Translate this page into:
Acute kidney injury is an independent predictor of in-hospital mortality in a general medical ward: A retrospective study from a tertiary care centre in south India
For correspondence: Dr Murugabharathy Kalimuthu, Department of Internal Medicine, Christian Medical College & Hospital, Vellore 632 004, Tamil Nadu, India e-mail: bharathymuruga@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Acute kidney injury (AKI) has been identified as an independent risk factor for mortality in intensive care units. This retrospective study was conducted to determine the effect of AKI on in-hospital mortality in a general medical ward of a tertiary care hospital and risk factors for mortality in patients with AKI.
Methods:
Demographic and clinical details, and outcome data were collected from case records of patients. In all hospitalized patients, factors associated with increased in-hospital mortality, such as AKI, inotrope requirement, mechanical ventilation and primary disease were compared between patients who died during their hospital stay and those who were discharged alive. Among the hospitalized patients, who had AKI, likely predictors of in-hospital mortality were compared between dead and alive patients at discharge. Factors that were significant in univariate analysis were tested by multivariate regression analysis to identify those that independently predicted poor outcomes.
Results:
Of the 1150 patients admitted in a general medical ward in a year, 220 patients were identified to have AKI. In-hospital mortality rate among patients with AKI was 19.09 per cent as compared to 1.8 per cent without AKI [adjusted odds ratio (OR) 5.7 (95% CI: 1.56-20.74)]. The presence of AKI was an independent risk factor for death, with an adjusted OR of 6.0 [95% CI: 1.67-21.6]. Among patients with AKI, the presence of haematological malignancy, adjusted OR 25.86 (95% CI: 1.81-369.58), requirement of inotrope, adjusted OR 126.5 (95% CI: 19.39-825.93) and serum creatinine at admission (P<0.001) were found to be independent predictors of death. The presence of underlying chronic kidney disease and hospital-acquired AKI were not found to have an association with mortality.
Interpretation & conclusions:
The study showed the in-hospital mortality rate among patients with AKI in a general medical ward was 19.09 per cent. The occurrence of AKI was an independent risk factor for death, with haematological malignancy, use of vasopressors and higher serum creatinine at admission, significantly associated with death among patients with AKI. Large prospective studies need to be done to better understand the outcomes in AKI and the ways to present and manage AKI.
Keywords
Acute kidney injury
in-hospital
mortality
risk factors
Acute kidney injury (AKI) is increasingly being diagnosed in healthcare, more so in critically ill patients. Numerous studies have been done to evaluate the incidence of AKI in critical care units and in specific situations such as sepsis, contrast administration and trauma care setting and to characterize the prognostic factors12. It is a well-recognized fact that the occurrence of AKI is an independent determinant of mortality and morbidity in addition to the primary disease causing the AKI3.
Most studies from India have described the incidence of AKI and its impact on mortality and morbidity in the intensive care unit (ICU) setting456. Only a few studies have addressed the clinical profile of AKI in medical and surgical settings individually78.
Differences have been observed in the aetiologies and precipitating factors of AKI in community-acquired and hospital-acquired AKI9101112.
The present study was undertaken to estimate the effect of AKI on in-hospital mortality in a medical ward and to identify the risk factors for mortality.
Material & Methods
This was a single-centre retrospective study conducted in the department of Internal Medicine, Christian Medical College, Vellore, India. Cases were patients who were admitted in a general medical unit between July 1, 2016 and June 31, 2017, with a diagnosis of AKI by the AKI Network (AKIN) classification13. Controls were patients who were admitted during the same period but did not have AKI. Controls were randomly selected from these patients in a 1:1 ratio. The patients with AKI were classified further into community-acquired AKI and hospital-acquired AKI. Hospital-acquired AKI was defined as an increase in serum creatinine by 0.3 mg/dl during the hospital stay with a normal admission creatinine. The recruitment of patients is described in the Figure.
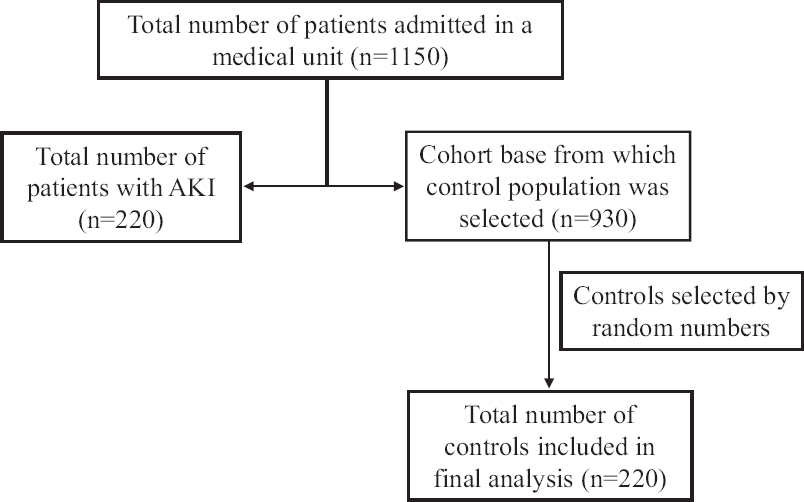
- Flow diagram of the study.
