivariable logistic regression analysis was carried out. Variables with P<0.25 were considered for multivariable analysis. The results were presented as an odds ratio (OR) with 95 per cent confidence level. P<0.05 was considered statistically significant.
Results
Out of 500 randomly selected elderly, one had died in the previous year, three had migrated, and one had rib fracture. Out of 495 eligible elderly, 44 were not available even after three visits, while two did not give consent. The remaining 449 participants were included in the study. Thus, the response rate was 90.7 per cent (Figure). The response rate was higher among women (94.5%) as compared to men (86.1%). The reason for more participation by women was their availability during the house visits made by the investigator. Comparatively more men were unavailable despite three house visits and were considered as non-responders.
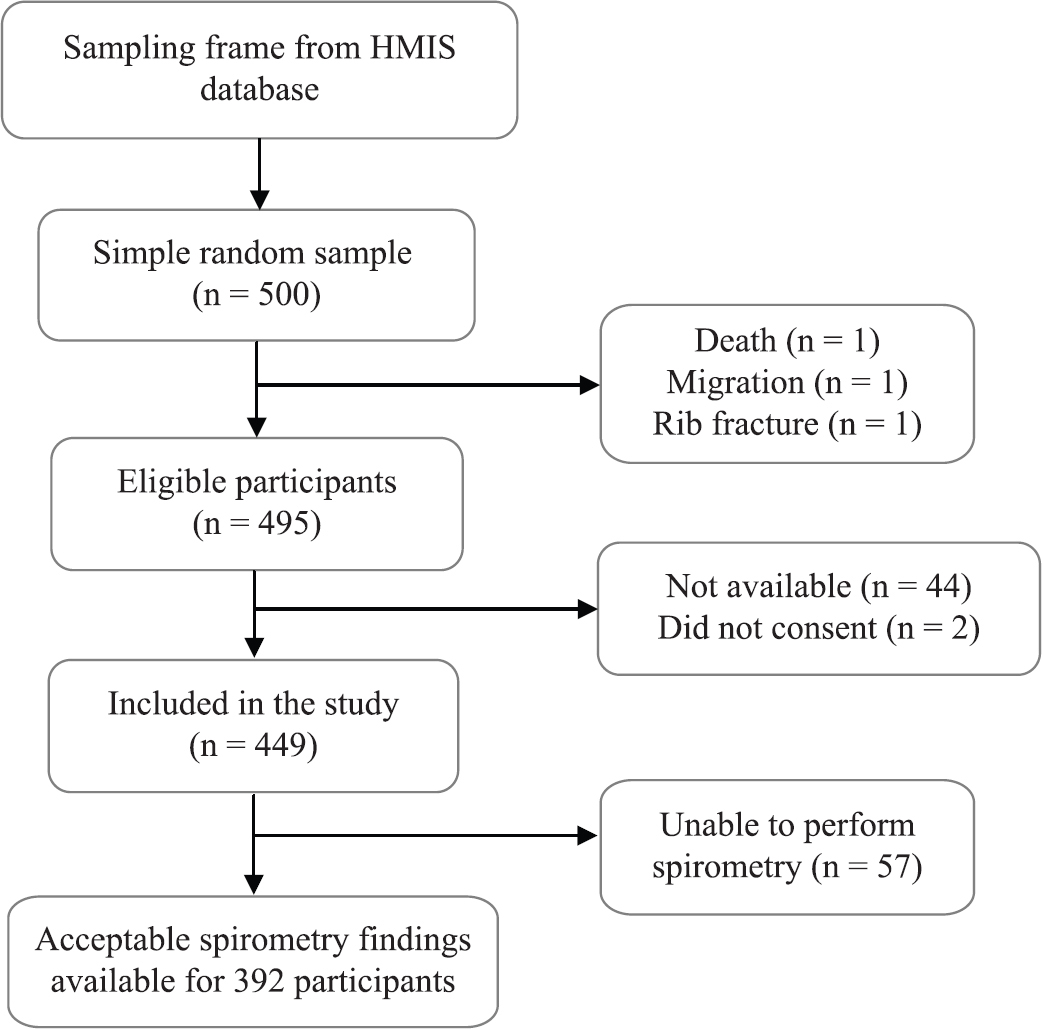
- Flow of study participants.
