Translate this page into:
Perioperative antimicrobial therapy in preventing infectious complications following pancreatoduodenectomy
Reprint requests: Dr Adarsh Chaudhary, Department of Gastrointestinal Surgery, Gastrointestinal Oncology & Bariatric Surgery, Medanta Institute of Digestive & Hepatobiliary Sciences, Medanta - The Medicity, Sector 38, Gurgaon 122 001, Haryana, India e-mail: adarsh_chaudhary@yahoo.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Infectious complications have been reported to occur in up to 45 per cent of patients, following pancreatoduodenectomy (PD). The incidence of perioperative infectious and overall complications is higher in patients undergoing preoperative invasive endoscopic procedures. The aim of the study was to compare the role of a carbapenem administered as three-once daily perioperative doses on infectious complications in patients at high risk for these complications versus those at low risk.
Methods:
A retrospective study with some secondary data collected from records was carried out on the data from a prospectively maintained surgical database of patients undergoing PD for pancreatic and periampullary lesions at a tertiary referral care centre, between June 2011 and May 2013. Patients were divided into two groups for comparison based on whether they underwent at least one preoperative endoscopic interventional procedure before PD (high-risk - intervention and low-risk - no intervention). All patients were administered three-once daily doses of ertapenem (1 g).
Results:
A total of 135 patients in two groups were comparable in terms of demographic and nutritional, surgical and histopathological factors. No significant difference between the two groups in terms of the overall morbidity (38.7 vs 35.7%), infectious complications (9.7 vs 4.8%), mortality (2.2 vs 2.4%) and mean post-operative hospital stay (9.2 vs 8.9 days) was observed.
Interpretation & conclusions:
Perioperative three-day course of once-daily administered ertapenem resulted in a non-significant difference in infectious and overall complications in high-risk patients undergoing PD as compared to the low-risk group.
Keywords
Morbidity
mortality
outcomes
surgery
Pancreatoduodenectomy (PD), or the Whipple's operation, is a technically complex procedure with attendant risk of major morbidity and even mortality1. Infectious complications which have been reported to occur in as high as 45 per cent of patients following PD2 not only lead to increased costs and extended hospital stay but may also contribute to mortality34. Morbidity following PD performed for cancer patients is one of the factors responsible for the delay, or even the omission, of adjuvant chemotherapy5. Valle et al6 have demonstrated the importance of completion of chemotherapy on overall survival. Thus, it is imperative that the need for minimizing infectious complications [including surgical site infections (SSIs)], following PD be strongly considered.
Biliary colonization that may occur as a result of preoperative biliary drainage is a major predictor of infectious complications, following PD789. While the evidence to routinely support the up-front drainage of the biliary tree in patients with pancreatic cancer and periampullary tumours presenting with surgical obstructive jaundice is lacking10, such procedures are on the rise the world over11. Besides biliary intervention, the nutritional status12, surgical operative time13 and anastomotic leaks following PD, especially pancreatic14 and biliary, are amongst the common factors linked to the development of infectious complications following PD. Not always is it possible to dramatically improve the state of nutrition of the patient as delays in surgery may result in disease progression in cancer patients15. One common inference from literature in terms of reducing the risk of anastomotic complications is the performance of surgery in high-volume centres16171819. There is also evidence to suggest that the ability to regulate the performance of preoperative biliary procedures including stenting and other invasive endoscopic procedures is difficult even in well-organized health-care systems11 which leaves the surgeon with limited options in terms of reducing post-operative infectious complications following PD, the most readily available being the use of appropriate antimicrobial prophylaxis to reduce infectious complications.
The aim of the present study was to compare the role of a carbapenem (choice based on intraoperative cultures) administered as three-once daily perioperative doses on infectious complications in patients at high risk for these complications (those undergoing preoperative invasive endoscopic procedures) versus those who underwent up-front surgery (low-risk group).
Material & Methods
The data of 135 consecutive patients who underwent PD for pancreatic and periampullary lesions (benign and malignant) at the department of Gastrointestinal Surgery, Gastrointestinal Oncology and Bariatric Surgery, Medanta, The Medicity, Gurgaon, India, between June 2011 and May 2013 were obtained from a prospectively maintained database. The study was approved by the Institutional Review Board and the Ethics Committee of the Medanta, The Medicity (Approval No: MICR-346/2013).
The patients were divided into two groups based on whether they underwent at least one preoperative endoscopic procedure including sphincterotomy, brushing, biopsy, endoprosthesis or nasobiliary drain into high risk and low risk (no preoperative intervention). The sample size of 135 patients was determined to provide an overall estimate of morbidity (assumed as 40%) related to surgical outcome well within 10 per cent margin of error with 95 per cent confidence level.
