Translate this page into:
National Iodine Deficiency Disorders Control Programme: Current status & future strategy
For correspondence: Dr Kapil Yadav, Centre for Community Medicine, All India Institute of Medical Sciences, New Delhi 110 029, India e-mail: dr.kapilyadav@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Iodine deficiency disorders (IDDs) constitute a significant public health problem globally. In India, the entire population is prone to IDDs due to deficiency of iodine in the soil of the sub-continent and thus both animal and plant source food grown on the iodine-deficient soil. IDDs encompass the spectrum of disability and disease and include goitre, cretinism, hypothyroidism, abortion, stillbirth, brain damage, learning disabilities, mental retardation, psychomotor defects, hearing and speech impairment. Iodine deficiency is known to be the single largest cause of preventable brain damage. IDDs with their causal association with brain development, cognition, and learning disabilities impair the human resource development and progress of the country. The children born in iodine-deficient regions on an average have 13.5 intelligence quotient (IQ) points lesser than children born in iodine-sufficient regions. IDD control programme in India is a public health success story, with 92 per cent of the population consuming iodized salt. The partnership between government agencies, academic institutions, salt industry, development agencies and civil society has been key to achieve this success story. The sustainable elimination of iodine deficiency in India is within reach, what is required is accelerated and coordinated effort by all key stakeholder at national and State level.
Keywords
ICCIDD
iodine deficiency disorder
iodized salt
last mile
public health nutrition
success story
way forward
Introduction
Iodine is a trace mineral required for optimal mental and physical development and is a key constituent of thyroid hormones. Iodine deficiency is the single largest cause of preventable brain damage globally1. Iodine deficiency disorders (IDDs) include goitre, cretinism, hypothyroidism, abortion, stillbirth, brain damage, learning disabilities, mental retardation, psychomotor defects, hearing and speech impairment2. Rapidly changing environmental conditions leading to melting of glaciers, frequent floods, change of river beds and loss of forest cover have led to depletion of the iodine from the top layers of the soil3. The resultant low iodine content of soil leads to low iodine in livestock and vegetation dependent on these soil and also in humans consuming these live stocks and vegetations. Historically, iodine deficiency was causally associated to only goitre and cretinism4. Research over the past three decades has shown that iodine deficiency has a significantly wider spectrum, affecting all the age groups from intrauterine period to adult life with serious impact on the brain of developing child and also manifests a myriad of health and social problems567.
It has been shown that even mild iodine deficiency during pregnancy has irreversible effects on foetal neurodevelopment and consequent cognition and learning abilities of the young child8910. The children born in iodine-deficient regions on an average have 13.5 intelligence quotient (IQ) points lesser than children born in iodine sufficient regions11. IDD with its causal association with brain development, cognition, learning disabilities impairs the human resource development (HRD) and progress of the country1213. It has been estimated that one point increase in a nations’ average IQ is associated with 0.11 per cent annual increase in gross domestic product (GDP), thus IDD elimination can potentially contribute to 1.5 per cent GDP growth annually14. Nearly all the short- and long-term consequences of IDDs are irreversible with the majority of them being difficult to recognise15. However, with appropriate interventions in place, all the adverse effects of IDD are totally preventable16. Globally, 1.8 billion people are at risk of iodine deficiency due to insufficient dietary iodine intake17. The Indian population is prone to IDDs due to deficiency of iodine in the soil and thus both animal and plant source food grown on the iodine-deficient soil1418. Universal Salt Iodization (USI) has been recognized as a key strategy for control of IDD. In 1994, the World Health Organization (WHO) and the United Nations Children's Fund (UNICEF) Joint Committee on Health Policy recognized USI as a safe, cost-effective and sustainable strategy to ensure sufficient intake of iodine by all individuals19. Salt iodization, which costs less than ₹0.2 per person per year20 and has been rated as one of the most cost-effective development interventions (ratio of 1:81) by Copenhagen Consensus Statement 200821 and subsequently again in 201222.
