Translate this page into:
Thiazide diuretics use & risk of falls & syncope among hypertensives: A retrospective cohort study
For correspondence: Dr Parth Anilbhai Parmar, Department of Community Medicine, Shri M. P. Shah Government Medical College, Jamnagar 361 008, Gujarat, India e-mail: parthparmar6036@gmail.com
-
Received: ,
Accepted: ,
Abstract
Background & Objectives
Although thiazide diuretics are frequently used to treat hypertension, they may also raise the risk of syncope and falls. The purpose of this study was to look at the relationship between hypertension individuals’ use of thiazide diuretics and falls or syncope.
Methods
This retrospective cohort study, conducted between March 2019 and March 2024, included 236 individuals with hypertension taking thiazides and 236 controls not taking thiazides. Data from electronic medical records were extracted, including demographic, clinical, laboratory, and outcome data. The main outcome was the occurrence of syncope episodes or falls. Logistic regression analyses examined associations between various factors and falls/syncope risk.
Results
The study included 236 study participants taking thiazides (118 men, 118 women) and 236 controls not taking thiazides (118 men, 118 women). Study participants taking thiazides had a higher prevalence of hyponatremia (57 study participants, 24.1% vs. 31 study participants, 13.1%), hypokalaemia (52 study participants, 22% vs. 32 study participants, 13.6%), hypercalcemia (37 study participants, 15.7% vs. 17 study participants, 7.2%), metabolic alkalosis (89 study participants, 37.7% vs. 52 study participants, 22%), acute kidney injury (59 study participants, 25% vs. 30 study participants, 12.7%), and chronic kidney disease (89 study participants, 37.7% vs. 59 study participants, 25%) compared to controls (all P<0.05). The prevalence of falls/syncope events was significantly higher in the thiazide group (76 study participants, 32.2%) compared to the non-thiazide group (46 study participants, 19.5%), with a P value of 0.002. Multivariate analysis showed increased falls/syncope risk with age [adjusted odds ratio (AOR)=1.38], congestive heart failure (AOR=2.12), longer thiazide duration (AOR=1.21), hyponatremia (AOR=1.68), hypokalaemia (AOR=1.72), metabolic alkalosis (AOR=1.68), acute kidney injury (AOR=1.85), and decreased eGFR (AOR=1.22 per 10 ml/min/1.73m2 decrease).
Interpretation & Conclusion
Thiazide diuretic use in hypertensive patients is related to syncope, potentially mediated by electrolyte disturbances and renal impairment. These results highlight the importance of careful monitoring and individualized treatment approaches when prescribing thiazide diuretics to hypertensive patients.
Keywords
Electrolyte disturbances
falls
hypertension
renal impairment
syncope
thiazide diuretics
Hypertension is the most common chronic disease affecting large percentages of the human population worldwide1. In such conditions, thiazide diuretics are commonly prescribed either as monotherapy or in combination with other antihypertensive classes2. Thiazide diuretics, although generally effective and well-tolerated, could cause numerous adverse drug reactions, including electrolyte disturbances, metabolic disorders, and impaired renal function3,4. These may lead to falls and syncope, especially in those cases with advanced age and comorbidities5. The potential mechanisms for increased risk may be due to electrolyte disturbances such as hyponatremia, hypokalaemia, hypercalcemia, metabolic alkalosis, and acute kidney injury (AKI)6,7. There have been several studies on the association between the risk of falls and syncope related to the use of thiazide diuretics in the general population, particularly in the elderly8,9. However, there is limited evidence to address this association in hypertensive patients, specifically who often possess unique clinical profiles and might be particularly vulnerable to the adverse effects of thiazide diuretics given their underlying condition and potential concomitant use of other medications. The knowledge of the precise relationship that exists between thiazide diuretics use and the risk of falls and syncope will rather inform clinical decisions on how to minimize adverse events. Identifying the risk factors and populations of vulnerable patients will help health providers focus interventions on close follow up, alternative treatment, or specific prophylactic measures to enhance the patients’ safety and quality of care. This study aimed to investigate the relationship between diuretic use and the occurrence of falls and syncope in hypertensive patients. We further investigated whether electrolyte disturbances, impairment of renal function, and other clinical factors might modulate the risk of falls and syncope in these patients.