Of the 449 participants included in the study, at least one acceptable spirometer finding was available for 392 (87.3%) participants. Table I shows the characteristics of the study participants. Out of 392 participants, 218 (55.6%) were women. The mean age was 68.1 yr (SD=6.6), being 68.4 (SD=6.4) for men and 67.9 (SD=6.6) for women. Majority (66.1%) of the participants were in the age group of 60-69 yr, while 33.9 per cent were aged 70 yr or above. Nearly three-fourth of the participants (73.5%) were illiterate. Among men 46.6 per cent were illiterate while 95.0 per cent of the elderly women were illiterate. Two hundred and seventy-two participants (69.4%) were currently married, whereas 30.6 per cent were widowed or separated (16.1% of men and 42.2% of women). Most (92.6%) of the participants were economically dependent on others. Majority (62.8%) of the participants belonged to low socio-economic status. The past occupation was agriculture/labour for 75.3 per cent of men, whereas 97.7 per cent of the women were homemakers.
| Variables | Male (n=174), n (%) | Female (n=218), n (%) | Total (n=392), n (%) |
|---|---|---|---|
| Age (yr) | |||
| 60-64 | 55 (31.6) | 85 (39.0) | 140 (35.7) |
| 65-69 | 63 (36.2) | 56 (25.7) | 119 (30.4) |
| ≥70 | 56 (32.2) | 77 (35.32) | 133 (33.9) |
| Literacy | |||
| Illiterate | 81 (46.6) | 207 (95.0) | 288 (73.5) |
| Literate | 93 (53.5) | 11 (5.1) | 104 (26.5) |
| Udai Pareek SES Scale | |||
| Lower class | 3 (1.7) | 2 (0.9) | 5 (1.3) |
| Lower middle | 45 (25.9) | 196 (89.9) | 241 (61.5) |
| Middle | 112 (64.4) | 20 (9.2) | 132 (33.7) |
| Upper middle | 14 (8.1) | 0 | 14 (3.6) |
| Marital status | |||
| Married | 146 (83.9) | 126 (57.8) | 272 (69.4) |
| Widow/widower/single/separated | 28 (16.1) | 92 (42.2) | 120 (30.6) |
| Economic status | |||
| Economically independent | 25 (14.4) | 4 (1.8) | 29 (7.4) |
| Dependent on the care providers | 149 (85.6) | 214 (98.2) | 363 (92.6) |
| Past occupation | |||
| Homemaker/stay at home | 2 (1.2) | 213 (97.7) | 215 (54.9) |
| Service/business | 41 (23.6) | 1 (0.5) | 42 (10.7) |
| Cultivation/labour | 131 (75.3) | 4 (1.8) | 135 (34.4) |
| Smoking | |||
| Present | 121 (69.5) | 76 (34.9) | 197 (50.3) |
| Absent | 53 (30.5) | 142 (65.1) | 195 (49.7) |
| Respiratory symptoms* | |||
| Chronic cough | 33 (19.0) | 23 (10.6) | 56 (14.3) |
| Chronic phlegm | 33 (19.0) | 15 (6.9) | 48 (12.2) |
| Dyspnoea | 53 (30.5) | 54 (24.8) | 107 (27.3) |
| Recurrent wheeze | 16 (9.2) | 10 (4.6) | 26 (6.6) |
| History of ATT | 5 (2.9) | 2 (0.9) | 7 (1.8) |
| BMI | |||
| Low (below 18.5 kg/m2) | 75 (43.1) | 52 (23.9) | 127 (32.4) |
| Normal (18.5-25 kg/m2) | 87 (50.0) | 125 (57.3) | 212 (54.1) |
| High (25 kg/m2 and above) | 12 (6.9) | 41 (18.8) | 53 (13.5) |
*Multiple responses possible. BMI, body mass index; ATT, anti-tuberculosis treatment; SES, socioeconomic status
Nearly half (50.3%) of the participants reported to have ever smoked tobacco while 41.0 per cent of all participants were current smokers. Out of these, majority (60.6%) were men. Nearly 75 per cent of the smokers had been smoking for 30 years or more, whereas 17.7 per cent smoked for 15-30 years. Majority of the smokers (65.5%) smoked beedi (hand-rolled cigarette), while 42.9 per cent smoked hookah (hubble-bubble). Only two participants smoked cigarette. Most of the women (90.2%) cooked food regularly in the past. Wood was the most commonly used fire-fuel (93.4%) among the participants, whereas cow dung cakes were used by 3.9 per cent of the participants. Thus, 97.3 per cent of the participants had exposure to biomass fuel. The mean (±SD) exposure years were 33.2 (±7.9).