India has made impressive progress in control of IDDs with successful adoption and scaling up of USI in the country. According to National Iodine and Salt Intake (NISI) survey, 2014-2015, currently, 78 per cent of households in India are consuming adequately iodized salt23. However, still significant percentage of the population continues to consume inadequately iodized salt (14%) or nil iodine salt (8%). There is a need to reach the unreached population and cover the ‘last mile’ of USI success story of India. This calls for developing and implementing the ‘end game strategy’ to accelerate, achieve and sustain the elimination of IDD in India.
Iodine deficiency disorder (IDD) control programme in India: A successful public health programme
IDD control programme in India has been a public health success story. We are within the grasping reach of the target of >90 per cent household level coverage of adequately iodized salt of USI. India has been at the forefront of global efforts by contributing to research and programme for the elimination of IDD. The National Goitre Control Programme (NGCP) was one of the earliest national programmes dedicated to the elimination of IDD launched in year 196224. The successful evolution of IDD control programme in India highlights factors for successful and sustainable implementation of a health programme and has lot of learning's for other health and nutrition programmes in the country in particular and other programmes related to social sector in general. The experience and lessons learned can be generalized to other countries as well.
Salt iodization was first used as an intervention strategy to present goitre in the United States of America and Switzerland in 1920s25. The landmark study in the Kangra valley in Himachal Pradesh from 1956 to 1972 successfully demonstrated the effectiveness of salt iodization in reducing goitre rates2627. The Kangra Valley Study led to the establishment of NGCP in India in 1962 even before the study was concluded in 197228. Providing iodized salt in the endemic areas through iodine subsidy was the key strategy for control of goitre under this Programme. Focus of the NGCP was on endemic districts. In the first decade or so of the Programme only 12 salt iodization plants were established in public sector, with annual production of only two lakh tons, which was able to cater to only 15 per cent of the total requirement of iodized salt. NGCP remained a low priority health programme as goitre was perceived to be a mild cosmetic problem that too restricted to the Himalayan region.
New scientific evidence emerged from India and other countries showed a significant impact of iodine deficiency on early brain development, cognition and learning abilities of children29. The whole country was shown to be endemic for IDD and very high prevalence of neonatal hypothyroidism was reported from some parts in the country7. In 1983 in the Meeting of Central Council of Health, policy decision to ensure USI in the whole of the country by the year 1992 was taken and to facilitate the availability of required amount of iodized salt, private sector was allowed to set up salt iodization plants30. Programme was expanded and renamed as National IDDs Control Programme (NIDDCP) in the same year taking into account recent evidence establishing public health significance of IDDs31. Due to advocacy by public health experts, the Government of India decided to make salt iodization mandatory for direct human consumption. In 1997, the ban on non-iodized salt was brought under the ambit of Prevention of Food Adulteration (PFA) Act, 1954 and was implemented in all parts of the country32. Concurrently, due to expansion and modernization of salt industry, there was an increase in the production of iodized salt from two lakh tons in 1986 to 44 lakh tons in 200033. There was an increase in household coverage of iodized salt with 49 per cent households consuming adequately iodized salt (15 parts per million)34.
The ban on sale of non-iodized salt in India was lifted in 2000 by the then National Democratic Alliance government due to a campaign by a few nationalist groups35. The factors responsible for lifting of the ban were higher price of iodized salt as compared to non-iodized salt; perception that IDD affects only a small proportion of the population; penalties and court cases faced by salt producers under PFA Act due to inadequate iodization, perception of association of salt iodization with multinational aid agencies and companies and question of individuals right to choose type of salt to consume. The lifting of ban resulted in decline in iodized salt production to 41 lakh tons in 2003 and resulted in a drop in the household coverage of iodized salt to 30 per cent in 2002-200336. In the third round of the National Family Health Survey (NFHS) conducted in 2005-2006, household coverage with adequately iodized salt increased to 51 per cent37.