Materials & Methods
Study design and setting
This retrospective cohort study was conducted at the department of General Medicine, Guru Gobind Singh Government Hospital and Shri M. P. Shah Government Medical College, Jamnagar, Gujarat between March 2019 and March 2024. The Institutional Ethics Committee examined and approved the study protocol.
Eligible population
All adult individuals aged ≥18 yr with a prescription of thiazide diuretic agents for the treatment of hypertension within the study period were eligible. Subjects were identified from the EMR system with the help of relevant prescription and billing codes. Individuals with incomplete medical records or who were lost to follow up were excluded from the study.
Sample size calculation
In this study, we assumed a thiazide diuretic use and falls/syncope events association of a moderate effect size-odds ratio of 1.5, based on previous literature. For these estimated parameters and considering a desired power of 80 per cent at a two-sided alpha level of 0.05, we estimated a required sample size of 472 (236 in each group)10.
Sampling strategy
Consecutive inclusion of the study participants receiving thiazide diuretic medication who were enrolled for hypertension was considered from March 2019 to March 2024 at the Guru Gobind Singh Government Hospital and Shri M P Shah Government Medical College, Jamnagar, Gujarat. This was done to reduce the possibility of selection bias and guarantee that the sample was representative of the target population (individuals with hypertension on thiazide diuretics). The steps performed for this sampling technique are described in the figure.
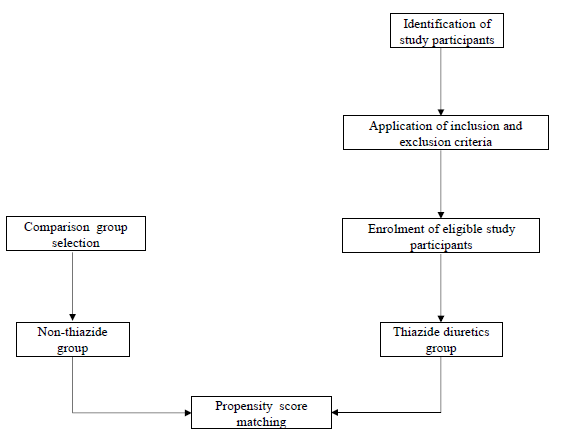
- Steps for sampling strategy.
Data collection
Trained personnel took all data from the electronic medical record (EMR) system. The collected data included age, gender, duration of thiazide use (most common usage -a daily dose of 12.5 mg Chlorthalidone, taken as one tablet in the morning), range of thiazide doses (12.5mg to 100mg/day), duration of comorbidities, body mass index (BMI), and concomitant medication use [angiotensin-converting enzyme (ACE) inhibitors/angiotensin-receptor blockers (ARBs), beta-blockers, and calcium channel blockers].
Laboratory data, including serum electrolyte levels (sodium, potassium, and calcium), renal function tests (serum urea, creatinine, and estimated glomerular filtration rate [eGFR]), and the presence of electrolyte disturbances (hyponatremia, hypokalaemia, hypercalcemia, and metabolic alkalosis) were also collected.
The estimated glomerular filtration rate (eGFR) was derived using reference equation11.
The primary outcome of interest was the occurrence of falls or syncope events during the study period. Falls and syncope events were identified from the EMR system using relevant diagnostic codes and physicians’ notes.
Definitions
Hyponatremia was defined as serum sodium concentration being <135 mmol/l and Hypokalaemia was defined as serum potassium being <3.5 mmol/land classified12,13. Hypercalcemia was defined as serum calcium level >10.2 mg/dl14. Metabolic alkalosis was defined as a serum bicarbonate level >28 mmol/l15. Acute kidney injury (AKI) and chronic kidney disease (CKD) were defined according to the Kidney Disease Improving Global Outcomes (KDIGO) guidelines16.
