Translate this page into:
Immunohistochemistry on pattern of ocular & adnexal tumours in a tertiary eye care centre of Northeast India
For correspondence: Dr Dipankar Das, Department of Ocular Pathology, Uveitis & Neuro-Ophthalmology Services, Sri Sankaradeva Nethralaya, Beltola, Guwahati 781 028, Assam, India e-mail: dr_dasdipankar@yahoo.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Ocular and adnexal tumours are important causes of morbidity in India and globally. Immunohistochemistry (IHC) is a vital molecular pathology tool, which helps to diagnose a tumour with more accuracy. The present study was undertaken to document the profile of ocular and adnexal tumour with IHC at a tertiary eye care center in Northeast India.
Methods:
This was a prospective and laboratory-based study. Histopathological and IHC study of the ocular and adnexal tumour was carried out from 2012 to 2014. Selection of pathological cases was made on the result of the histological diagnosis. All samples were subjected to IHC using kits for different antibodies as per indications.
Results:
In total, 645 tumours were included in our study, with 449 benign conditions and 196 were malignant tumours. Total IHCs were done in 87 tumours and 238 of antibodies were used. Non-Hodgkin's lymphomas (B-cell, low-to-intermediate type and mucosal-associated lymphoid tumours) were the most common tumor.
Interpretation & conclusions:
Clinical utility of the IHCs in different ophthalmic tumours can enable pathologists to make an accurate diagnosis and thus help in the overall management of the patient care. IHC may be carried out using various methods and some of the methods practiced are time consuming and tedious. In this study, kit methods were used which were found to be simpler and less time-consuming.
Keywords
Histopathology
immunohistochemistry
lymphoma
melanoma
orbit
retinoblastoma
Tumours of eye and adnexa are not rare in our country and Northeast region of India12 We have earlier published profile of ocular and adnexal tumours of 10 years with 1003 cases1. Extension of this study in a tertiary care eye centre of Northeast India was carried forward with molecular pathology diagnostic tools of immunohistochemistry (IHC). IHC study for orbital, lid, other adnexal tissues and ocular and intraocular tumours is important when the complete diagnosis of these tumours is sought.
The identification of specific cellular antibodies in paraffin wax embedded tissues plays an important role123 and it has revolutionized diagnostic histopathology45. We present here the profile of ocular and adnexal tumours diagnosed with molecular pathology technique (IHC) at a tertiary care eye centre of Northeast India.
Material & Methods
The histopathological and IHC reports were collected from the ocular pathology laboratory of Sri Sankaradeva Nethralaya, Guwahati, India, a tertiary eye care centre of Northeast India between 2012 and 2014. In total, 645 tumours were included in the study, with 449 benign and 196 were malignant tumours. Total IHCs were done in 87 tumours, and a total of 238 antibodies were used.
The study was approved by the Institutional Ethics Committee and written informed consent was obtained from all patients. The design of the study was prospective and laboratory based. All patients with conjunctival, lid, orbital, adnexal and intraocular tumours were included in the study. After initial diagnosis using haematoxylin and eosin (H & E) stains, samples were subjected to IHCs using number markers as per indications.
Paraffin embedded tissues were sectioned at 2-4 μm on the coated slides with the help of LEICA RM 2145 microtome (Germany). The tissues in the slides were kept for one hour at 60°C followed by deparaffinization with xylene, graded alcohol and distilled water.
The IHC was carried out using kits available commercially (BioGenex, USA). Buffer washing was used with tris-buffered saline (×1), pH 7.6 followed by peroxidase block (100 μl) for 10 min at room temperature. After subjecting to second buffer, slides were drowned for a hydrophobic blockade in the region of the tissue using a tissue tek pen. Power block was prepared using 100 μl of commercially available kit solution for 30 min and antibody (primary) incubation for overnight at 2-8°C. The third buffer was used by washing with the addition of super enhancer (100 μl) for 1.5 hours at room temperature. Again, buffer wash was done with the addition of polymer horseradish peroxidase (100 μl) for another 1.5 hours at room temperature and a drop of diaminobenzidine (DAB) chromogen in one ml of stable DAB buffer was added for five minutes at room temperature. Further washing and H and E counterstaining for 45 sec to one minute was carried out. Final washing, clearing and mounting of slides were done, and slides were seen and documented under a compound microscope (ZEISS, Axioskop 40 with AxioCam MRc, Germany).