The lifting of ban and subsequent decline in household coverage with adequately iodized salt forced the scientific community in generating scientifically valid information to counteract the propaganda against iodized salt and establish criticality of IDD problem in India. IDD survey conducted by the International Council for Control of IDD (ICCIDD) in seven States spread across geography of the country in 2000-2006 established that IDD was a significant public health problem7. Intense advocacy campaign was undertaken using the results of these surveys and also global experiences to address the claims made against the salt iodization. After a prolonged campaign by the scientist community of India, the ban on non-iodized salt was reinstated in 200538. However, the opposition to a mandatory ban on non-iodized salt continued, and in 2011 in wake of Public Interest Litigation, the Supreme Court of India constituted a committee to review the scientific basis of mandatory salt iodization for control of IDD39. The committee comprising of leading public health experts of India, upheld the relevant salt iodization regulations under the Food Safety and Standards Act, 200640.
The Core Advisory Group on Public Health and Human Rights of National Human Rights Commission examined the public health consequence of lifting of ban on mandatory salt iodization in 2004. The Group recommended that IDD continued to be of public health significance in India and the USI was needed to be mandatorily implemented throughout the country41. The ban on sale of non-iodized salt was reinstated in 2005 by the Government of India pursuant to the recommendation of the Group.
Partnerships amongst key stakeholders for sustained advocacy and promoting sustained elimination of IDD
The National Coalition for Sustained Optimal Iodine Intake (NCSOII) was established in 2006 with partnership from government agencies, Salt Commissioner of India, academic institutions, salt producers and traders, bilateral and multilateral development agencies and civil society42. Small and medium scale salt producers were targeted for strengthening of capacity to establish quality assurance of laboratory monitoring thus improving the quality of iodized salt43. Innovative business models including providing iodized salt in Public Distribution System through salt traders groups were implemented to increase coverage with iodized salt. The multipronged approach of strengthening supply and demand side intervention led to an increase in the household coverage of adequately iodized salt in the country44. The iodized salt production was also increased to 6.2 million tons thus meeting the total iodized salt requirement of the country. According to NISI survey, 2014-2015, currently, 78 per cent of households in India are consuming adequately iodized salt45. There has been encouraging trend of sustained improvement in salt iodization coverage over the last decade (Fig. 1)142638. However, significant percentage of the population continues to consume inadequately iodized salt (14%) or nil iodine salt (8%)45.
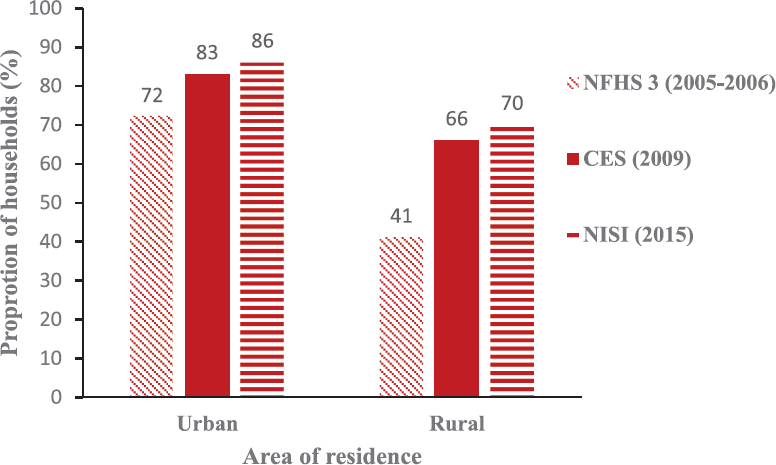
- Trends in use of adequately iodized salt use at national level across urban and rural areas. NFHS 3, National Family Health Survey 3; CES, Coverage Evaluation Survey; NISI, National Iodine and Salt Intake Survey, 2015.
-
Source: Refs 14, 26, 38.
Key milestones in journey of IDD control in India
The results of recently concluded surveys have shown significant sub-national differentials in iodized salt coverage. NISI Survey 2014-201523 reported IDD status in India desegregated by geographical zones, rural-urban areas and socio-economic status. There was 17 percentage point differential across urban and rural population and 10 percentage point differential across deprived and non-deprived households (Fig. 2). The south zone (adequately iodized salt coverage only 62%) of India comprising of States of Andhra Pradesh, Karnataka, Kerala, Tamil Nadu and Telangana continues to have below national level coverage of adequately iodized salt.