Based on an analysis of 117 intraoperative bile cultures taken during PD, it was noted that the most common organisms found were Enterococcus (24%), Escherichia coli (20%) and Klebsiella sp. (11%). Other less frequently encountered organisms included Pseudomonas and Enterobacter sp. (3% each). Isolated cases of Aeromonas sp., Morganella sp., Streptococcus sanguis, Shewanella sp. and Acinetobacter sp. were also detected. Positive bile cultures in our centre have been noted in 64 per cent patients who have undergone a preoperative invasive procedure and 18 per cent of patients undergoing up-front surgery.
The use of cephem or carbapenems has been advised to prevent post-operative infections20. Carbapenems also cover anaerobes in their bacterial spectrum and are especially preferred in pancreatic diseases21. Ertapenem, a carbapenem like imipenem and meropenem, demonstrates broad-spectrum antimicrobial activity against many Gram-positive and Gram-negative aerobes and anaerobes and is resistant to nearly all β-lactamases, including extended-spectrum β-lactamases and AmpCs. The extensive protein binding of ertapenem extends the half-life and allows for once-daily dosing22. Even in the experimental setting, ertapenem has been shown to be as effective as meropenem in pancreatitis (murine) models23.
Based on this, all the 135 patients were administered three-once daily doses of ertapenem (1 g) as follows: within one hour before induction and on day one and day two following surgery. Antibiotics were then ceased following post-operative day two until discharge. Therapeutic use of antimicrobials was considered in patients who thereafter developed infectious complications based on the site of infection and appropriate culture and sensitivity report. This was encountered in 47 patients (35%). In 11 patients, ertapenem itself was continued for an average of three additional days, and in 36 patients, other antibiotics were used.
Perioperative management: The post-PD clinical pathway for post-operative care followed in our unit has been previously published24. All patients underwent a classical PD, after an overnight fast, via a right subcostal incision with the following reconstruction: pancreaticojejunostomy - end-to-side, duct to mucosa in two layers; hepaticojejunostomy - end-to-side; gastrojejunostomy - side-to-side, retrocolic, retrogastric. In patients in whom the pancreatic duct was not visualized, an end-to-side pancreaticojejunostomy was performed. A standard lymphadenectomy was performed in all patients. The decision on whether or not to place a single drain (32 Fr Portex drain in the Morisson's pouch) intraoperatively was made on a case-to-case basis.
Definition of complications: For the study, infectious complications were defined as SSIs and/or intra-abdominal collections or respiratory infective complications associated with signs of sepsis (transient or prolonged) including fever, elevated leucocytosis and the need for re-initiation of antibiotics. Post-operative pancreatic anastomotic leak/post-operative pancreatic fistula (POPF), delayed gastric emptying (DGE), bile leak and post-pancreatectomy haemorrhage (PPH) were defined as per the International Study Group of Pancreatic Surgery criteria252627. Mortality was defined as any death that has occurred not only in the 30 days following surgery but even thereafter so long as there existed sufficient evidence to link the cause of death to the surgery or its complications. Any re-admissions within 30 days of discharge were recorded.
Statistical analysis: The analysis included profiling of patients on different demographic and clinical as well as treatment outcome parameters. Descriptive statistics of quantitative variables are expressed as means and standard deviation. Ordinal/categorical data are expressed in terms of proportions and percentages. The assessment of normality of data was tested using the Kolmogorov–Smirnov test. For the comparison of means between groups, independent Student's t test was performed. Standard normal deviate test (Z-test) and Chi-square test were used for the qualitative variables. All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) Inc., IBM, USA, Version 18.0 for Windows.
Results
There were 97 males and 38 females with a median age of 58 yr (range: 15-80 yr), median body mass index (BMI) of 24.4 kg/m2 (range: 12.5-41.5 kg/m2) and median serum albumin level of 3.5 g per cent (range: 1.4-5 g %). The comparative demographic data of the 135 patients in the two groups are presented in Table I. There were a total of 93 and 42 patients in the high- and low-risk groups, respectively. No significant difference in the parameters was noted between the two groups.
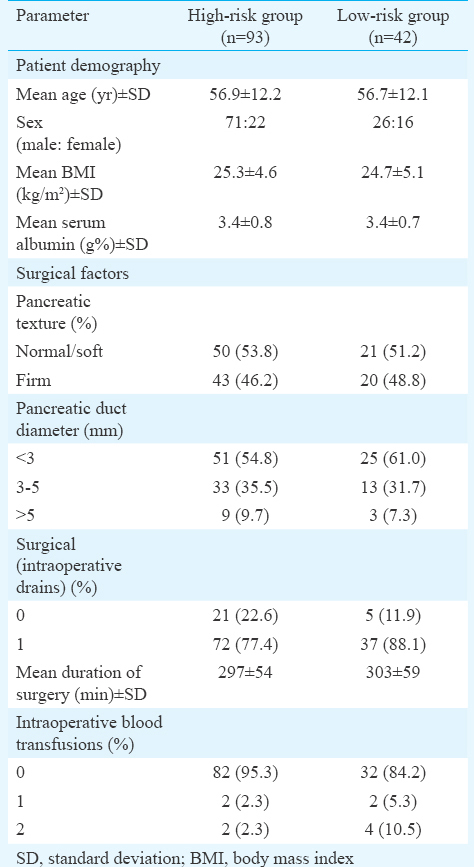
Surgery-related factors: All patients underwent a classical Whipple's procedure with a median duration of 293 min (range: 205-480 min). Surgical factors such as pancreatic texture, duct size, use of drains, intraoperative blood transfusions and duration of surgery were compared (Table I). There was no significant difference between the two groups with regards to these parameters.