IHC panel (BioGenex, USA) was selected as CD20 (B-cell), CD3 (T-cell), CD45 (leucocyte common antigen), CD10 (immature B-cell), CD31 (endothelial cells, platelets and macrophages), CD34 (endothelial cells), CD38 (for leucemic prognosis) and CD99/MIC2 (for diffuse large-B-cell lymphoma, primitive neuroectodermal tumour, metastatic Ewing's sarcoma, etc.), neuron-specific enolase (NSE) [retinoblastoma (RB)], Glial fibrillary acidic protein (GFAP) (optic nerve), C-myc (RB), P-53 (RB), factor-VIII (endothelial cells), P16 (RB), Bax protein (pro-apoptotic marker), cytokeratin (CK) (squamous cell carcinoma and other ocular surface neoplasia), Ki-67 (for proliferative index). Vimentin, desmin, and actin testing was done in mesenchymal tumours such as rhabdomyosarcoma. S100 protein was useful as a marker of tumours such as schwannomas and neurofibromas. BCL2 antibody, the anti-apoptotic protein was useful for some of the tumours. HMB45 was done in various ocular and adnexal melanomas. Chromogranin and synaptophysin testing was done in neuroendocrine tumours such as metastatic carcinoid to the orbit, and expression was also seen in RB with new rosettes, where both markers did not yield positive results. Neurofilament was seen in some of the neuroblastic tumours metastatic to orbit. Collagen-IV molecule was seen in some of the basement membranes of the cornea and ciliary body.
Results
In two years of study period (2012-2014), total tumours studied were 645, of which, 449 were benign and 196 were malignant. Total IHC was done in 87 tumors (Table) and in all 238 different antibodies were used. In 185 conjunctival tumours, 45 were malignant and in 11 cases, IHC was done. Of the 220 lid tumours, 49 were malignant, and IHC was done in eight cases and of these, four cases were squamous cell carcinoma of the lid. In benign lid tumours (n=171), IHC was done in five cases.