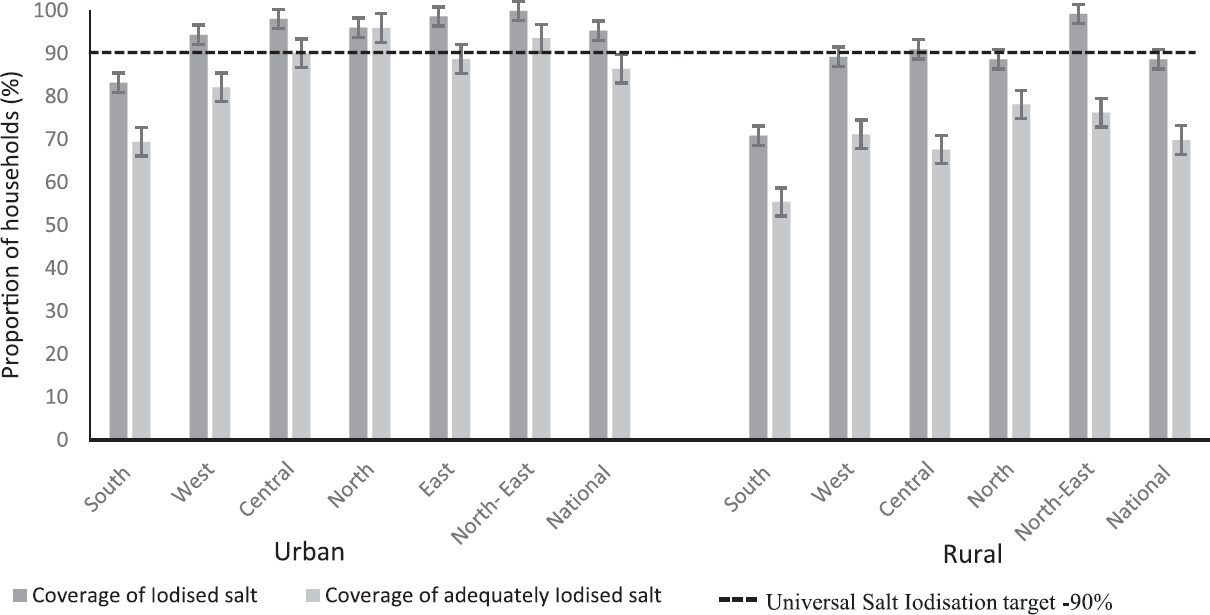
- National and sub-national iodized salt coverage in urban and rural strata. Source: Ref. 23.
The journey of salt iodization programme in India can be broadly classified into the following phases: (i) Phase 1: Scientific research leading to programme (1956-1983); (ii) Phase 2: From goitre to IDD (1983-2000); (iii) Phase 3: Lifting the ban on sale of non-iodized salt (2000-2005); and (iv) Phase 4: Reinstatement of ban on sale of non-iodized salt and consolidation of sustainable elimination of IDD (Since 2005).
The critical factors for the achievement of success of IDD control programme in India were as follows: (i) Generation of regular, representative and reliable scientific data - Regular, representative and reliable data at the State and national level are required for the development of effective and efficient policy and programmes and effective advocacy. From Kangra Valley study (1956-1972)26 to NISI Survey (2014-2015)23 generation of evidence has been an iterative process in India and provided inputs for the policy and programme. (ii) Stakeholder analysis and development of partnership - the development of partnership between various stakeholders namely government institutions, academic institutions, international and national non-governmental organization, civil society organization and salt producers helped in sustainability in efforts towards achieving USI and elimination of IDD. (iii) Institutional continuity and mentorship for the achievement of sustainability - Active involvement of All India Institute of Medical Sciences, New Delhi, in IDD control programme provided institutional continuity and allowed mentorship for generations of researchers and workers in the field of IDD. (iv) Addressing the value system of stakeholders - Neglect by the policymakers leads to serious setback to the programme implementation as seen in case of NIDDCP46. Addressing these issues through sustained advocacy led to lifting of ban on non-iodized salt and improvement in household coverage with adequately iodized salt. (v) Legislation for achieving public health goals - The PFA Act 1954 and its successor, the Food Safety and Standards Act 2006; which prevents the sale of non-iodized salt for human consumption, were instrumental in creating enabling environment for the achievement of USI in India. (vi) The involvement of private sector in public health efforts - Cooperation from salt industry was one of the main factors in achieving high coverage with adequately iodized salt. Engagement with medium and small-scale salt producers and focus on improvement in quality of iodized salt through maintenance of quality assurance has been one of the prime reasons for improved household coverage with adequately iodized salt.