Statistical analysis
Descriptive statistics were used to summarise baseline characteristics. Differences between thiazide and non-thiazide groups were assessed using unpaired t-tests for continuous variables and chi-square tests for categorical variables. Logistic regression analyses examined associations between thiazide use, electrolyte disturbances, renal function, and the risk of falls/syncope events. Multivariate models adjusted for age, gender, comorbidities, and concomitant medications. All analyses were performed using R software (R Core Team, Vienna, Austria 4.2.1).
Results
The study included 236 study participants taking thiazide diuretics and 236 study participants not taking thiazides (Table I). The mean age of study participants in the thiazide group (68.4±9.6 yr) was similar to the non-thiazide group (67.8±10.2 yr), with no significant difference (P=0.542). The gender distribution was balanced, with 50 per cent males in both groups. The mean duration of thiazide use in the thiazide group was 22.8±15.2 months. Study participants in the non-thiazide group, by definition, had no thiazide use. The mean duration of hypertension was similar between the two groups (thiazide group: 9.6±6.4 yr; non-thiazide group: 8.8±5.6 yr, P=0.168). Diabetes mellitus (7.2±4.6 yr vs. 6.8±4.2 yr, P=0.336) and congestive heart failure (5.4±3.2 yr vs. 4.8±2.8 yr, P=0.042) were slightly higher in the thiazide group, with a statistically significant difference observed for congestive heart failure. Falls/syncope events were more in the thiazide group (32.2%) compared to the non-thiazide group (19.5%); P=0.002 .
| Variable | Study participants taking thiazide (n=236) | Study participants without thiazide (n=236) | P value |
|---|---|---|---|
| Age (yr), mean±SD | 68.4±9.6 | 67.8±10.2 | 0.542 |
| Male gender, n (%) | 118 (50%) | 118 (50%) | 1 |
| Duration of thiazide use (months), mean±SD | 22.8±15.2 | - | - |
| Duration of hypertension (yr), mean±SD | 9.6±6.4 | 8.8±5.6 | 0.168 |
| Diabetes mellitus, n (%) | 94 (39.8%) | 89 (37.7%) | 0.632 |
| Duration of diabetes mellitus (yr), mean±SD | 7.2±4.6 | 6.8±4.2 | 0.336 |
| Congestive heart failure, n (%) | 56 (23.7%) | 60 (25.4%) | 0.674 |
| Duration of congestive heart failure (yr), mean±SD | 5.4±3.2 | 4.8±2.8 | 0.042* |
| BMI (kg/m2), mean±SD | 29.2±5.2 | 28.6±4.8 | 0.208 |
| Other medication usage, n (%) | |||
| ACE inhibitors/ARBs | 134 (56.8%) | 128 (54.2%) | 0.574 |
| Beta-blockers | 89 (37.7%) | 84 (35.6%) | 0.622 |
| Calcium channel blockers | 75 (31.8%) | 69 (29.2%) | 0.542 |
| Falls/Syncope events, n (%) | 76 (32.2%) | 46 (19.5%) | 0.002* |
P*<0.05. BMI, body mass index; SD, standard deviation; ACE, angiotensin-converting enzyme
Study participants taking thiazides had a higher prevalence of electrolyte disturbances compared to that in controls (Table II). Hyponatremia was observed in 57 (24.1%) study participants in the thiazide group versus 31 (13.1%) in the non-thiazide group (P=0.04). Hypokalaemia was present in 52 (22%) thiazide users compared to 32 (13.6%) non-users (P=0.02). Hypercalcemia was found in 37 (15.7%) study participants taking thiazides versus 17 (7.2%) not taking thiazides (P=0.006). Metabolic alkalosis was significantly more common in the thiazide group, affecting 89 (37.7%) study participants, compared to 52 (22%) in the non-thiazide group (P<0.001).