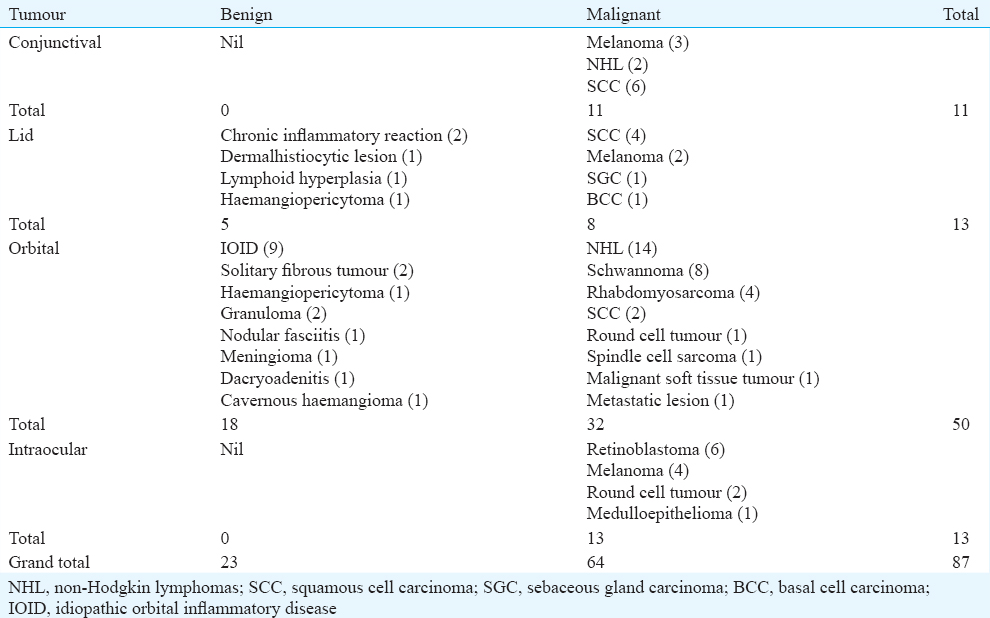
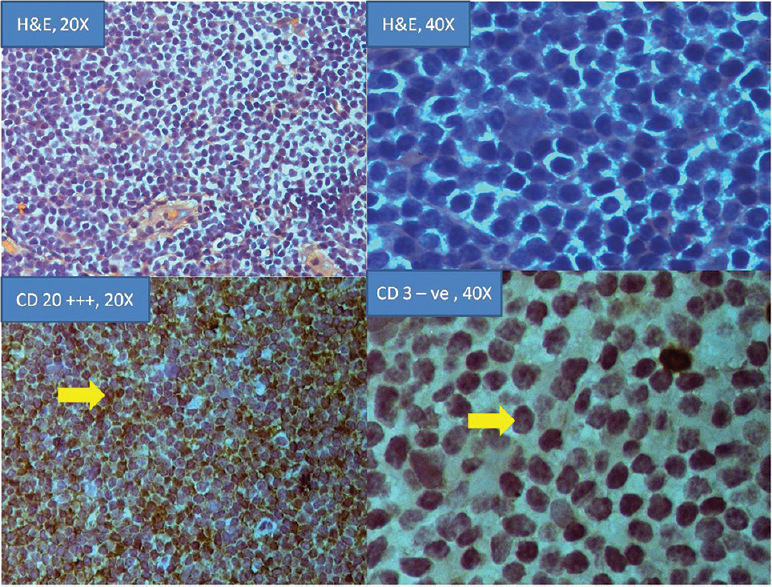
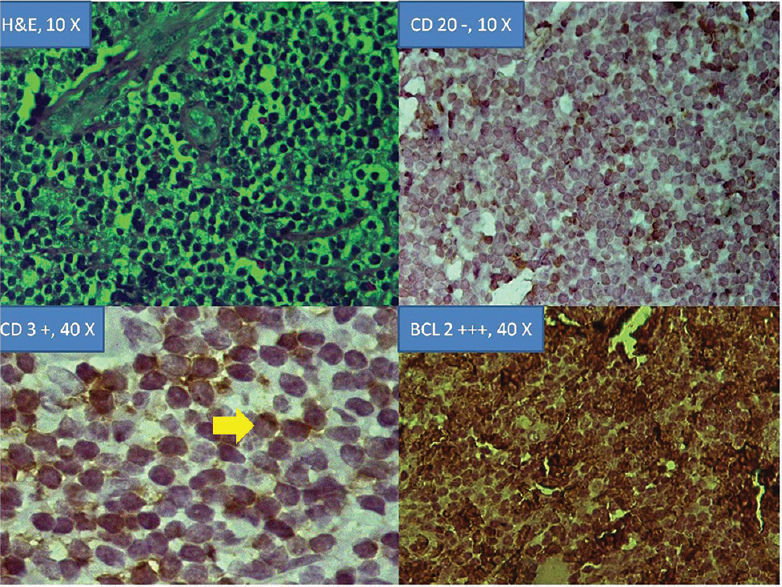
Of the 172 orbital cases, 65 were malignant and 107 had benign pathology. Fifty IHCs were done in orbital pathologies, of which 32 cases were malignant and 18 were benign. Non-Hodgkin lymphomas (NHL) of orbit were 14 in numbers, which were confirmed by IHC for B-cell and T-cell antibodies (Fig. 1). BCL 2 was positive in diffuse large B-cell lymphoma in two cases of orbital NHLs. In both the cases, abnormal B cells were seen in varying stages of differentiation and thus, the immunophenotype in those cases were heterogeneous (Fig. 2). One case of T cell NHL of the orbit was documented (Fig. 2). IHC for the squamous cell carcinoma was the highest in this study group (Fig. 3) and proliferative index for each case was seen by Ki 67 immunostain. NHL of orbit was the commonest orbital pathology in the series. The benign cases included six cases of idiopathic orbital inflammatory disease (IOID), two of reactive lymphoid hyperplasia and one case of atypical benign lymphocytic infiltrate. In the benign group of orbit tumours, all cases were confirmed by various markers and special stains such as the Grocott's methenamine silver stain (GMS) for fungus, acid-fast bacilli (AFB) for mycobacteria and tissue Gram's stain (GIS). IHC with CD3, CD20 and CD45 showed polyclonal involvement with negative GMS, GIS and AFB for IOID.