Future strategy for achieving sustainable elimination of IDD in India
To accelerate the progress towards sustainable elimination of IDD in the country, there is a need to invigorate the efforts at national and State level from production to consumer level. There is a need to reposition the NIDDCP by linking elimination of IDD to HRD of the country. The social process model47 based on four main components, Demand for Iodized Salt (Pull), Supply of Iodized Salt (Push), Regular Reliable Representative State Level Scientific Data and Data for Decision Makers and Sustained Political Commitment needs to be followed (Fig. 3).
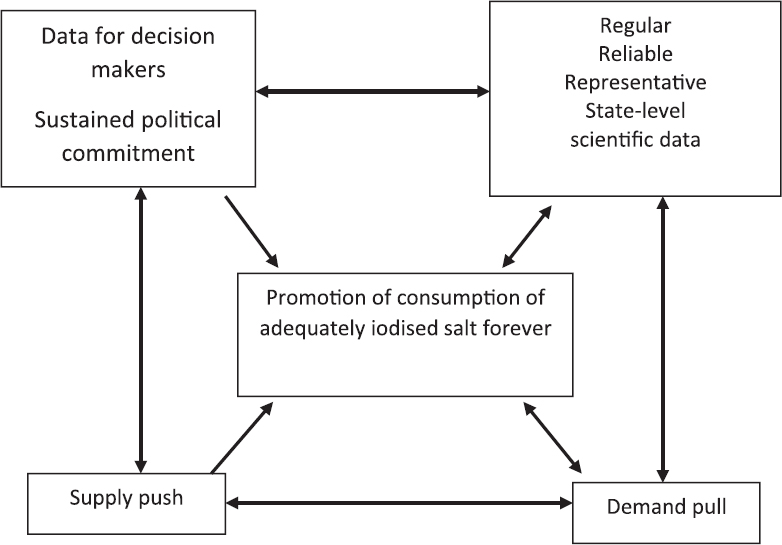
- The multi-component model for Iodine Deficiency Disorder Control Programme.
-
Source: Ref. 20.
There is a need for renewed focus and vigour to achieve USI in the country by developing strategy to target and engage small-scale producer/difficult to reach areas/marginalized population and strengthen monitoring of iodine content of salt from production to consumer level. There is also a need to establish national and State level coalitions for sustained optimal iodine intake comprising key stakeholders which include government policymakers, salt industry representatives, civil society, consumer organizations and national and international development agencies working for IDD elimination in India.
There has been long-standing demand to revise the technical guidelines of NIDDCP in line with the maturity of the national iodine elimination programme. The district-based approach of the periodic IDD survey guidelines should be revamped to focus on generating meaningful epidemiological data which can guide programme and policy. The regulatory framework to ensure stringent implementation of mandatory salt iodization needs to be strengthened. The Food Safety and Standards Act (FSSA) at the national level should issue guidelines and advisory for mandatory salt iodization. At the State level, adequate resources including workforce need to be allocated to salt iodization regulation and use of Management Information System (MIS) for monitoring of salt iodization from production to consumer level. Consolidation, modernization and mechanization of salt industry have been an essential component of the successful progress towards USI and policy changes should be made to enable this to continue, to improve access to adequately iodized salt for all sub-national population groups.