| Variable | Study participants taking thiazide (n=236) | Study participant without thiazide (n=236) | P value |
|---|---|---|---|
| Hyponatremia, n (%) | 57 (24.1%) | 31 (13.1%) | 0.04* |
| Mild (130-134 mmol/l) | 35 (61.4%) | 20 (64.5%) | 0.01* |
| Moderate (125-129 mmol/l) | 19 (33.3%) | 8 (25.8%) | 0.02* |
| Severe (<125 mmol/l) | 3 (5.3%) | 3 (9.7%) | 1.0 |
| Hypokalaemia, n (%) | 52 (22%) | 32 (13.6%) | 0.02* |
| Mild (3.0-3.5 mmol/l) | 32 (61.5%) | 16 (50%) | 0.02* |
| Moderate (2.5-2.9 mmol/l) | 12 (23.1%) | 11 (34.4%) | 0.83 |
| Severe (<2.5 mmol/l) | 8 (15.4%) | 5 (15.6%) | 0.4 |
| Hypercalcemia, n (%) | 37 (15.7%) | 17 (7.2%) | 0.006* |
| Metabolic alkalosis, n (%) | 89 (37.7%) | 52 (22%) | <0.001** |
P*<0.05,**<0.001
The severity of hyponatremia also differed between groups. In the thiazide group, 35 (61.4%) study participants had mild hyponatremia, 19 (33.3%) had moderate hyponatremia, and three (5.3%) had severe hyponatremia. In contrast, in the non-thiazide group, 20 (64.5%) had mild, eight (25.8%) had moderate, and three (9.7%) had severe hyponatremia.
Similarly, for hypokalaemia, in the thiazide group, 32 (61.5%) study participants had mild, 12 (23.1%) had moderate, and eight (15.4%) had severe hypokalaemia. In the non-thiazide group, 16 (50%) had mild, 11 (34.4%) had moderate, and five (15.6%) had severe hypokalaemia. The prevalence of hypercalcemia was significantly higher in the thiazide group (15.7%) compared to the non-thiazide group (7.2%); P=0.006. The prevalence of metabolic alkalosis was also significantly higher in the thiazide group (37.7%) compared to the non-thiazide group (22%), with a P<0.001.
Supplementary table explains the renal function and markers.
Table III presents that increasing age was associated with falls/syncope in the thiazide group. For every one-year increase in age, the adjusted odds of falls/syncope increased by 38 per cent [adjusted odds ratio (AOR)=1.38, 95% confidence interval (CI): 1.14-1.67, P=0.001]. Study participants with congestive heart failure had a significantly higher risk of falls/syncope while taking thiazides, with an adjusted odds ratio of 2.12 (95% CI: 1.28-3.51, P=0.003) compared to those without congestive heart failure.
| Variable | Events of falls/syncope | Crude OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|---|
| Age (yr) | |||
| <65 | 25/180 (13.9%) | Reference | Reference |
| ≥65 | 97/292 (33.2%) | 3.08 (1.89-5.02)** | 1.38 (1.14-1.67)* |
| Congestive heart failure | |||
| No | 78/356 (21.9%) | Reference | Reference |
| Yes | 44/116 (37.9%) | 2.18 (1.39-3.42)** | 2.12 (1.28-3.51)** |
| Hyponatremia | |||
| No | 86/384 (22.4%) | Reference | Reference |
| Yes | 36/88 (40.9%) | 2.40 (1.47-3.91)** | 1.68 (1.03-2.74)* |
| Hypokalaemia | |||
| No | 92/388 (23.7%) | Reference | Reference |
| Yes | 30/84 (35.7%) | 1.79 (1.08-2.96)* | 1.72 (1.20-3.07)* |
| Metabolic alkalosis | |||
| No | 75/331 (22.7%) | Reference | Reference |
| Yes | 47/141 (33.3%) | 1.71 (1.10-2.63)* | 1.68 (1.08-2.94)* |
| Acute kidney injury | |||
| No | 88/383 (23%) | Reference | Reference |
| Yes | 34/89 (38.2%) | 2.07 (1.27-3.38)* | 1.85 (1.04-3.29)* |
| Estimated GFR (per 10 mL/min/1.73m2 decrease) | - | 1.34 (1.18-1.52)* | 1.22 (1.07-1.39)* |
P*<0.05,**<0.001. OR, odds ratio; GFR, glomerular filtration rate; CI, confidence interval
Electrolyte disturbances, such as hyponatremia and hypokalaemia, were associated with falls/syncope in the thiazide group. The presence of metabolic alkalosis was also a significant risk factor. Study participants with (AKI) had an increased risk of falls/syncope while taking thiazides, with an AOR of 1.85 (95% CI: 1.04-3.29, P=0.036) compared to those without AKI. The estimated glomerular filtration rate (eGFR) was inversely associated with the risk of falls/syncope (AOR =1.22, 1.07-1.39, P=0.003).