Demographic data and information on risk factors, need for intensive care, renal replacement, ventilator support, inotropic support and the outcome were collected. The data were extracted by one investigator and entered using Epidata software version 3.1 (Epidata Association, Odense, Denmark). A second investigator verified every tenth case report form and errors which were found and were rectified by consensus. Selection bias was addressed by including all cases which were identified during the period and by selecting a random control population. The study was approved by the institutional review board and ethics committee of the participating institution. [IRB Number 10993 (retro)]. Written informed consent was obtained from each participant.
Statistical analysis: The data collected were analyzed using SPSS Inc. (SPSS for Windows, version 16.0, Chicago, IL, USA). Factors associated with increased in-hospital mortality, (AKI, inotrope requirement, mechanical ventilation, primary disease) were compared between hospitalized patients who died during their hospital stay and those who were discharged alive, by chi-square analysis. A similar analysis was done separately in the hospitalized patients with AKI, to determine the predictors of in-hospital mortality, and those found significant in univariate analysis were entered into a multivariate regression analysis to identify factors that independently predicted poor outcomes.
Results
During the one year study period, a total of 1150 patients were admitted in the medicine ward. Of these, 220 (19.13%) had AKI. The patients with AKI had a significantly higher proportion of diabetes mellitus, hypertension, chronic kidney disease (CKD), congestive cardiac failure, exposure to diuretics, systemic infection, vasopressor requirement, ICU admission and requirement of mechanical ventilation (Table I). The non-AKI group had a higher proportion of patients exposed to angiotensin-converting enzyme inhibitors or angiotensin receptor blockers. Among those with AKI, 19.1 per cent expired during the hospital stay as compared to 1.8 per cent without AKI, adjusted odds ratio (OR) 5.7 [95% confidence interval (CI): 1.56-20.74]. In total 23 of 220 patients with AKI (10.5%) required dialysis and all of them underwent haemodialysis. Ten of the 23 who underwent dialysis died. Among those with community-acquired AKI (n=104), 56 (53.8%) had complete recovery at discharge, 41 (39.4%) had partial recovery and seven (6.7%) were dialysis dependent. Among hospital-acquired AKI (n=77), eight (10.4%) had a complete recovery, 53 (68.8%) had partial recovery and 16 (20.8%) were dialysis dependent. Thirty nine patients had insufficient data to be categorized into the community or hospital-acquired AKI.
| Parameters | Non-AKI, n (%) | AKI, n (%) | OR (95% CI) unadjusted |
|---|---|---|---|
| Age, yr (mean±SD) | 47.85±17.33 | 56.92±14.85 | |
| Male gender | 111 (50.5) | 138 (62.7) | 1.65 (1.13-2.42)* |
| Category of AKI# | |||
| Community acquired | 104 (47.3) | ||
| Hospital acquired | 77 (35) | ||
| Comorbid illnesses | |||
| Diabetes mellitus | 74 (33.6) | 135 (61.4) | 3.13 (2.12-4.63)* |
| Hypertension | 74 (33.6) | 134 (60.9) | 3.07 (2.08-4.54)* |
| Chronic kidney disease | 3 (1.4) | 103 (46.8) | 63.68 (19.77-205.12)* |
| Chronic liver disease | 5 (2.3) | 8 (3.6) | 1.62 (0.52-5.04) |
| Congestive cardiac failure | 15 (6.8) | 40 (18.2) | 3.04 (1.62-5.68)* |