Strong government leadership and coordination amongst all stakeholders, which has been a cornerstone of the success, should be maintained. The success of the NCSOII and State USI coalitions in Bihar, Gujarat, Rajasthan and Uttar Pradesh highlights key the role of all stakeholders in USI. These partnerships should be sustained, strengthened and most importantly replicated in other States as well. The initial stages of formation of district USI coalitions in 12 leading salt producing districts of the country (accounting for 90% iodized salt production) should also be accelerated. There is a need to consolidate, modernize and mechanize salt industry particularly iodized salt industry to ensure availability of good quality, affordable, quality adequately iodized salt across India.
Strengthening quality assurance of salt iodization at production level
Experience across the globe and in India has shown that strengthening quality assurance of salt iodization at the point of production is the most efficient way to achieve and sustain USI. There is a need to strengthen quality assurance at production facilities in India particularly in southern States. The provision of FSSA, 200538, regarding mandatory iodization of all edible salt needs to be implemented with zero tolerance. The significant augmentation of infrastructure and human resource under the Act needs to be optimally harnessed to ensure stringent implementation of the salt iodization provision. The success achieved in special campaigns on salt iodization by a few States in India (UP, Bihar and Gujarat)4849 needs to be replicated in other States of the country.
The non-availability of quality affordable salt due to supply chain bottlenecks is responsible for the zonal difference in the iodized salt coverage. Reforms in iodized salt transportation policy are required to facilitate the availability of quality, affordable iodized salt in all regions of the country. A behaviour change communication (BCC) strategy focussing on promoting awareness regarding the linkage between iodine nutrition and iodized salt needs to be developed and implemented. The 2014-2015 national survey highlighted the differentials across zones, rural-urban and socio-economic strata in iodized salt coverage50. There is a need to conduct sub-national and State level USI surveys to build on this new evidence base to further understand determinants of these differentials and develop a strategy to address them. Existing network of quantitative estimation of iodine content of salt needs to be strengthened. These include the Salt Commissioner Office Laboratory and Salt producer's laboratories at production end and FSSA and State IDD cell at the consumer end. The novel experiment to establish laboratories for quantitative analysis of salt iodine level by salt traders and in State medical colleges (USI laboratories in UP and Bihar) should be replicated in other States of the country. Although the survey was not powered to estimate the iodine intake of pregnant women, the findings of the survey provided an indication of sub-optimal iodine status among pregnant women23. There is a need to undertake research on ascertaining iodine intake in pregnant women in India and to develop appropriate strategies to ensure achieving optimal iodine nutrition amongst pregnant women.
Production and distribution of good quality iodized salt are critical determinants for universal coverage of adequately iodized salt. Only three States of India account for more than 90 per cent of the iodized salt production and in these three States 10 districts account for more than 95 per cent of iodized salt production51. Iodized salt from these salts producing areas is transported by rail or roadways depending upon several factors.
Conclusion
The elimination of IDD is eminently possible. We are at a turning point in our battle against the ancient and pervasive scourge of iodine deficiency. IDD control programme in India is one of the success stories of public health in India. The current 92 per cent household level coverage of iodized salt in India, of which 78 per cent is adequately iodized salt, is a huge achievement. USI programme in India is in critical phase, and its success needs to be sustained to prevent slip backs. Government and all partner agencies are striving to develop an ‘end game strategy’ to cover the last mile towards achieving USI. Achieving sustainable elimination of the IDD would require coordinated effort; what is required now is mission approach with effective and efficient coordination amongst all stakeholders of IDD control efforts in India. With accelerated and coordinated efforts it would be possible to achieve the IDD control goal in the near future and sustain it thereafter.
Acknowledgment: Authors acknowledge valuable contribution by Salt Commissioner's Office, Government of India and Nutrition and IDD Cell, Ministry of Health and Family Welfare, Government of India, New Delhi, for facilitating the development of this manuscript. Also, due acknowledgements to research staff and support staff of ICCIDD for providing secretarial help in drafting of the manuscript.
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- ICCIDD, UNICEF, WHO. In: Assessment of iodine deficiency disorders and monitoring their elimination: A guide for programme managers (3rd ed). Geneva: World Health Organization; 2007.
- [Google Scholar]
- International Council for the Control of Iodine Deficiency Disorders. In: Towards the global elimination of brain damage due to iodine deficiency: A global program for human development with a model applicable to a variety of health, social and environmental problems. New Delhi: Oxford University Press; 2004.