- Hematoxylin and eosin, (×20 and ×40) and immunohistochemistry of non-Hodgkin lymphomas of orbit with CD 20 (×20) and CD 3 (×40) immunostains.
- Hematoxylin and eosin, (×10) and immunohistochemistry of T-cell non-Hodgkin lymphomas of orbit with CD 20 –(×10), CD 3 + (×40) and B-cell lymphoma +++ (×40).
- Hematoxylin and eosin, (×20) and immunohistochemistry for cytokeratin (ck) positivity (×40 and ×20) in a squamous cell carcinoma of conjunctiva. Positive control (×10) shown.
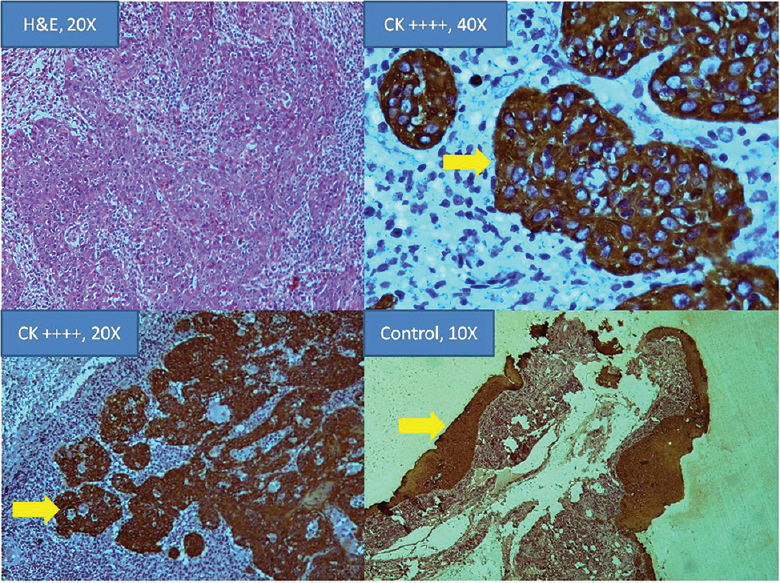
Of the 73 intraocular tumours, 13 IHC were malignant cases and RB was found in six cases and melanoma was found in four. In RB, IHC was carried out for NSE, P53, P16, Bax protein and GFAP. All positive controls showed appropriate positive immunostaining. Negative control slide did not show immunostaining (Fig. 4). One rare case of intraocular IgG4 related disease mimicking ciliary body melanoma was documented. Similarly, another case was noted arising from the orbit.