| Acute coronary syndrome | 5 (2.3) | 19 (8.6) | 4.06 (1.49-11.09)* |
| Cerebrovascular accident | 17 (7.7) | 15 (6.8) | 0.87 (0.42-1.80) |
| Solid organ tumour | 9 (4.1) | 5 (2.3) | 0.54 (0.18-1.65) |
| Hematological malignancy | 4 (4.1) | 6 (2.7) | 1.51 (0.42-5.44) |
| Peripheral vascular disease | 0 | 4 (1.8) | |
| Dementia | 1 (0.5) | 1 (0.5) | 1.00 (0.06-16.09) |
| Peptic ulcer disease | 1 (0.5) | 0 | |
| Systemic lupus erythematosus | 7 (3.2) | 1 (0.5) | 0.14 (0.02-1.14) |
| Rheumatoid arthritis | 4 (1.8) | 1 (0.5) | 0.25 (0.03-2.22) |
| Systemic sclerosis | 1 (0.5) | 0 | |
| Chronic obstructive pulmonary disesase | 13 (5.9) | 6 (2.7) | 0.45 (0.17-1.20) |
| HIV infection | 2 (0.9) | 3 (1.4) | 1.51 (0.25-9.08) |
| Hepatitis B infection | 1 (0.5) | 2 (0.9) | 2.01 (0.18-22.32) |
| Hepatitis C infection | 0 | 1 (0.5) | |
| Medication use | |||
| NSAID | 5 (2.3) | 3 (1.4) | 0.59 (0.14-2.52) |
| Steroid | 55 (25) | 58 (26.4) | 1.07 (0.7-1.65) |
| Cancer chemotherapy | 3 (1.4) | 5 (2.3) | 1.68 (0.40-7.13) |
| Anti-retroviral therapy | 0 | 1 (0.5) | |
| Native medication | 1 (0.5) | 1 (0.5) | 1.00 (0.06-16.09) |
| Diuretics | 26 (11.8) | 91 (41.4) | 5.26 (3.23-8.59)* |
| ACEI or ARB | 57 (25.9) | 31 (14.1) | 0.47 (0.29-0.78)* |
| Beta-lactam | 25 (11.4) | 22 (10) | 0.87 (0.47-1.59) |
| Rifampicin | 1 (0.5) | 7 (3.2) | 7.20 (0.88-59.00) |
| Sulphonamide | 0 | 0 | |
| Aminoglycosides | 1 (0.5) | 2 (0.9) | 2.01 (0.18-22.32) |
| Quinolones | 12 (5.5) | 8 (3.6) | 0.65 (0.26-1.63) |
| Proton pump inhibitors | 213 (96.8) | 206 (93.6) | 0.48 (0.19-1.22) |
| Amphotericin | 0 | 4 (1.8) | |
| Drugs - others | 200 (90.9) | 191 (86.8) | 0.66 (0.36-1.20) |
| Clinical and laboratory features | |||
| Urine output - oliguric | 1 (0.5) | 41 (18.6) | |
| Urine output - anuric | 0 | 3 (1.4) | |
| Dependant oedema | 33 (15) | 65 (29.5) | |
| Ascites | 9 (0.9) | 18 (8.2) | |
| Asterixis | 0 | 8 (3.6) | |
| Dysmorphic RBCs | 1 (0.5) | 3 (1.4) | |
| Aetiology | |||
| Systemic infection | 85 (38.6) | 122 (55.5) | 1.98 (1.35-2.89)* |
| Diarrhoeal disease | 6 (2.7) | 13 (5.9) | |
| Malaria | 0 | 3 (1.4) | |
| Dengue | 5 (2.3) | 4 (1.8) | 0.80 (0.21-3.01) |
| Leptospirosis | 0 | 1 (0.5) | |
| Scrub typhus | 8 (3.6) | 5 (2.3) | 0.62 (0.20-1.91) |
| Enteric fever | 2 (0.9)) | 1 (0.5) | 0.50 (0.04-5.53) |
| Heat related illness | 0 | 2 (0.9) | |
| Treatment | |||
| ICU stay | 17 (7.7) | 62 (28.2) | 4.69 (2.63-8.33)* |
| Invasive ventilation | 10 (4.5) | 49 (22.3) | 6.02 (2.96-12.23)* |
| Inotrope requirement | 5 (2.3) | 47 (21.4) | 11.68 (4.55-30.01)* |
| Outcome | |||
| Death | 4 (1.8) | 42 (19.1) | 12.74 (4.48-36.21)* |
*P<0.05; #Missing data for 39 patients. AKI, acute kidney injury; OR, odds ratio; CI, confidence interval; SD, standard deviation; NSAID, non-steroidal anti-inflammatory drug; ACEI, angiotensin converting enzyme inhibitor, ICU, intensive care unit; RBCs, red blood cells; ARB, angiotensin receptor blocker
Among the patients admitted in the general medical ward, the occurrence of AKI was an independent predictor of death with an OR of 6.0 ((95% CI: 1.67-21.6) (Table II). Among those with AKI, the independent predictors of death were inotrope use [OR 40.78 (95% CI: 14.18-117.23)], haematological malignancy [OR 16.34 (95% CI: 2.34-114.15)] and serum creatinine at admission. The presence of CKD and hospital-acquired AKI were not predictive of death (Table III).