- [Google Scholar]
- Intellectual assessment of school children from severely iodine deficient villages. Indian Pediatr. 1987;24:467-73.
- [Google Scholar]
- Developmental lag in preschool children of goitrous mothers. Indian Pediatr. 1983;20:259-63.
- [Google Scholar]
- Iodine deficiency and neonatal hypothyroidism. Bull World Health Organ. 1986;64:547-51.
- [Google Scholar]
- Iodine supplementation improves cognition in mildly iodine-deficient children. Am J Clin Nutr. 2009;90:1264-71.
- [Google Scholar]
- Effect of inadequate iodine status in UK pregnant women on cognitive outcomes in their children: Results from the Avon Longitudinal Study of Parents and Children (ALSPAC) Lancet. 2013;382:331-7.
- [Google Scholar]
- The adverse effects of mild-to-moderate iodine deficiency during pregnancy and childhood: A review. Thyroid. 2007;17:829-35.
- [Google Scholar]
- A meta-analysis of research on iodine and its relationship to cognitive development. The damaged brain of iodine deficiency -Cognitive behavioral, neuromotor, educative aspects 1994:195-200.
- [Google Scholar]
- Evidence-based interventions for improvement of maternal and child nutrition: What can be done and at what cost? Lancet. 2013;382:452-77.
- [Google Scholar]
- Micronutrient Initiative. In: Investing in the future: A united call to action on vitamin and mineral deficiencies: Global report 2009. New Delhi: Micronutrient Initiative; 2009.
- [Google Scholar]
- Iodine deficiency disorders (IDD) control in India. Indian J Med Res. 2013;138:418-33.
- [Google Scholar]
- Global iodine status in 2011 and trends over the past decade. J Nutr. 2012;142:744-50.
- [Google Scholar]
- Biomarkers of nutrition for development-iodine review. J Nutr. 2014;144((8)):1322S-1342S.
- [Google Scholar]
- UNICEF, WHO. In: World summit for children-mid decade goal: Iodine deficiency Disorders. UNICEF-WHO joint committee on health policy. Geneva: United Nations Children's Fund, World Health Organization; 1994.
- [Google Scholar]
- Salt for Freedom and Iodized Salt for Freedom from Preventable Brain Damage 2012
- The challenge of hunger and malnutrition. 2008. Copenhagen Consensus. Available from: https://www.copenhagenconsensus.com/sites/default/files/CP_Malnutrition_and_Hunger_-_Horton.pdf
- [Google Scholar]
- Challenge paper: Hunger and malnutrition. 2012. Copenhagen consensus centre. Coenhagen. Available from: https://www.copenhagenconsensus.com/sites/default/files/hungerandmalnutrition.pdf
- [Google Scholar]
- High national and sub-national coverage of iodised salt in India: Evidence from the first national iodine and salt intake survey (NISI) 2014-2015. Public Health Nutr. 2018;21:3027-36.
- [Google Scholar]
- Department of Health and Family Welfare. In: Annual report 2016-2017. New Delhi: Ministry of Health and Family Welfare, Government of India; 2017.
- [Google Scholar]
- History of the prevention of endemic goitre. Bull World Health Organ. 1953;9:241-8.
- [Google Scholar]
- Preliminary report of an experiment in the Kangra valley for the prevention of Himalayan endemic goitre with iodized salt. Bull World Health Organ. 1965;32:299-315.
- [Google Scholar]
- Prevention of endemic goitre with iodized salt. Bull World Health Organ. 1973;49:307-12.
- [Google Scholar]
- Iodine deficiency disorders in India: Review of control measures. Indian Pediatr. 1986;23:325-9.
- [Google Scholar]
- The effects of iodine on intelligence in children: A meta-analysis of studies conducted in China. Asia Pac J Clin Nutr. 2005;14:32-42.
- [Google Scholar]
- National Health Programme Series 5: National iodine deficiency disorders control programme. New Delhi: National Institute of Health and Family Welfare; 2010.
