Translate this page into:
Malaria-associated secondary haemophagocytic lymphohistiocytosis: Report of two cases & a review of literature
*For correspondence: sahajal@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Haemophagocytic lymphohistiocytosis (HLH), a systemic disorder caused by immune dysregulation, occurs in primary (genetic) and secondary (acquired) forms. Secondary HLH refers to cases triggered by infections, malignancy (predominantly haematologic) and autoimmune diseases1. Primary HLH is mostly recognized in childhood whereas the secondary form can occur at any age2. HLH secondary to infections can occur with viral, bacterial, fungal or parasitic infections; viral infections, [especially Epstein–Barr virus (EBV)], being the most common13. While the treatment of familial or primary HLH has been systematically studied and reported, the optimum treatment of secondary HLH remains speculative4. Literature on malaria-associated HLH is sparse. We describe here two cases of malaria-associated secondary HLH successfully managed with intravenous immunoglobulin (IVIG). The literature on secondary HLH associated with malaria, has also been reviewed.
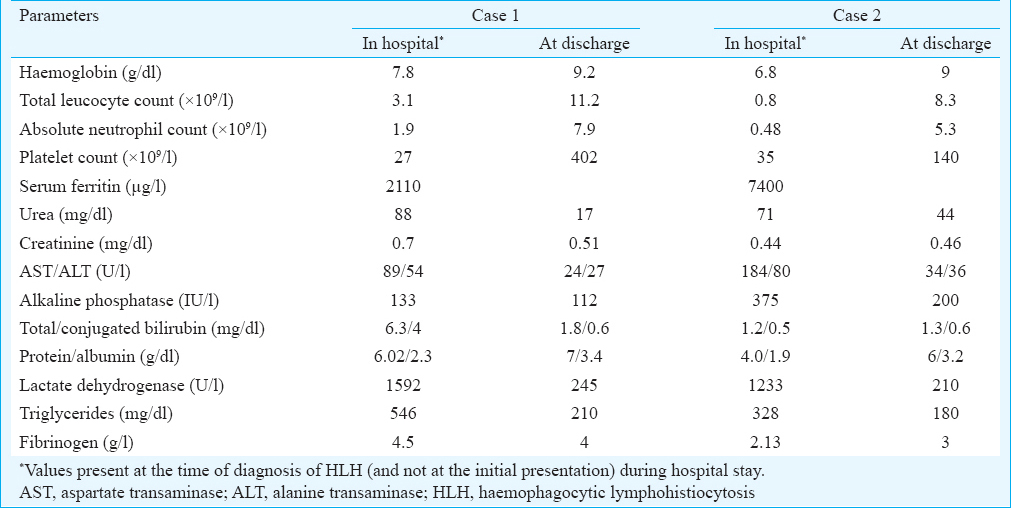
The first case was a 43 yr old male presented to the Pulmonary Medicine Outpatient Department (OPD), Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India, in August 2013 with fever, dry cough and breathlessness of four days’ duration. Examination revealed pallor, icterus and tachypnoea. Investigations showed the presence of anaemia, thrombocytopenia and conjugated hyperbilirubinaemia (Table I). Rapid diagnostic test [based on species-specific lactate dehydrogenase (LDH)] was positive for Plasmodium vivax as well as P. falciparum. The peripheral blood smear revealed P. vivax ring forms. Chest radiograph was suggestive of acute respiratory distress syndrome (ARDS). During the hospital stay, the patient developed worsening respiratory distress and hypotension. He was intubated and started on mechanical ventilation; vasopressors were administered. He was treated with intravenous (i.v.) ceftriaxone, i.v. artesunate and oral doxycycline. Following a transient clinical improvement, the patient's clinical status worsened. Investigations on day seven of hospitalization revealed pancytopenia. Clinical possibilities of sepsis-associated bone marrow suppression, drug-induced bone marrow suppression and HLH, were considered. Further investigations showed raised liver transaminases, raised serum LDH, hypertriglyceridaemia, raised serum ferritin and splenomegaly on abdominal ultrasonography. EBV and cytomegalovirus (CMV) serologies (IgM) were negative. Bone marrow aspiration showed the presence of haemophagocytosis (Figure A). A diagnosis of secondary HLH was made. IVIG (2 g/kg given in divided doses over five days) was administered for the management of secondary HLH. The patient's condition improved gradually and laboratory parameters including leucocyte and platelet counts, liver transaminases, serum LDH and triglycerides normalized. The patient was extubated on day 13 of hospitalization and discharged two days later. The patient was doing well after six months and his blood counts were all within normal limits.