Regarding self-reported health conditions, hypertension and diabetes were reported by 9.4 and 5.6 per cent of the participants, respectively. Seven (1.8%) elderly reported a history of anti-tuberculosis treatment, whereas 27.3 per cent of the participants reported shortness of breath. Chronic cough and chronic phlegm were reported by 14.3 and 12.2 per cent of the participants, respectively while 6.6 per cent had recurrent wheeze. The mean (±SD) duration of chronic cough was 4.04±2.28 yr, chronic phlegm was 4.02±2.20 yr, recurrent wheeze was 4.88±2.88 yr and dyspnoea was 4.22±3.36 yr. According to Barthel’s ADL score, 38 (9.7%) of the participants had some functional disability. Low BMI (<18.5 kg/m2) was found in 32.4 per cent of the participants, whereas 13.5 per cent had high BMI (25 kg/m2).
Table II shows the distribution of FEV1/FVC ratio among study participants. Mean (±SD) of FEV1/FVC among men was 66.05±13.48, whereas it was 73.28±11.89 among women. Mean (±SD) of FEV1/FVC among the total participants was 70.07±13.11.
| Gender | Age group (yr) | Number of individuals | FEV1/FVC (mean±SD) | FEV1/FVC <0.7 per cent (SE) |
|---|---|---|---|---|
| Male | 60-64 | 55 | 66.93±14.67 | 49.1 (6.8) |
| 65-69 | 63 | 67.6±12.78 | 46.0 (6.3) | |
| ≥70 | 56 | 63.43±12.87 | 69.6 (6.2) | |
| Total | 174 | 66.05±13.48 | 54.6 (3.8) | |
| Female | 60-64 | 85 | 75.66±11.18 | 24.7 (4.7) |
| 65-69 | 56 | 72.02±11.68 | 39.3 (6.6) | |
| ≥70 | 77 | 71.56±12.51 | 39.0 (5.6) | |
| Total | 218 | 73.28±11.89 | 33.5 (3.2) | |
| Total | 60-64 | 140 | 72.23±13.32 | 34.3 (4.0) |
| 65-69 | 119 | 69.68±12.42 | 42.9 (4.6) | |
| ≥70 | 133 | 68.14±13.24 | 51.9 (4.3) | |
| Total | 392 | 70.07±13.11 | 42.9 (2.5) |
SD, standard deviation; SE, standard error
In our study, the prevalence of COPD, as diagnosed by the post-bronchodilator spirometric value of FEV1/FVC <0.7, was 42.9 per cent (95% CI 37.9-47.7). Among those having COPD, 48.8 per cent had moderately severe disease, 22 per cent had severe disease, while 6.5 per cent had very severe disease. The prevalence of COPD was more among men (54.5%) as compared to women (33.4%) (Table III).
| Prevalence | Male (n=174), n (%) | Female (n=218), n (%) | Total (n=392), n (%) |
|---|---|---|---|
| COPD (FEV1/FVC <0.7), 95% CI | 95 (54.5), 47.1-62.0 | 73 (33.4), 27.2-39.8 | 168 (42.9), 37.9-47.7 |
| Severity | |||
| Mild (FEV1% predicted 80 and above) | 23 (13.2) | 15 (6.8) | 38 (9.7) |
| Moderate (FEV1% predicted 50-79.9) | 45 (25.9) | 37 (17) | 82 (20.9) |
| Severe (FEV1% predicted 30-49.9) | 18 (10.3) | 19 (8.7) | 37 (9.4) |
| Very severe (FEV1% predicted <30) | 9 (5.2) | 2 (0.9) | 11 (2.8) |
volume in one second; CI, confidence interval
Table IV shows the distribution of respiratory symptoms among participants with COPD and without COPD. A significantly higher proportion of participants with COPD had respiratory symptoms as compared to those without COPD.