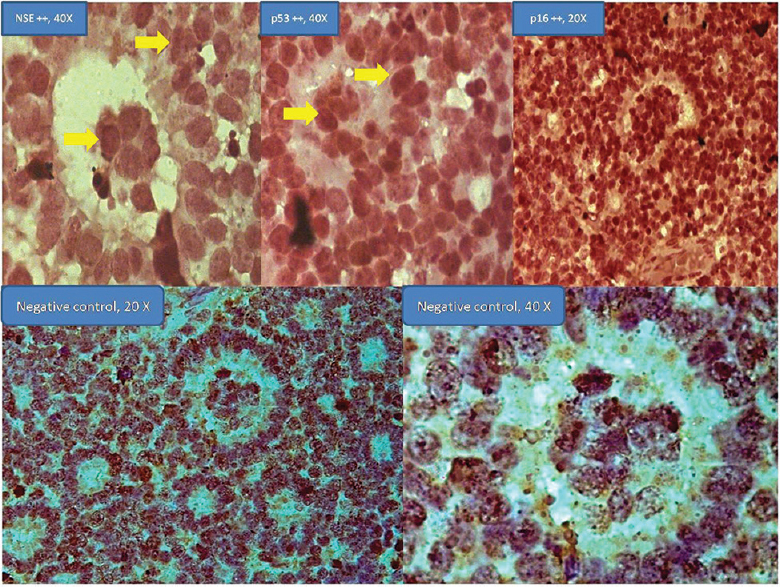
- Immunohistochemistry for neuron-specific enolase (×40), p53 (×40), and p16 (×20) shown in new rosettes retinoblastoma. Negative controls (×20 and ×40).
Discussion
IHC is a method for recognition of cellular and tissue constituent (antigens) using antigen-antibody links, the site of antibody binding being identified either by direct labelling of the antibody or by the use of secondary labelling methods23456. The recognition of specific or extremely selective cellular epitopes in routinely processed paraffin wax embedded tissue with an antibody and appropriate labelling arrangement is a routine procedure in most cellular pathology laboratories in the world789. The IHC has different facets in diagnostic areas for determining the nature of protein deposits in the tissue. There has been a significant advancement in IHC technology, but newer and simpler methods like kit procedure has come in a big way to replace the tedious and complicated techniques of antibody-antigen binding recognition23456789.
A total 645 tumours were seen in two years, and IHC was done in 87 cases In ocular surface squamous neoplasia (OSSN), subtle forms of invasive carcinomas with breach of basement membrane were picked up better by CK and distinguished the cellular subtype. In some instances, Ki 67 index greater than 60 per cent was found to be a strong predictor of poor survival and local spread. Squamous cell carcinoma was the highest in the series. . Among the NHL, most were low-grade B-cell lymphoma of mucosal-associated lymphocytic tumour type and a similar observation was noted earlier39. T-cell NHL was seen in one case. In all benign cases/IOID, the infectious panel was ruled out. Benign tumours were found in 449 samples in the study period. Among the benign tumours, three cases of orbital haemangiopericytoma were seen and two cases of schwannoma were diagnosed.
In intraocular tumours, IHC was done in 13 cases, of which six were in RB specimen and four in choroidal melanoma specimen. In RB, IHC was seen in the tumours with new rosettes, which were previously described by the authors10. Various markers (NSE, p53, p16) showed positivity in the tumour cells along with high-risk factors10. The utility of IHC in clinical conditions such as RB could be in demarcating the high-risk factor such as optic nerve invasion. In the present study, two cases of optic nerve invasion were seen. One was pre-laminar and the other one was post-laminar and the cut end was involved. Sometimes, the round cells of RB are better stained with NSE. For choroidal melanoma, we had an index case where the optic nerve invasion was better taken up by HMB-45.
For the strength of the study, internal quality control was done for various markers in IHCs. All measures were taken to ensure the reliability of investigations right from the selection of test samples, appropriate analysis, recording and reporting of the samples to the clinicians and oncologist for appropriate actions111213. The study was based on tumours of eye and adnexa, which were relatively in small number, similar to other studies141516171819202122232425. One of the shortcomings of the study was its small sample size as ocular and the adnexal tumours are rare in presentation compared to other tumours of the body.