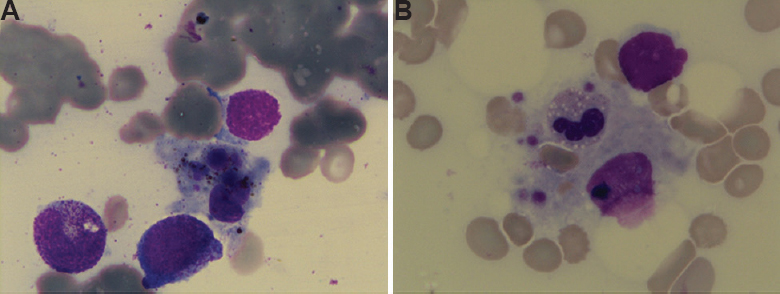
- (A)Hamophagocytosis seen on the bone marrow aspiration smear of case 1. (B) Bone marrow aspiration smear of case 2 showing haemophagocytosis with leucocytes, erythrocytes and platelets inside a macrophage.
The second case was a 34 yr old female who was admitted in December 2013 with high-grade fever and progressive breathlessness for 10 days. She had tachypnoea and pallor but no icterus or lymphadenopathy. On admission, she had normal liver and renal functions. Rapid diagnostic test (species-specific LDH-based immunochromatographic test) was positive for P. falciparum. However, the peripheral smear for malarial parasite was negative on four occasions. Chest radiograph and arterial blood gas analysis suggested ARDS. She was intubated and mechanically ventilated for respiratory failure. The patient was treated with i.v. ceftriaxone, i.v. artesunate and oral doxycycline along with best supportive care. She remained clinically sTable for two days, following which high-grade fever reappeared. Shock and hypoxaemia resolved, but pancytopenia worsened. Drug-induced bone marrow suppression, sepsis-associated bone marrow suppression and HLH were considered in the differential diagnosis. Secondary HLH was suspected in view of pancytopenia, raised liver transaminases, raised LDH, hypertriglyceridaemia, raised serum ferritin and hypofibrinogenaemia (Table I). Bone marrow aspiration and biopsy revealed haemophagocytosis (Figure B). IgM antibodies against CMV and EBV were absent. IVIG was administered over two days (total dose of 2 g/kg). Following this therapy, the laboratory parameters improved. She was extubated after 12 days of admission and discharged on day 21 of hospitalization after resolution of the nosocomial infection. No recurrence of fever or cytopenia was noted on follow up at six months.
The two cases described here exemplify the classic course of HLH secondary to tropical infections. HLH is suspected in patients presenting with high-grade fever and multisystem involvement15. Cytopenia and splenomegaly often draw the clinician's attention to the possibility of this rare syndrome. The findings of raised ferritin and triglyceride and/or a low fibrinogen further increase the probability of HLH. Confirmation often arrives from the demonstration of haemophagocytosis in the bone marrow biopsy6. It is noteworthy that the criteria used for diagnosing secondary HLH are an extrapolation from what is used for primary HLH and have not been validated systematically for secondary HLH4.
Malaria as a cause of secondary HLH is rare. The literature search yielded 17 studies (18 patients) reporting on patients with HLH secondary to malaria (Table II)7891011121314151617181920212223. A majority of the described cases have reported only six of the eight criteria used for HLH, and investigations to look for natural killer cell activity and soluble CD25 antigen levels were not available in most cases except one11. Only three of the 18 previously reported cases of malaria associated HLH had shown malarial parasites in bone marrow121322. Although malarial parasite/pigment was not demonstrated in the bone marrow of the remaining patients (including the index patients), malaria seems to be the most likely cause of secondary HLH in these cases due to the temporal relationship to the illness.