| Symptoms | Total (n=392) | COPD present (n=168), n (%) | COPD absent (n=224), n (%) | Odds ratio (95% CI) |
|---|---|---|---|---|
| Chronic cough | 56 | 44 (26.2) | 12 (5.4) | 6.27 (3.19-12.32)*** |
| Chronic phlegm | 48 | 42 (25.0) | 6 (2.7) | 12.11 (5.01-29.29)* |
| Dyspnoea | 107 | 78 (46.4) | 29 (12.9) | 5.83 (3.56-9.55)** |
| Recurrent wheeze | 26 | 24 (14.3) | 2 (0.89) | 18.50 (4.31-79.47)* |
P *<0.05, **<0.01, ***<0.001
The prevalence of COPD was significantly higher as the age group increased. (Chi-square for trend: 8.62, P-value for trend: 0.013). The prevalence was also found to be more among smokers (58.8%; 95% CI=51.9-65.8%) as compared to non-smokers (26.6%; 95% CI=20.4-32.9%). We found that 26.7 per cent of non-smokers had COPD. The risk factors among non-smokers were exposure to agricultural dust (n=8), exposure to dust at construction sites (n=2) and exposure to biomass fuel (n=35).
Association of COPD with socio-demographic and selected clinical variables is shown in Table V. In univariate analysis, it was found that age, male sex, low socio-economic status, low literacy, low BMI and smoking were associated with COPD. Following univariate analysis, multivariate logistic regression was carried out. The variables with P<0.25 were considered for the multivariate analysis.
| Variable | Number of participants (n=392) | COPD present (n=168), n (%) | Unadjusted odds ratio (95% CI) | P | Adjusted odds ratio (95% CI) | P |
|---|---|---|---|---|---|---|
| Age (yr) | ||||||
| 60-64 | 140 | 48 (34.3) | ||||
| 65-69 | 119 | 51 (42.9) | 1.44 (0.86-2.38) | 0.158 | 1.38 (0.79-2.40) | 0.256 |
| ≥70 | 133 | 69 (51.9) | 2.07 (1.27-3.36) | 0.004 | 1.77 (1.04-3.05) | 0.036 |
| Gender | ||||||
| Female | 218 | 73 (33.5) | ||||
| Male | 174 | 95 (54.6) | 2.39 (1.59-3.60) | <0.001 | 1.66 (0.88-3.13) | 0.115 |
| Literacy | ||||||
| Illiterate | 288 | 117 (40.6) | ||||
| Literate | 104 | 51 (49.0) | 1.4 (0.89-2.21) | 0.138 | 0.88 (0.45-1.70) | 0.702 |
| Marital status | ||||||
| Married | 272 | 120 (44.1) | ||||
| Widow/single/separated | 120 | 48 (40.0) | 0.84 (0.55-1.31) | 0.448 | - | - |
| Economic dependence | ||||||
| Independent | 29 | 12 (41.4) | ||||
| Dependent | 363 | 156 (43.0) | 1.07 (0.5-2.3) | 0.867 | - | - |
| SES | ||||||
| High | 146 | 71 (48.6) | ||||
| Low | 246 | 97 (39.4) | 0.68 (0.45-1.03) | 0.076 | 1.13 (0.58-2.22) | 0.714 |
| Smoking | ||||||
| Absent | 195 | 52 (26.7) | ||||
| Present | 197 | 116 (58.9) | 3.94 (2.57-6.03) | <0.001 | 2.97 (1.86-4.74) | <0.001 |
| History of ATT | ||||||
| Absent | 385 | 165 (42.9) | ||||
| Present | 7 | 3 (42.9) | 1 (0.22-4.53) | 1.000 | - | - |
| BMI (kg/m2) | ||||||
| Normal (18.5-25) | 212 | 71 (33.5) | ||||
| Low (below 18.5) | 127 | 83 (65.4) | 3.75 (2.36-5.96) | <0.001 | 2.99 (1.81-4.93) | <0.001 |
| High (25 and above) | 53 | 14 (26.4) | 0.71 (0.36-1.4) | 0.325 | 0.93 (0.46-1.90) | 0.848 |
BMI, body mass index; ATT, anti-tuberculosis treatment; SES, socio-economic status
Age 70 yr or above [P=0.036, OR 1.77 (1.04-3.05)], low BMI [P<0.001, OR 2.99 (1.81-4.93)] and smoking [P<0.001, OR 2.97 (1.86-4.74)] were significantly associated with COPD.