Although CKD and hypercalcemia had significant crude odds ratios (CORs) for falls/syncope, their associations were not statistically significant after adjusting for other factors in the multivariate logistic regression analysis. Overall, this logistic regression analysis identified several risk factors, including age, congestive heart failure, electrolyte disturbances (hyponatremia, hypokalaemia, and metabolic alkalosis), AKI, and decreased renal function, that were independently associated with an increased risk of falls/syncope in study participants taking thiazides.
Table IV presents a comprehensive analysis of the association between thiazide diuretic use, its duration, and the risk of falls/syncope events in hypertensive individuals. The table has two main sections: overall thiazide use and duration. The first section shows that among study participants not taking thiazides, 46 out of 236 (19.5%) experienced falls or syncope, while in the thiazide group, this increased to 76 out of 236 (32.2%). After adjusting for potential confounders, the association remained significant, with an AOR of 1.85 (95% CI: 1.18-2.9).
| Variable | Events of falls/syncope | Crude OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|---|
| Thiazide use | |||
| No thiazide | 46/236 (19.5%) | Reference | Reference |
| Thiazide use | 76/236 (32.2%) | 1.96 (1.29-2.99)* | 1.85 (1.18-2.9)* |
| Duration of thiazide use | |||
| No use | 46/236 (19.5%) | Reference | Reference |
| <12 months | 22/80 (27.5%) | 1.57 (0.87-2.82) | 1.48 (0.81-2.7) |
| 12-24 months | 26/78 (33.3%) | 2.06 (1.17-3.64)* | 1.92 (1.07-3.45)* |
| >24 months | 28/78 (35.9%) | 2.31 (1.32-4.05)** | 2.15 (1.21-3.83)** |
| Per 12-month increase | - | 1.32 (1.14-1.53)* | 1.21 (1.04-1.41)* |
P*<0.05,**<0.001. Note: Adjusted odds ratios (AOR) were calculated using multivariate logistic regression models adjusting for the following covariates: Age, gender, body mass index (BMI), duration of hypertension, presence of diabetes mellitus, presence of congestive heart failure, estimated glomerular filtration rate (eGFR), concomitant use of other antihypertensive medications (ACE inhibitors/ARBs, beta-blockers, calcium channel blockers), serum sodium, potassium, and calcium levels, presence of metabolic alkalosis
The second section of the table presents the impact of thiazide use duration on falls/syncope risk. A clear dose-response relationship is evident, with longer durations of thiazide use associated with progressively higher risks. Compared to no thiazide use, study participants using thiazides for less than 12 months showed a non-significant increase in risk (AOR: 1.48, 95% CI: 0.81-2.7). However, for those using thiazides for 12-24 months and more than 24 months, the risk became statistically significant, with AORs of 1.92 (95% CI: 1.07-3.45) and 2.15 (95% CI: 1.21-3.83), respectively.
Discussion
The present study has identified the potential risks related to thiazide diuretic use in hypertensive individuals. This observation is consistent with previous studies reporting an elevated risk of falls and syncope related to thiazide diuretic use in the general population8,9.
Firstly, the higher prevalence of electrolyte disturbances, such as hyponatremia, hypokalaemia, and hypercalcemia, among study participants taking thiazide diuretics is a well-established adverse effect of these medications17-19. These electrolyte imbalances can lead to various physiological consequences, including neurological impairments, muscle weakness, and cardiovascular dysregulation, which may predispose patients to falls and syncope events20,21.