Pathological factors: Table II lists the histopathological features in the two patient groups. There was no significant difference between the two groups with regards to these parameters.

Surgical outcomes: The overall morbidity and mortality rates for all patients were 36.9 and 2.2 per cent with infectious complications noted in 11 patients (8.1%). Two patients in the high-risk group developed POPF (Grade B and C) and one patient in the low-risk group developed POPF (Grade A). All three patients required percutaneous pigtail catheter insertions by the interventional radiology team. In addition, the patient with the Grade B POPF developed PPH necessitating an embolization of the gastroduodenal artery. Despite all intensive measures, the patient developed multiple organ dysfunction syndrome and succumbed. There were three patients with wound infections, five patients with intra-abdominal collections and one patient with an infective respiratory complication in the high-risk group and one patient each with a wound infection and collection (who also developed an infective respiratory complication) in the low-risk group.
Table III provides a comparison between the two groups with regard to post-operative outcomes such as overall complications, infectious complications, mortality and hospital stay. No significant difference was noted in these variables between the two groups.

Discussion
The present data indicated that the rate of overall as well as infectious complications in high-risk patients undergoing PD was no different from the low-risk group using a standardized, perioperative antimicrobial prophylaxis of ertapenem administered as three-once daily perioperative dosages.
PD remains a technically demanding procedure with a high propensity for complications. While the surgical complications of POPF, DGE and PPH remain the most described, infectious complications occur independently, or as a result of POPF14, in as many as 45 per cent of patients2. Thus, while the focus of the surgical fraternity is justified on the technical aspect of the surgery, it is also important to direct attention to the role of antimicrobial prophylaxis in this surgery. The main reasons for this is: the number of patients undergoing preoperative biliary drainage is increasing11 despite the fact that it is not routinely indicated10.
Biliary colonization is a direct off shoot of this practice (as has been noted in this study and by others7) with a large number of patients going on to develop complications such as cholangitis and acute pancreatitis. These have been shown to influence the incidence of surgical complications92829. Surgical morbidity is associated with increased medical costs and even the risk of mortality. In patients with cancers, complications may additionally result in delays in commencing chemotherapy or even completion of chemotherapy5, thereby jeopardizing survival. Thus, it is imperative that every effort must be made to reduce the incidence of complications following PD.
The present study attempted to analyze the impact of a simple antimicrobial perioperative prophylaxis strategy [three-once daily doses of ertapenem (1 g)] in patients undergoing PD by comparing the outcomes of the intervention in two groups of patients who were comparable in terms of demographic and nutritional (age, sex, BMI and serum albumin levels), surgical (pancreatic duct size and texture, intraoperative blood transfusions and duration of surgery) and histopathological (benign and malignant disease) factors, some of which are known to affect outcomes (including infectious complications) and differing in only a single variable - preoperative invasive endoscopic intervention. There was no significant difference between the two groups in terms of the overall morbidity, infectious complications, mortality and post-operative hospital stay.
Sourrouille et al7 noted that a five-day course of antimicrobial prophylaxis was effective in reducing infectious complications in patients who were high risk and underwent PD. While they excluded patients without malignancies, we included patients with benign diseases as infectious complications following PD occur irrespective of the underlying pathology. The equal distribution of benign malignant pathologies in our study (P=0.423) negated any potential bias of malignancy having a poor influence on the incidence of infectious complications in either of the two groups30. One of the intriguing findings noted in the study was the 18 per cent positive isolation of organisms from intraoperative bile culture even in those patients who had not undergone any prior invasive procedure. This has also been noted by Sourrouille et al7 in 12 per cent of low-risk patients. Although this rate, noted in our study, was significantly lower than the 64 per cent in the high-risk group, it still supports the routine use of antimicrobial prophylaxis in PD31.
The limitations of our study were related to its inherent retrospective nature. A way forward would certainly be to conduct prospective randomized controlled trials to further explore/validate these findings. This would help clarify the role of perioperative antimicrobial prophylaxis with three-dose ertapenem in patients undergoing PD.