Discussion
In this study, we report the magnitude of COPD among the community-dwelling rural elderly by using spirometry. Out of 449 participants enrolled, 392 (87.3%) were able to perform spirometry of acceptable quality. This figure is fairly higher in comparison to other reported studies. In a study in rural setting of Tanzania, spirometry could be performed only in 57.1 per cent of the participants18. In India, in a community-based study conducted in Kashmir among adults aged 40 yr and above, acceptable spirometry results were available for 79 per cent of the participants19. Higher spirometry rate in our study may be due to the fact that the investigator got thorough training at the laboratory of a tertiary care institute. The investigator was also supervised in the field by a community medicine specialist and support was provided whenever required. Moreover, the participants were elderly persons aged 60 yr and above, having various respiratory symptoms. The felt need for investigations among participants might have led to a higher response rate for spirometry.
In this study, the prevalence of COPD by the GOLD criteria of FEV1/FVC <0.7 was 42.9 per cent (95% CI 37.9-47.7). This finding is similar to a spirometry-based study done by Koul et al19 in rural Kashmir in which the prevalence of COPD among persons aged 60 yr and above was reported to be 41.4 per cent. In a study done by Sinha et al20 in Delhi, the prevalence was 31.4 per cent which was lower than ours. Sharma et al21 reported a prevalence of 12.5 per cent among persons aged 60 yr and above in rural Jammu, which is lower than our study. They, however, used peak flow meter to assess the prevalence of COPD, which is a less sensitive method than spirometry.
Similar spirometry-based studies conducted in Russia, Egypt, Iran and Saudi Arabia have reported a much lower prevalence of 6.6, 6.6, 9.2 and 4.2 per cent, respectively22232425. However, studies from Korea and rural Tanzania have reported a similar prevalence of 35 and 41.7 per cent, respectively1826.
COPD was significantly associated with smoking, low BMI and higher age. This is similar to other studies conducted in India and abroad272829.
Male sex, low socio-economic status and low education status have been reported to be associated with COPD in some studies303132. In our study, these were found to be associated in univariate analysis but not in multivariate analysis.
This study had a few limitations. Biomass exposure index could not be calculated, as detailed history in terms of hours of exposure per day was not enquired in the study. Moreover, the effect of biomass fuel could not be studied because none of the men used to cook and almost all participants (97.3%) used biomass fuel only. In most of the rural households, cooking was done in the open courtyard. Hence, a higher prevalence as is seen in indoor air pollution, where cooking is done in closed rooms was not reported.
Past occupation and cooking had to be omitted from the multivariable model due to co-linearity in these two variables. Hence, their association with COPD could not be studied. Due to the rural setting of the study, association with passive tobacco exposure could not be studied, as most of the smokers used to smoke in the courtyard or outside the house.
The study was conducted in the winter months due to logistic reasons. Respiratory symptoms were likely to be more common during the study period.
In the absence of complete clinical data, other diseases with an obstructive pattern on spirometry such asthma or bronchiectasis may be misdiagnosed with COPD. However, since the symptoms were of late onset, one may conclude that it was less likely to be asthma. Hence, the chances of misdiagnosis were minimal.
During the study, X-ray and sputum examination was done on case-to-case basis wherever required for the management of patients. However, data regarding X-ray and sputum examination were not collected for this study.
Spirometry-based assessment and high proportion of acceptable spirometry results (87%) are some of the strengths of this study.
Overall, the identification of factors associated with COPD and appropriate measures can help in addressing the problem. Since the highest burden was seen among those aged 70 yr or more, increasing trend of ageing of the population is an important determinant of prevalence of COPD in the country. The prevention and management of chronic respiratory diseases including COPD should be emphasized in national health programmes for the elderly. Elderly patients with symptoms or risk factors should promptly be referred to a facility where spirometry can be done. Wherever feasible, facility for spirometry should be made available at the primary level. Smoking was another factor found to be strongly associated with COPD. For people who continue to smoke, counselling for smoking cessation may be useful.