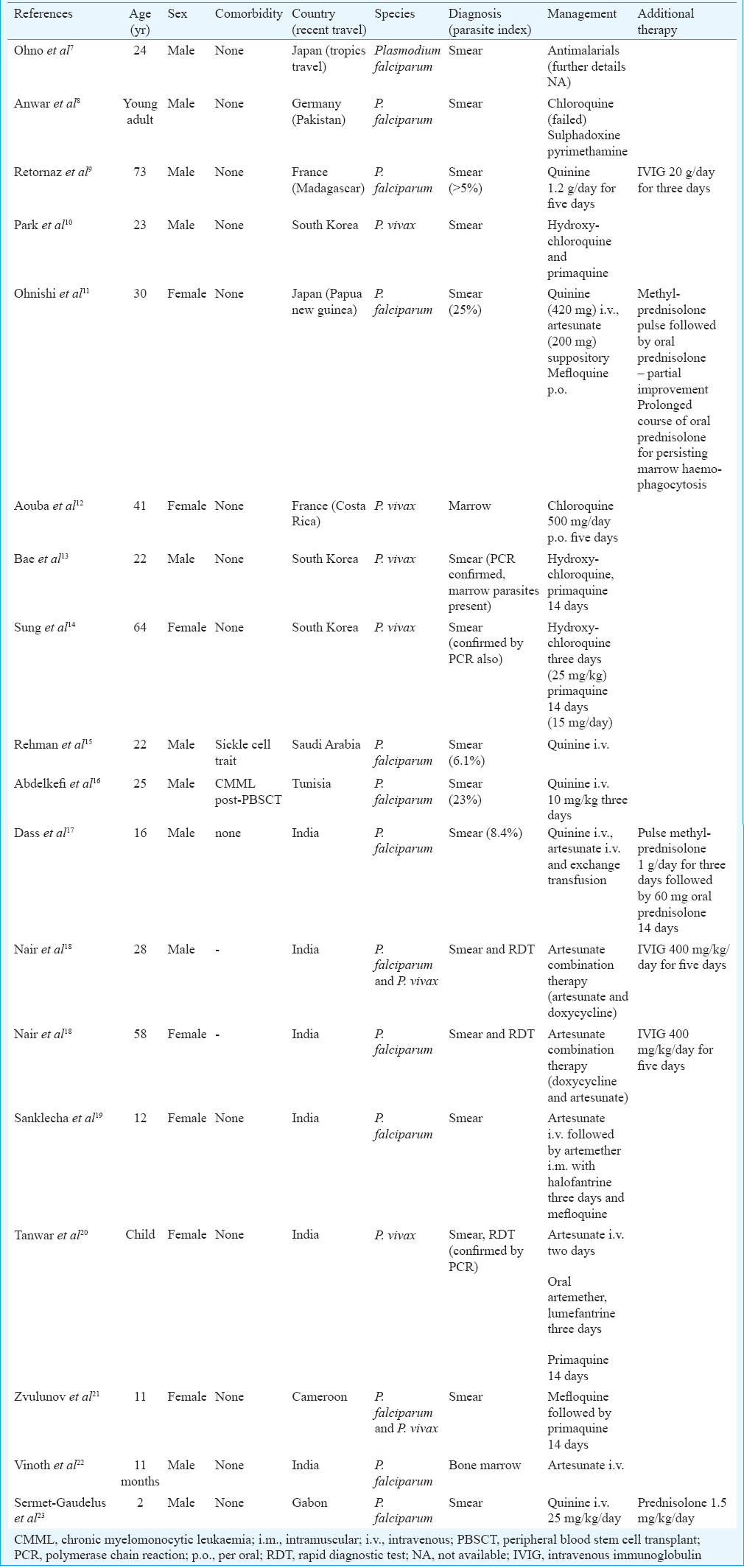
Of the 20 cases (including present two cases), three patients had dual infection with P. vivax and P. falciparum. All patients were either native of countries in Asia or Africa or had travelled to these places. The diagnosis of malaria was based on peripheral blood smear and/or rapid diagnostic tests for malarial antigens, supported by molecular methods in a few instances131420. Malaria-associated HLH was observed in previously healthy individuals except for two patients: an adult with sickle cell trait and the other with chronic myelomonocytic leukaemia following peripheral blood stem cell transplant1516. Twelve patients improved with antimalarial therapy alone and eight patients (40%) required additional immunosuppression. Of these eight patients, IVIG was used in five and corticosteroids in three. All patients recovered. No death due to malaria-associated HLH has been reported.
