Translate this page into:
Single visit approach for management of cervical intraepithelial neoplasia by visual inspection & loop electrosurgical excision procedure
Reprint requests: Dr. Neerja Bhatla, Professor, Department of Obstetrics & Gynaecology, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110 029, India e-mail: neerja.bhatla07@gmail.com
-
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Developing a feasible and sustainable model of cervical cancer screening in developing countries continues to be a challenge because of lack of facilities and awareness in the population and poor compliance with screening and treatment. This study was aimed to evaluate a single visit approach (SVA) for the management of cervical intraepithelial neoplasia (CIN) using visual inspection with acetic acid (VIA) and Lugol's iodine (VILI) along with loop electrosurgical excision procedure (LEEP) in women attending Gynaecology OPD in a tertiary care hospital in north India.
Methods:
In this hospital-based study, 450 women receiving opportunistic screening by conventional Pap cytology were also screened by VIA and VILI. VIA/VILI positive cases underwent same-day colposcopy and biopsy of all lesions. If the modified Reid score was >3, the patient underwent LEEP at the same visit.
Results:
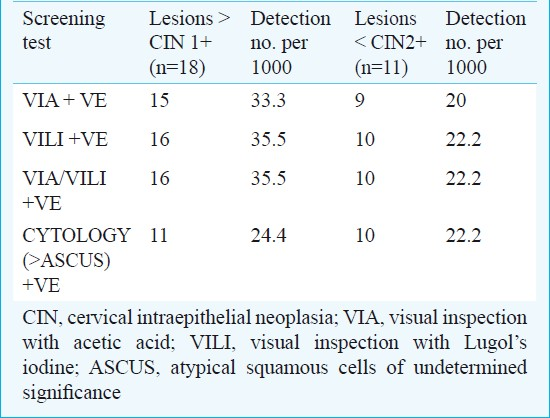
Of the 450 women screened, 86 (19.1%) and 92 (20.5%) women were VIA and VILI positive, respectively. Detection rates of VIA, VILI and cytology findings at ASCUS threshold were 33.3, 35.5 and 24.4 per 1000, women, respectively to detect a lesion >CIN1. For detection of CIN2+ lesion, detection rates of VIA, VILI and cytology were 20, 22.2 and 22.2 per 1000 women, respectively. Sixteen patients with Reid score >3 underwent the See-and-treat protocol. The overtreatment rate was 12.5 per cent and the efficacy of LEEP was 81.3 per cent. There were no major complications.
Interpretation & conclusions:
The sensitivity of VIA/VILI was comparable to cytology. A single visit approach using visual screening methods at community level by trained paramedical personnel followed by a combination of ablative and excisional therapy can help to decrease the incidence of cervical neoplasia.
Keywords
Acetic acid
cervical cancer
cervical intraepithelial neoplasia
loop electrosurgical excision procedure
Lugol's iodine
see-and-treat
Cervical cancer is the commonest cause of death from cancer in India and second most common worldwide amongst females. Eighty per cent of the estimated 529,400 new cases and 274,800 deaths due to cervical cancer in 2008 worldwide were in developing countries, with an estimated 1,34,420 new cases and 72,825 deaths in India1. While cervical cancer occupies either the top or second rank among cancers in developing countries, it does not find a place in the top five leading cancers in women in affluent nations2. This is because organized cytology-based mass screening programmes cannot be implemented in developing countries due to logistic reasons. Cervical cancer incidence rates have been decreasing in China and Japan as a result of screening programmes, creation of registries, and health education. The age-adjusted incidence rate in China was 29.0 in 1973 versus 5.6 in 2002; corresponding rates for Japan were 17.3 versus 6.73. In India, all the urban Population Based Cancer Registries at Bangalore, Bhopal, Chennai, Delhi and Mumbai have shown a statistically significant decrease in incidence rates of this site of cancer. Since over 70 per cent of the Indian population resides in the rural areas, cancer cervix still continues to be the number one cancer4.