Additionally, we observed a higher prevalence of metabolic alkalosis in the thiazide group, another known adverse effect of these diuretics7. Metabolic alkalosis can contribute to impaired neuromuscular function, altered mental status, and increased risk of arrhythmias, further exacerbating the risk of falls and syncope22.
The study also revealed a higher prevalence of AKI and CKD among study participants taking thiazide diuretics. Renal impairment can lead to various metabolic and electrolyte disturbances and impaired fluid and electrolyte homeostasis, which may contribute to an increased risk of falls and syncope23,24.
Furthermore, the logistic regression analysis identified several independent risk factors for falls and syncope in study participants taking thiazide diuretics. These included increasing age, congestive heart failure, longer duration of thiazide use, hyponatremia, hypokalaemia, metabolic alkalosis, AKI, and decreased estimated glomerular filtration rate (eGFR). These findings highlight the importance of considering individual patient characteristics, comorbidities, and potential drug-related adverse effects when prescribing thiazide diuretics, particularly in vulnerable patient populations.
Our findings of increased risk of falls and syncope associated with thiazide diuretic use are consistent with several previous studies. The present study also provided new insights into potential mechanisms. A large retrospective cohort study by Ravioli et al10 (2021) involving 1604 patients found such an association similar to the AOR of 1.96 (95% CI 1.28-3.01) for falls/syncope events that we estimated.
A meta-analysis by Bai et al25 (2023) of 13 studies that were meta-analysed found the same. Our findings of increased risk associated with hyponatremia and hypokalaemia are novel contributions to the literature, as previous studies have not specifically examined these electrolyte abnormalities related tofall- risk in thiazide users.
Interestingly, prospective research by Bakar et al26 (2021) discovered that older persons using diuretics (AOR 2.803, 95% CI 1.418, 5.544) and polypharmacy (AOR 2.513, 95% CI 1.339, 4.718) had a greater risk of falling. However, no correlation was found between an increased occurrence of falls and older persons, especially those taking more anti-hypertensive drugs26.
A prior meta-analysis found that taking thiazides was linked to a lower incidence of fracture in case-control studies but not in cohort studies. Selection and recollection biases are two types of inherent biases that may be responsible for the relationships shown in case-control studies. Therefore, using thiazides might not prevent fractures27. While our study demonstrated associations between thiazide use and falls/syncope, several alternative explanations should be considered. Confounding by indication may play a role, as patients on thiazides could have more severe hypertension or other comorbidities that independently increase the risk of falls. Additionally, unmeasured confounders such as cognitive function, frailty, or physical activity levels could influence thiazide prescription and the risk of falls. The potential for detection bias should also be acknowledged, as study participants taking thiazides may be monitored more closely, leading to increased identification of falls/syncope events.
Future research should focus on prospective studies to further elucidate the causal relationship between thiazide diuretic use and falls and syncope events and the underlying mechanisms involved. Additionally, studies investigating the efficacy of preventive interventions and alternative treatment strategies in high-risk patients would be valuable in improving patient safety and clinical outcomes.
The present study included 152 study participants taking thiazide diuretics and 352 study participants not taking thiazides, providing sufficient statistical power to detect significant associations. Moreover, in this study, detailed demographic, clinical, laboratory, and outcome data were collected, allowing for a thorough investigation of potential risk factors and confounders. The use of propensity score matching in the control group further helped reduce potential selection bias and ensure comparability between the two groups. The inclusion of multivariate logistic regression models allowed for the adjustment of potential confounding factors, providing more reliable estimates of the associations between thiazide use and the risk of falls/syncope.
Despite the above strengths, there were some limitations. As a retrospective study, the data were collected from existing medical records in the present investigation, which may be subject to potential inaccuracies or missing information. The investigation was located in one centre study. Notably, the study did not provide details on the severity or consequences of the falls and syncope events, which could have been useful for assessing their clinical impact. Despite the comprehensive data collection and multivariate analysis, there may be additional, unmeasured confounding factors that could influence the observed associations. The unmeasured confounders like diet, physical activity, depression, and cognitive impairment were not accounted for and might have influenced the results. Finally, the study did not specify the duration of follow up, which could affect the capture of long-term outcomes or adverse events.