The treatment strategy for secondary HLH includes supportive care, treatment of inciting factor and the use of immunosuppressants (steroids, IVIG and other immunosuppressive drugs) in unresponsive cases1. Polyclonal IVIG, a preparation of IgG antibodies derived from pooled serum of thousands of donors, is used primarily as replacement therapy for patients with immunodeficiencies. IVIG has also been found to be used in the treatment of autoimmune conditions and even in sepsis where its primary mechanism of action is by immunomodulation24. The exact mode of its action in HLH needs further elucidation. The use of IVIG as the sole immunological treatment in infection-associated HLH, in particular malaria-associated HLH, warrants further investigation.
In conclusion, HLH in malaria is rare, although underrecognition and underreporting may contribute to the apparent rarity. Prospective and systematic data collection is essential to assess the incidence and the natural history of secondary HLH in the tropics. IVIG as an additional treatment option for this form of HLH needs further research.
Conflicts of Interest: None.
References
- Hemophagocytic lymphohistiocytosis: Review of etiologies and management. J Blood Med. 2014;5:69-86.
- [Google Scholar]
- Visceral leishmaniasis associated hemophagocytic lymphohistiocytosis – Case report and systematic review. J Infect. 2008;56:381-8.
- [Google Scholar]
- HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48:124-31.
- [Google Scholar]
- Severe hemophagocytic lymphohistiocytosis in adults-experience from an Intensive Care Unit from North India. Indian J Crit Care Med. 2012;16:198-203.
- [Google Scholar]
- Diagnosing and treating hemophagocytic lymphohistiocytosis in the tropics: Systematic review from the Indian subcontinent. Acta Med Acad. 2012;41:161-74.
- [Google Scholar]
- Hemophagocytic syndrome induced by Plasmodium falciparum malaria infection. Int J Hematol. 1996;64:263-6.
- [Google Scholar]
- Severe haemophagocytic syndrome in falciparum malaria. Pak Med Assoc. 1995;45:302-3.
- [Google Scholar]
- Plasmodium falciparum malaria infection complicated by haemophagocytic syndrome in an old man. Acta Haematol. 2000;103:224-5.
- [Google Scholar]
- Plasmodium vivax malaria complicated by hemophagocytic syndrome in an immunocompetent serviceman. Am J Hematol. 2003;74:127-30.
- [Google Scholar]
- Clinical case report: Falciparum malaria with hemophagocytic syndrome. Am J Trop Med Hyg. 2007;76:1016-8.
- [Google Scholar]
- Haemophagocytic syndrome associated with Plasmodium vivax infection. Br J Haematol. 2000;108:832-3.
- [Google Scholar]
- Plasmodium vivax malaria-associated hemophagocytic lymphohistiocytosis in a young man with pancytopenia and fever. Ann Hematol. 2011;90:491-2.
- [Google Scholar]
- Hemophagocytic lymphohistiocytosis (HLH) associated with Plasmodium vivax infection: Case report and review of the literature. Chonnam Med J. 2011;47:173-6.
- [Google Scholar]
- Falciparum malaria in a patient with sickle cell trait with hemophagocytosis and secondary pancytopenia. Ann Hematol. 2012;91:1329-30.
- [Google Scholar]
- Plasmodium falciparum causing hemophagocytic syndrome after allogeneic blood stem cell transplantation. Hematol J. 2004;5:449-50.
- [Google Scholar]
- A clinicopathological analysis of 26 patients with infection-associated haemophagocytic lymphohistiocytosis and the importance of bone marrow phagocytosis for the early initiation of immunomodulatory treatment. Postgrad Med J. 2013;89:185-92.
- [Google Scholar]
- Varied presentation of complicated falciparum malaria in a family. Indian Pediatr. 2012;49:413-4.
- [Google Scholar]
- Hemophagocytic syndrome associated with severe Plasmodium vivax malaria in a child in Bikaner (Northwestern India) J Vector Borne Dis. 2013;50:318-20.
- [Google Scholar]
- Pancytopenia resulting from hemophagocytosis in malaria. Pediatr Infect Dis J. 2002;21:1086-7.
- [Google Scholar]
- Hemophagocytic syndrome associated with Plasmodium falciparum infection. Indian J Pathol Microbiol. 2011;54:594-6.
- [Google Scholar]
- Haemophagocytic syndrome in Plasmodium falciparum malaria. Acta Paediatr. 2000;89:368-9.
- [Google Scholar]
- Intravenous immunoglobulin for treating sepsis, severe sepsis and septic shock. Cochrane Database Syst Rev. 2013;9:CD001090.
- [Google Scholar]