Traditionally, a 3-step approach is followed for detection and management of premalignant lesions: (i) Pap smear; (ii) colposcopy of abnormal Pap cases and directed biopsy if indicated; and (iii) further treatment of abnormal cases. These multiple visits are associated with a high rate of loss to follow up and increased costs for poor women5. Moreover, patients may suffer anxiety while awaiting the test results in the interim period. The single visit approach (SVA) has been described in women presenting with abnormal cytology, combining colposcopy with loop electrosurgical excision procedure (LEEP)5–7. In India, Pap smear facilities are largely restricted to urban areas only. Since visual inspection with acetic acid (VIA) and with Lugol's iodine (VILI) have been shown to be a feasible alternative to cytology in low resource settings89, in the present study we investigated the place of single visit approach (SVA) combining VIA/VILI, colposcopy and LEEP in women suspected to here carvical neoplasia to decrease the overall costs, provide adequate treatment and minimize loss-to-follow up in a tertiary care hospital in north India.
Material & Methods
Study design: This cross-sectional study was carried out in the Gynecology Outpatient Department (OPD) of All India Institute of Medical Sciences (AIIMS), New Delhi, from May 2005 to May 2007. Sexually active, parous women attending Gynaecology OPD were invited to participate in this study. The inclusion criteria were: at least one live issue; intact uterus; advised opportunistic Pap smear screening because of gynaecological symptoms; and willing for single-visit management and follow up. Exclusion criteria were: currently pregnant /< 3 months post-partum, bleeding disorders, obvious growth on cervix suggestive of malignancy, acute cervicitis, previous history of any procedure on cervix and allergy to local anaesthetics. Informed written consent was taken from all women. The study protocol was approved by the Institute Ethics Committee.
A detailed medical and gynaecological history was taken and general physical examination was performed. All women underwent Pap smear collection using an Ayre's spatula and an endocervical brush, followed by VIA and VILI by a trained paramedical worker as per IARC criteria810. VIA positivity was defined as appearance of acetowhite areas in the transformation zone close to squamocolumnar junction or the os. The cervix was examined under bright light source such as VIA light source or halogen focus lamp. VILI was considered positive if there were thick, dense, bright, mustard yellow or saffron-yellow well defined iodine non-uptake areas touching the squamocolumnar junction were identified. All VIA/VILI positive cases underwent colposcopy with directed cervical punch biopsy from all abnormal lesions. Patients underwent LEEP also, on a day-care basis, if the colposcopic Reid score index was >3 (but not frank cancer), with the entire transformation zone (TZ) and limit of the lesion visualized. VIA/VILI negative cases reported to have an abnormal Pap smear (>ASCUS) were called for colposcopy later and managed as per routine protocol.
LEEP was carried out as a day-care procedure in the minor operation theatre using universal aseptic precautions after informed written consent. The woman was placed in lithotomy position, an insulated Graves’ speculum inserted and cervix and upper vagina was painted with Lugol's iodine. Circumferential cervical block was given using 1 per cent lidocaine. Short lasting intravenous sedation was given to women who so demanded. Loops used for LEEP were made of 0.2 mm hard stainless steel or titanium of diameters ranging from 1-3 cm. Depending on the loop size, a power setting 50-55 watts of blend cutting plus coagulation current was used for excision. An attempt was made to remove entire involved lesion in a single pass moving from right to left. If endocervical excision was needed, a smaller loop (usually 0.8 cm in width) was used for second pass, removing the region around the endocervical canal in a “top hat” fashion. The power setting was lowered when using the smaller loop.
Bleeding, a major possible complication, was assessed on the basis of amount of blood loss and haemostatic agent required intraoperatively. Haemostasis was first attempted by the routine use of roller ball coagulation using 50 mV current. If this failed, Monsel's paste was applied. If bleeding persisted, packing was done with roller gauze soaked in povidone iodine. In case of a spurting vessel not controlled by cautery, a 2-0 chromic catgut suture was used.
Follow up was at one week for review of the histopathology report, and at one month to examine the cervix and ask the patient about problems faced, if any. The further plan of management was discussed with the patient.
Statistical analysis: The data were analyzed using the software SPSS 11.0 STATA software (STATA, College station, TX, USA). Detection rates per 1000 women were calculated for the various cervical cancer screening techniques (VIA, VILI and Pap at ASCUS threshold) using histopathology of the punch biopsy/ LEEP specimen as the reference standard.