| Variable | Death (n=46), n (%) | Alive (n=394), n (%) | Adjusted OR# (95% CI) | P |
|---|---|---|---|---|
| AKI | 42 (91.3) | 178 (45.2) | 6.00 (1.67-21.61) | 0.006 |
| Inotrope use | 32 (69.6) | 20 (5.1) | 36.4 (14.34-92.54) | 0.001 |
| Solid organ malignancies | 3 (6.5) | 7 (2.8) | 12.31 (2.16-68.12) | 0.005 |
| Haematological malignancies | 3 (6.5) | 11 (1.8) | 9.93 (1.71-57.65) | 0.010 |
#Adjustment done for gender (male), diabetes mellitus, chronic kidney disease, congestive cardiac failure, hypertension, acute coronary syndrome
| Variable | Death (n=42) | Alive (n=178) | Adjusted OR* (95% CI) | P |
|---|---|---|---|---|
| Diabetes mellitus | 23 | 112 | 0.571 (0.15-2.21) | 0.418 |
| Chronic kidney disease | 15 | 88 | 2.348 (0.50-11.06) | 0.280 |
| Congestive cardiac failure | 10 | 30 | 2.253 (0.46-11.06) | 0.317 |
| Systemic infection | 33 | 89 | 1.351 (0.24-7.60) | 0.732 |
| Inotrope requirement | 32 | 15 | 126.5* (19.39-825.93) | <0.001 |
| Solid organ malignancy | 2 | 3 | 8.672 (0.99-758.07) | 0.344 |
| Haematological malignancy | 3 | 3 | 25.86* (1.81-369.58) | 0.017 |
| Hospital acquired AKI | 18 | 81 | 0.699 (0.34-6.03) | 0.626 |
| Admission creatinine, median (IQR) | 1.84 (1.86) | 1.12 (1.70) | <0.001# |
#P-value by Mann-Whitney U-test; *Adjusted for diabetes mellitus, chronic kidney disease, congestive cardiac failure, systemic infection, inotrope requirement, solid organ malignancy, haematological malignancy and hospital acquired AKI. IQR, interquartile range
Discussion
The incidence of AKI as reported in various studies has been 1.68 per cent to 22.7 per cent141516. These studies have been done outside India and in critically ill patients admitted in the ICU. In our study, 19.13 per cent in-patients had AKI. The in-hospital mortality among patients with AKI has been reported in various studies to be between 9.1 per cent and 43.5 per cent171819202122. In studies from India mortality ranged between 19.6 and 29.2 per cent1922, though the investigators included patients developing AKI due to medical, surgical, obstetric causes and post-operative patients. Our hospital mortality of 19.1 per cent in patients with AKI was within the same range. The mortality was significantly higher in the AKI group when compared to the non-AKI group. A few studies have shown a decreasing trend in mortality in patients with AKI192021222324. An analysis of mortality among patients admitted in the general medical ward revealed AKI as an independent risk factor for death with an OR of 6.0 (95% CI: 1.67-21.6).
The study also showed that in patients with AKI, the odds of the death being high with the presence of haematological malignancy, vasopressor requirement and higher serum creatinine at admission. Vasopressor requirement is indicative of the severity of illness and the presence of shock is a well-known risk factor for mortality. The number of patients with haematological malignancies in this study was only 11; hence, the results will have to be interpreted with caution. The presence of CKD was not predictive of death in our study. This was in contrast to various other reported studies2324252627 which found older age, pre-existing CKD, presence of infectious disease, malignancies, oliguria, higher AKI stage, need for renal replacement therapy, vasopressor requirement, cardiovascular disease, multiple organ dysfunction syndrome and need for ICU admission as being significant risk factors for death.
The present study was a retrospective descriptive study based on hospital records, and relied on information given in the patient records. This being a study from a general medical ward of single tertiary care centre, the results cannot be generalized to medical wards in hospitals of all levels. About 46 per cent of patients with AKI had pre-existing CKD whose prognosis can be different from AKI alone. Ultrasonogram was performed only in 160 of the 220 patients with AKI. We did not analyze the impact of comorbidity indices, APACHE scores, duration of ICU stay, mechanical ventilation and inotrope requirement which could have impacted mortality in AKI. An analysis including serial creatinine measurements from baseline, stages of AKI with mortality and risk factors, may give a better understanding of their correlation and odds of adverse outcomes with specific creatinine levels.