Overall, our study demonstrated a significant increase in falls and syncope events among patients taking thiazide diuretics compared to those who were not on these medications. We identified several independent risk factors, including increasing age, congestive heart failure, longer duration of thiazide use, electrolyte imbalances (hyponatremia, hypokalaemia, and metabolic alkalosis), acute kidney injury, and decreased renal function. These results highlighted the importance of careful monitoring and individualized treatment approaches when prescribing thiazide diuretics to hypertensive patients. While these medications remain valuable for hypertension management, our findings underscore the need for regular electrolyte and renal function monitoring and the implementation of fall prevention strategies in high-risk patients.
Financial support & sponsorship
None.
Conflicts of Interest
None.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- Hypertension prevalence among adults aged 18 and over: United States, 2017-2018. NCHS Data Brief. 2020;364:1-8.
- [Google Scholar]
- 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American college of cardiology/American heart association task force on clinical practice guidelines. J Am Coll Cardiol. 2018;71:e127-e248.
- [CrossRef] [PubMed] [Google Scholar]
- Diuretic initiation and the acute risk of hip fracture. Osteoporos Int. 2013;24:689-95.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Thiazide Diuretics. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2025.
- [Google Scholar]
- Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701-7.
- [CrossRef] [PubMed] [Google Scholar]
- Thiazide-associated hyponatremia: Clinical manifestations and pathophysiology. Am J Kidney Dis. 2020;75:256-64.
- [CrossRef] [PubMed] [Google Scholar]
- Metabolic complications associated with use of thiazide diuretics. J Am Soc Hypertens. 2007;1:381-92.
- [CrossRef] [PubMed] [Google Scholar]
- The association between diuretics and falls in older adults: A systematic review and meta-analysis. Geriatr Nurs. 2023;52:106-14.
- [CrossRef] [PubMed] [Google Scholar]
- Diuretics, SGLT2 inhibitors and falls in older heart failure patients: To prescribe or to deprescribe? A clinical review. Eur Geriatr Med. 2023;14:659-74.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Risk of electrolyte disorders, syncope, and falls in patients taking thiazide diuretics: Results of a cross-sectional study. Am J Med. 2021;134:1148-54.
- [CrossRef] [PubMed] [Google Scholar]
- A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical aspects of symptomatic hyponatremia. Endocr Connect. 2016;5:R35-R43.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2024;105:S117-S314.
- [CrossRef] [PubMed] [Google Scholar]
- KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120:c179-84.
- [CrossRef] [PubMed] [Google Scholar]
- Thiazide-associated hyponatremia, report of the hyponatremia registry: An observational multicenter international study. Am J Nephrol. 2017;45:420-30.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Impact of diuretic therapy-associated electrolyte disorders present on admission to the emergency department: A cross-sectional analysis. BMC Med. 2013;11:83.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Thiazides and the risk of hypokalemia in the general population. J Hypertens. 2014;32:2092-7. discussion 2097
- [CrossRef] [PubMed] [Google Scholar]
- Hypokalemia and sudden cardiac death. Exp Clin Cardiol. 2010;15:e96-9.
- [PubMed] [PubMed Central] [Google Scholar]
- Hyponatremia is associated with worse outcomes from fall injuries in the elderly. Int J Environ Res Public Health. 2017;14:460.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Timing of onset of CKD-related metabolic complications. J Am Soc Nephrol. 2009;20:164-71.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Metabolic alkalosis in patients with renal failure. Nephrol Dial Transplant. 2003;18:2442-8.
- [CrossRef] [PubMed] [Google Scholar]
- The association between diuretics and falls in older adults: A systematic review and meta-analysis. Geriatr Nurs. 2023;52:106-114.
- [CrossRef] [PubMed] [Google Scholar]
- Older adults with hypertension: Prevalence of falls and their associated factors. Int J Environ Res Public Health. 2021;18:8257.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Thiazide use and fracture risk: An updated Bayesian meta-analysis. Sci Rep. 2019;9:19754.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