In conclusion, perioperative three-day course of once daily administered ertapenem resulted in a non-significant difference in infectious and overall complications in high-risk (preoperative endoscopic intervention) patients undergoing PD as compared to the low-risk (up-front surgery) group. Based on the results of this study it is not possible to comment on the causal role of the antibiotic coverage on reducing the complications in the high-risk group as this was only an observational study.
Acknowledgment
This study was awarded an Investigator Initiated Study grant by Merck Sharp & Dohme (MSD Regional Office, India).
Conflicts of Interest: None.
References
- Increased plasma levels of IL-6 and IL-8 are associated with surgical site infection after pancreaticoduodenectomy. Pancreas. 2006;32:178-85.
- [Google Scholar]
- Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20:250-78.
- [Google Scholar]
- Continuous, 10-year wound infection surveillance. Results, advantages, and unanswered questions. Arch Surg. 1990;125:794-803.
- [Google Scholar]
- Postoperative complications reduce adjuvant chemotherapy use in resectable pancreatic cancer. Ann Surg. 2014;260:372-7.
- [Google Scholar]
- Optimal duration and timing of adjuvant chemotherapy after definitive surgery for ductal adenocarcinoma of the pancreas: Ongoing lessons from the ESPAC-3 study. J Clin Oncol. 2014;32:504-12.
- [Google Scholar]
- Five days of postoperative antimicrobial therapy decreases infectious complications following pancreaticoduodenectomy in patients at risk for bile contamination. HPB (Oxford). 2013;15:473-80.
- [Google Scholar]
- Is bactibilia a predictor of poor outcome of pancreaticoduodenectomy? Hepatobiliary Pancreat Dis Int. 2010;9:65-8.
- [Google Scholar]
- Pre-operative stenting is associated with a higher prevalence of post-operative complications following pancreatoduodenectomy. Int J Surg. 2011;9:145-9.
- [Google Scholar]
- The current status of preoperative biliary drainage for patients who receive pancreaticoduodenectomy for periampullary carcinoma: A comprehensive review. Surgeon. 2014;12:290-6.
- [Google Scholar]
- Current trends in preoperative biliary stenting in patients with pancreatic cancer. Surgery. 2013;154:179-89.
- [Google Scholar]
- Nutritional risk index as an independent predictive factor for the development of surgical site infection after pancreaticoduodenectomy. Surg Today. 2013;43:276-83.
- [Google Scholar]
- Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999;27:97-132.
- [Google Scholar]
- Risk factor of surgical site infection after pancreaticoduodenectomy. World J Surg. 2012;36:2888-94.
- [Google Scholar]
- Preoperative immunonutrition in patients at nutritional risk: Results of a double-blinded randomized clinical trial. Eur J Clin Nutr. 2012;66:850-5.
- [Google Scholar]
- Effect of centralization of pancreaticoduodenectomy on nationwide hospital mortality and length of stay. Br J Surg. 2007;94:1377-81.
- [Google Scholar]
- Peri-operative outcomes for pancreatoduodenectomy in India: A multi-centric study. HPB (Oxford). 2009;11:638-44.
- [Google Scholar]
- Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117-27.
- [Google Scholar]
- Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128-37.
- [Google Scholar]
- Guidelines for adequate antibiotic prophylaxis after hepatic, biliary, and pancreatic surgery. Nihon Geka Gakkai Zasshi. 2001;102:851-5.
- [Google Scholar]
- The role of antibiotics in the management of patients with acute necrotizing pancreatitis. Curr Infect Dis Rep. 2010;12:13-8.
- [Google Scholar]
- Effect of early antibiotic prophylaxis with ertapenem and meropenem in experimental acute pancreatitis in rats. J Hepatobiliary Pancreat Surg. 2009;16:328-32.
- [Google Scholar]
- Early discharge after pancreatoduodenectomy: What helps and what prevents? Pancreas. 2015;44:273-8.
- [Google Scholar]
- Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS) Surgery. 2007;142:761-8.
- [Google Scholar]
- Postpancreatectomy hemorrhage (PPH): An International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142:20-5.
- [Google Scholar]
- International Study Group on Pancreatic Fistula Definition. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8-13.
- [Google Scholar]
- Clinical impact of preoperative cholangitis after biliary drainage in patients who undergo pancreaticoduodenectomy on postoperative pancreatic fistula. Am Surg. 2014;80:36-42.
- [Google Scholar]
- Preoperative biliary drainage for distal biliary obstruction and post-operative infectious complications. ANZ J Surg. 2013;83:280-6.
- [Google Scholar]
- Identification of risk factors by systematic review and development of risk-adjusted models for surgical site infection. Health Technol Assess. 2011;15:1.
- [Google Scholar]
- Current antibiotic prophylaxis in pancreatoduodenectomy in Japan. J Hepatobiliary Pancreat Surg. 2005;12:304-9.
- [Google Scholar]