Results
A total of 450 women were screened. The mean age was 36 ± 7.5 yr (range 20-70 yr) with the majority (n= 212, 47.1%) between 30 to 40 yr. The parity ranged from 1 to 6. Most women were para 3 (n=196, 43.6%) and para 2 (n=177, 39.3%). The mean parity of women with no dysplasia, cervical intraepithelial neoplasia l (CIN 1) and CIN 2/3 was 2.6, 3.8 and 4.5, respectively. The difference in parity among women with and without dysplasia was not significant but the difference between women with LSIL and HSIL was significant (P<0.001).
Discharge per vaginum was the most common complaint, seen in 302 (67.1%) women. Other presenting complaints included menstrual disturbances in 44 women (9.8%) and pain abdomen in 51 (11.3%), while 53 (11%) were asymptomatic. The chief complaint of women with CIN 2 or higher grade lesion was either foul smelling discharge per vaginum or post-coital bleeding.
VIA/VILI: All 450 patients underwent VIA and VILI as per the criteria laid down by the International Agency for Research on Cancer (IARC)810. Eighty six (19.1%) and 92 (20.5%) women were VIA and VILI positive, respectively, of whom 71 (15.8%) were positive for both VIA and VILI, while 107 (23.7%) women were positive on either of the tests. The detection rates of VIA and VILI for detection of CIN 1 and CIN 2+ disease are shown in Table I.
Pap smear: The Pap smear was inflammatory in 347(77.1%) women, with associated infection in 12 cases (HPV changes in 9, Trichomonas vaginalis in 2, granulomatous changes suggestive of tuberculosis in1. Pap smear was considered abnormal if the report showed ASCUS, AGUS or worse. Thirty six (8%) smears were abnormal: ASCUS - 7, AGUS - 1, LSIL - 10, HSIL - 15 and malignancy - 3. Of these, six (1.33%) were in the age group <30 yr (ASCUS - 2, LSIL - 1 and HSIL - 3).
The detection rate of Pap smear to detect CIN 1+ lesions was 24.4/1000 while for detection of CIN2+ lesions on histology, the detection rate was 22.2/1000 (Table I).
Colposcopy: One hundred and seven (23.7%) women were screen positive on either VIA/VILI and all agreed to same-day colposcopy. Besides these, 11 were called for colposcopy at a second-visit after a report of abnormal Pap smear was received, as per standard practice. Therefore, overall, 118 (26.2%) women underwent colposcopy and directed biopsy. Modified Reid score <2 was seen in 91 (77.1%) women, the score was >2 in 27 (22.9%) women and >3 in 18 (15.3%) women.
Eighteen (4%) biopsies showed lesion >CIN 1 (CIN 1 - 7, CIN 2 - 2, CIN 3 - 6, invasive carcinoma - 3) and CIN 2+ disease was detected in 2.4 per cent (11 women) of the total women studied.
The agreement between colposcopy and biopsy findings is shown in Table II. All CIN 2/3 lesions had Reid score >3. However, the Reid score underestimated one case of invasive carcinoma.
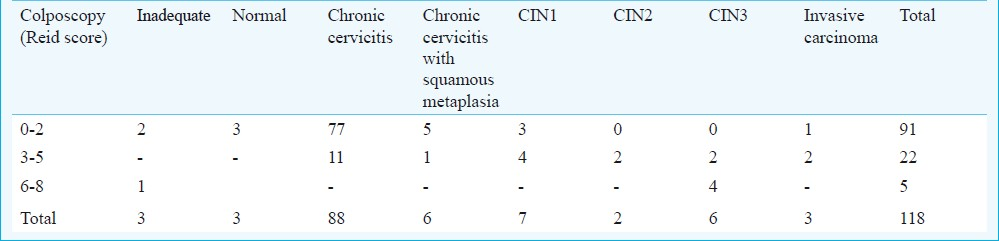
Colposcopy had a sensitivity of 78.3 per cent and specificity of 90.5 per cent to detect low-grade lesions. For detecting high-grade lesions, sensitivity improved to 92.9 per cent and specificity was 86.5 per cent. Taking a Reid score cut-off at 4 would improve specificity markedly, only missing cases of CIN 1.