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- 2020. Global alliance against chronic respiratory diseases:A world where all people breathe freely. Available from:https://www.Who.Int/gard/gard_sign_up/en/
- 2019. Chronic respiratory diseases (CRDs). Available from:http://www.who.int/entity/respiratory/en/index.html
- 2019. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease;2018 report. Available from:https://goldcopd.org/wpcontent/uploads/2017/11/GOLD-2018-v6.0-FINAL-revised-20-Nov_WMS.pdf
- The burden of chronic respiratory diseases and their heterogeneity across the states of India:The global burden of disease study 1990-2016. Lancet Glob Health. 2018;6:e1363-74.
- [Google Scholar]
- A review of population studies from India to estimate national burden of chronic obstructive pulmonary disease and its association with smoking. Indian J Chest Dis Allied Sci. 2001;43:139-47.
- [Google Scholar]
- Chronic obstructive pulmonary disease in the elderly:Evaluation and management. Asian J Gerontol Geriatr. 2013;8:90-7.
- [Google Scholar]
- 61st AIIMS Annual Report 2016-17. Available from:https://www.aiims.edu/en/about-us/annual-reports.html
- Indian study on epidemiology of asthma, respiratory symptoms and chronic bronchitis in adults (INSEARCH) Int J Tuberc Lung Dis. 2012;16:1270-7.
- [Google Scholar]
- Body mass index of the elderly derived from height and from armspan. Asia Pac J Clin Nutr. 1996;5:79-83.
- [Google Scholar]
- 2019. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease;2019. Available from:https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf
- Evaluation of the ERS'93 reference equations of Total Lung Capacity. Eur Respir J. 2018;52((Suppl 62)) OA3778
- [Google Scholar]
- Recommendations for a standardized pulmonary function report. An official American Thoracic Society technical statement. Am J Respir Crit Care Med. 2017;196:1463-72.
- [Google Scholar]
- Stata Statistical Software:Release 12. College Station, TX: StataCorp LP; 2011.
- Prevalence, risk factors and clinical correlates of COPD in a rural setting in Tanzania. Eur Respir J. 2018;51:1700182.
- [Google Scholar]
- Prevalence of chronic airflow limitation in Kashmir, North India:Results from the BOLD study. Int J Tuberc Lung Dis. 2016;20:1399-404.
- [Google Scholar]
- An epidemiological profile of chronic obstructive pulmonary disease:A community-based study in Delhi. J Postgrad Med. 2017;63:29-35.
- [Google Scholar]
- Prevalence of chronic respiratory disorders in a rural area of North West India:A population-based study. J Family Med Prim Care. 2016;5:416-9.
- [Google Scholar]
- The prevalence of chronic obstructive pulmonary disease by the global lung initiative equations in north-western Russia. Respiration. 2016;91:43-55.
- [Google Scholar]
- Prevalence of chronic obstructive pulmonary disease (COPD) in Qena Governorate. Egypt J Chest Dis Tuberc. 2016;65:29-34.
- [Google Scholar]
- Burden of obstructive lung disease study in Tehran:Prevalence and risk factors of chronic obstructive pulmonary disease. Lung India. 2015;32:572-7.
- [Google Scholar]
- The prevalence of chronic obstructive pulmonary disease in Riyadh, Saudi Arabia:A BOLD study. Int J Tuberc Lung Dis. 2015;19:1252-7.
- [Google Scholar]
- Prevalence of chronic obstructive pulmonary disease in Korea:A population-based spirometry survey. Am J Respir Crit Care Med. 2005;172:842-7.
- [Google Scholar]
- The association between BMI and COPD:The results of two population-based studies in Guangzhou, China. COPD. 2013;10:567-72.
- [Google Scholar]
- Chronic airflow limitation in a rural Indian population:Etiology and relationship to body mass index. Int J Chron Obstruct Pulmon Dis. 2011;6:543-9.
- [Google Scholar]
- Body mass index and its relation to GOLD stage in chronic obstructive pulmonary disease patients. Egypt J Chest Dis Tuberc. 2016;65:411-4.
- [Google Scholar]
- Influence of sex on chronic obstructive pulmonary disease risk and treatment outcomes. Int J Chron Obstruct Pulmon Dis. 2014;9:1145-54.
- [Google Scholar]
- Socioeconomic status and COPD among low- and middle-income countries. Int J Chron Obstruct Pulmon Dis. 2016;11:2497-507.
- [Google Scholar]
- Does educational level influence lung function decline (Doetinchem Cohort Study)? Eur Respir J. 2009;34:940-7.
- [Google Scholar]