- National Health Mission, IDD & Nutrition Cell. 2006. Revised policy guidelines on National Iodine Deficiency Disorders Control Programme. New Delhi: Directorate General of Health Services, Ministry of Health & Family Welfare, Government of India; Available from: http://pbhealth.gov.in/revised%20policy%20guidelines%20govt.%20of%20india.pdf
- [Google Scholar]
- Gazette of India. 1997. GSR 670 (E) 1997. New Delhi: Ministry of Health and Family Welfare; Available from: https://archive.org/details/in.gazette.e.1997.868/page/n5
- [Google Scholar]
- Salt Commissioner of India. In: Annual report 2000-2001. Jaipur: Office of the Salt Commissioner of India. Salt Department, Ministry of Commerce and Industry, Government of India; 2001.
- [Google Scholar]
- International Institute for Population Sciences. In: National Family Health Survey (NFHS-2) 1998-99. Mumbai: IIPS; 2000.
- [Google Scholar]
- Gazette of India. 2000. GSR 716(E) 2000. New Delhi: Ministry of Health and Family Welfare; Available from: https://archive.org/details/in.gazette.central.e.2000-09-13.020/page/n1
- [Google Scholar]
- International Institute for Population Sciences. In: District Level Household Survey (DLHS-2), 2002-04. Mumbai: IIPS; 2006.
- [Google Scholar]
- International Institute for Population Sciences. In: National Family Health Survey (NFHS-3), 2005-06. Mumbai: IIPS; 2007.
- [Google Scholar]
- Gazette of India. 2005. GSR 670(E) 2005. New Delhi: Ministry of Health and Family Welfare; Available from: http://www.aiclindia.com/Acts/Prevention%20Of%20Food%20Adulteration%20(eighth%20Amendment)%20Rules%202006.pdf
- [Google Scholar]
- Supreme Court of India. Civil Writ Petition No 80/2006 (2011). Academy of nutrition improvement and Ors. vs. Union of India. Available from: https://www.indiankanoon.org/doc/665756/
- [Google Scholar]
- >Food Safety and Standards Authority of India. In: Food safety and standards (prohibition and restriction on Sales) regulation. New Delhi: Food Safety and Standards Authority of India; 2011.
- [Google Scholar]
- National Human Rights Commission. Available from: http://nhrc.nic.in/sites/default/files/AR03-04ENG.pdf
- [Google Scholar]
- The national coalition for sustained optimal iodine intake (NSOI): A case study of a successful experience from India. Asia Pac J Clin Nutr. 2014;23((Suppl 1)):S38-45.
- [Google Scholar]
- Successful implementation of a laboratory iodization quality assurance system in small-scale salt production facilities in India. Public Health Nutr. 2014;17:2816-23.
- [Google Scholar]
- Evolution of iodine deficiency disorders control program in India: A journey of 5,000 years. Indian J Public Health. 2013;57:126-32.
- [Google Scholar]
- Household coverage with adequately iodized salt varies greatly between countries and by residence type and socioeconomic status within countries: Results from 10 national coverage surveys. J Nutr. 2017;147:1004S-14S.
- [Google Scholar]
- Towards universal salt iodisation in India: achievements, challenges and future actions. Matern Child Nutr. 2015;11:483-96.
- [Google Scholar]
- S.O.S for a billion: The conquest of iodine deficiency disorders. Oxford University Pression 1994
- [Google Scholar]
- Iodized salt coverage study 2010 conducted across eight States in India. Available from: www.micronutrient.org
- [Google Scholar]
- A State-level salt iodization coalition achieves success in Bihar, India. Available from: http://www.ign.org/newsletter/idd_aug17_india.pdf
- [Google Scholar]
- International Institute of Population Sciences (IIPS) National Family Health Survey 4. 2015-16. Fact sheets. Mumbai: IIPS; Available from: http://rchiips.org/nfhs/factsheet_NFHS-4. shtml
- [Google Scholar]
- Salt industry in India. Available from: http://saltcomindia.gov.in/industry_india.html?tp=Salt
- [Google Scholar]