In conclusion, IHC was useful in our study to correctly diagnose various ophthalmic tumours in addition to histopathological evidence. Some of the tumours had specific markers positivity which differentiated them from closely related tumours. IHC can be carried out by a variety of methods and some of the methods practiced are time taking and tedious. In our study, kit methods were used which were found to be simpler and less time-consuming.
Acknowledgment
Authors acknowledge Drs. S. Krishna Kumar, Jyotirmay Biswas and Ms. Nalini Venkatesan, Sankara Nethralaya, Chennai, and Drs. Diva Kant Misra and Akanksha Koul, Sankaradeva Nethralaya, Guwahati, India for technical support.
Financial support & sponsorship: Authors acknowledge the Indian Council of Medical Research, New Delhi, and Sri Kanchi Sankara Health and Education Foundation for financial support
Conflicts of Interest: None.
References
- Profile of ocular and adnexal tumours at a tertiary institute of Northeast India. Orbit. 2014;33:412-5.
- [Google Scholar]
- Small round cell tumor with divergent differentiation: Cytologic, histologic, and ultrastructural findings. Diagn Cytopathol. 1994;11:159-64.
- [Google Scholar]
- Breast carcinoma with positive results for melanoma marker (HMB-45).HMB-45 immunoreactivity in normal and neoplastic breast. Am J Clin Pathol. 1989;92:491-5.
- [Google Scholar]
- Immunohistochemistry and related marking techniques. In: AndersonŨs pathology (10th ed). St. Louis: Mosby; 1996. p. :136-75.
- [Google Scholar]
- Immunohistopathology: A practical approach to diagnosis. In: Principles and techniques in diagnostic histopathology (2nd ed). Chicago: ASCP Press; 2003. p. :14-33.
- [Google Scholar]
- Soft tissue tumors 1995:108-33.
- Detection and clinical importance of micrometastatic disease. J Natl Cancer Inst. 1999;91:1113-24.
- [Google Scholar]
- Primary versus metastatic pulmonary adenocarcinoma: An immunohistochemical study using villin and cytokeratins 7 and 20. Appl Immunohistochem. 1996;4:86-94.
- [Google Scholar]
- Ocular adnexal lymphoma in the Northeast Indian population. Indian J Ophthalmol. 2008;56:153-5.
- [Google Scholar]
- Primary primitive neuroectodermal tumor of the orbit. Indian J Ophthalmol. 2009;57:391-3.
- [Google Scholar]
- Immunohistochemical markers of prognostic value in surgical pathology. Histol Histopathol. 1997;12:1039-55.
- [Google Scholar]
- Suppression of endogenous avidin-binding activity in tissues and its relevance to biotin-avidin detection systems. J Histochem Cytochem. 1981;29:1196-204.
- [Google Scholar]
- A retrospective analysis of primary eye cancer at the University of Alabama at Birmingham 1958-1988.Part I: Eye and orbital cancer. J Am Optom Assoc. 1991;62:815-9.
- [Google Scholar]
- Primary malignant tumours of eye and adnexa in Eastern Nepal. Clin Exp Ophthalmol. 2003;31:415-7.
- [Google Scholar]
- The incidence of retinoblastoma in the United States: 1974 through 1985. Arch Ophthalmol. 1990;108:128-32.
- [Google Scholar]
- Clinical analysis of tumors of the eye and its adnexa. Korean J Ophthalmol. 1988;2:27-31.
- [Google Scholar]
- A clinicopathological study of eyelid malignancies from central India. Indian J Ophthalmol. 2007;55:109-12.
- [Google Scholar]
- Clinicopathological analysis of malignant eyelid tumours in North-West Pakistan. J Pak Med Assoc. 2013;63:25-7.
- [Google Scholar]
- Sebaceous carcinoma of the eyelids: Personal experience with 60 cases. Ophthalmology. 2004;111:2151-7.
- [Google Scholar]