In conclusion, our study showed AKI as an independent predictor of mortality in patients admitted in a general medical ward. The presence of haematological malignancy, requirement of vasopressors and higher serum creatinine at admission were significant predictors of death among patients with AKI. Larger prospective studies categorizing the severity of AKI by the AKIN classification or RIFLE (Risk, Injury, Failure, Loss of kidney function, End-stage kidney disease) criteria13, are required for a better understanding of outcomes in AKI and its prevention and appropriate management.
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- Spectrum of acute kidney injury in critically ill patients: A single center study from South India. Indian J Nephrol. 2014;24:280-5.
- [Google Scholar]
- Epidemiology of acute kidney injury in the intensive care unit. Crit Care Res Pract. 2013;2013:479730.
- [Google Scholar]
- Acute kidney injury is a common and serious condition.The clinical significance is great and probably underestimated. Lakartidningen. 2016;113:pii: DXD3.
- [Google Scholar]
- Epidemiology and outcomes of acute kidney injury in critically Ill: Experience from a tertiary care center. Indian J Nephrol. 2018;28:413-40.
- [Google Scholar]
- Predictors of mortality in acute kidney injury patients admitted to medicine intensive care unit in a rural tertiary care hospital. Indian J Crit Care Med. 2018;22:231-7.
- [Google Scholar]
- Acute kidney injury-incidence, prognostic factors, and outcome of patients in an Intensive Care Unit in a tertiary center: A prospective observational study. Indian J Crit Care Med. 2016;20:332-6.
- [Google Scholar]
- Community acquired AKI: A prospective observational study from a tertiary level hospital in southern India. Indian J Nephrol. 2019;29:254-60.
- [Google Scholar]
- Epidemiology and outcome of acute kidney injury from a tertiary care hospital in India. Saudi J Kidney Dis Transpl. 2018;29:956-66.
- [Google Scholar]
- Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 2005;16:3365-70.
- [Google Scholar]
- Acute kidney injury is a powerful independent predictor of mortality in critically ill patients: A multicenter prospective cohort study from Kinshasa, the Democratic Republic of Congo. BMC Nephrol. 2016;17:118.
- [Google Scholar]
- Acute kidney injury and mortality in hospitalized patients. Am J Nephrol. 2012;35:349-55.
- [Google Scholar]
- The RIFLE and AKIN classifications for acute kidney injury: A critical and comprehensive review. Clin Kidney J. 2013;6:8-14.
- [Google Scholar]
- Incidence, outcomes, and comparisons across definitions of AKI in hospitalized individuals. Clin J Am Soc Nephrol. 2014;9:12-20.
- [Google Scholar]
- Epidemiology and clinical correlates of AKI in Chinese hospitalized adults. Clin J Am Soc Nephrol. 2015;10:1510-8.
- [Google Scholar]
- Incidence, aetiology and outcome of community-acquired acute kidney injury in medical admissions in Malawi. BMC Nephrol. 2017;18:21.
- [Google Scholar]
- Incidence, outcomes, and risk factors of community-acquired and hospital-acquired acute kidney injury: A retrospective cohort study. Medicine (Baltimore). 2016;95:e3674.
- [Google Scholar]
- Hospital-acquired acute kidney injury in medical, surgical, and intensive care unit: A comparative study. Indian J Nephrol. 2013;23:24-9.
- [Google Scholar]
- Spectrum of acute kidney injury in the Himalayan region. Indian J Nephrol. 2012;22:363-6.
- [Google Scholar]
- Hospital mortality in the United States following acute kidney injury. Biomed Res Int. 2016;2016:4278579.
- [Google Scholar]
- Community-acquired acute kidney injury in adults in Africa. Clin Nephrol. 2016;86:48-52.
- [Google Scholar]
- Epidemiologic trend changes in acute renal failure - a tertiary center experience from South India. Ren Fail. 2006;28:405-10.
- [Google Scholar]
- A nationwide survey of clinical characteristics, management, and outcomes of acute kidney injury (AKI) - patients with and without preexisting chronic kidney disease have different prognoses. Medicine (Baltimore). 2016;95:e4987.
- [Google Scholar]
- Acute renal failure mortality in hospitalized African Americans: Age and gender considerations. J Natl Med Assoc. 2002;94:127-34.
- [Google Scholar]
- Acute kidney injury burden in different clinical units: Data from nationwide survey in China. PLoS One. 2017;12:e0171202.
- [Google Scholar]
- Acute kidney injury: Experience from a state run tertiary care centre in Southern India. Int J Med Res Health Sci. 2016;5:83-7.
- [Google Scholar]
- Characteristics of and risk factors for death in elderly patients with acute kidney injury: A multicentre retrospective study in China. Postgrad Med J. 2018;94:249-53.
- [Google Scholar]