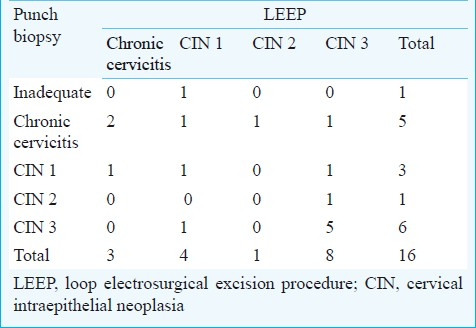
LEEP: Of the 18 women with Reid score >3, one woman was excluded from the SVA protocol as the colposcopy diagnosis was malignancy (subsequently confirmed on histology). The second excluded woman was VIA/VILI negative but had abnormal cytology. She had a second visit colposcopy and LEEP and did not fit in inclusion criteria of the present study. Among the 16 women treated using the SVA approach, the final report was chronic cervicitis in two cases, CIN 1 in four cases, CIN 2 in one and CIN 3 in nine cases. The worst histological diagnosis, whether on punch biopsy or LEEP, was taken as the final diagnosis.
The agreement between LEEP histopathology and punch biopsy in patients with Reid >3 is shown in Table III. Of the nine women with CIN 2/3 on LEEP biopsy, there was 66.7 per cent concordance with six patients having the same on punch biopsy. Thus, there were a total of 14 biopsy-proven cases of CIN 2/3 (either on punch or LEEP biopsy). Both punch and LEEP biopsy were negative in two cases, making the over-treatment rate 12.5 per cent. The remaining 14 women had a CIN 1+ lesion: 13 in the LEEP specimen and one had focal mild dysplasia (CIN 1) on punch biopsy. Margins were negative in 13 of the 16 women, positive in two and could not be commented on in one case. Two of the three women underwent hysterectomy and one was lost to follow up. Hence, the overall efficacy was 81.3 per cent.
The Fig. shows the algorithm of the study design followed in the present study and the outcomes obtained. Both VIA/VILI and Pap smear missed only one case of high grade CIN each.
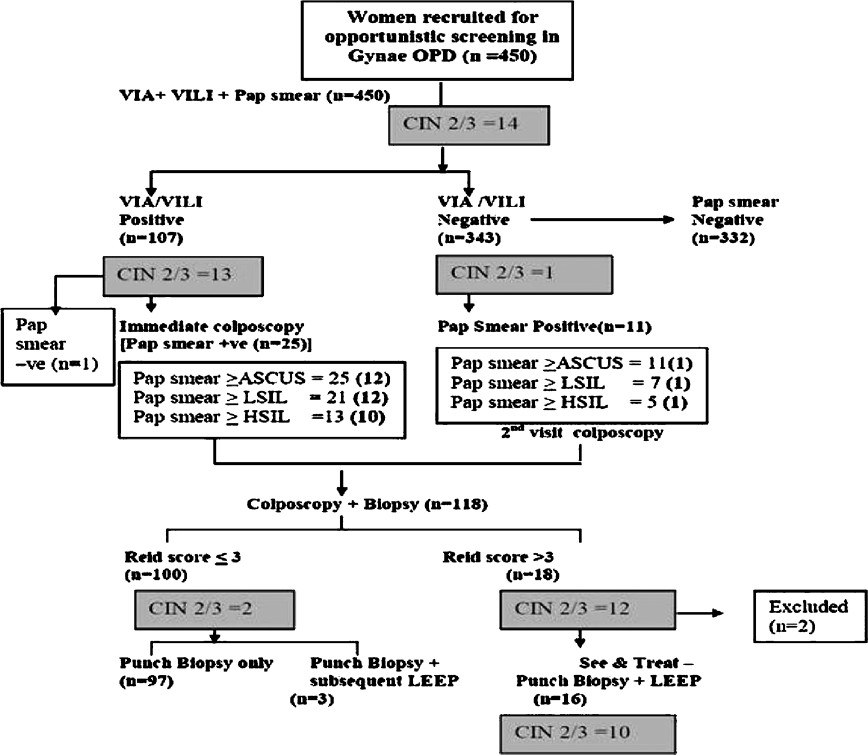
- Algorithm: Study design and outcomes. The number of cases of high grade disease (CIN 2+) diagnosed on histology in each arm is shown in the shaded boxes. VIA, visual inspection with acetic acid; VILI, visual inspection with Lugol's iodine; CIN, cervical intraepithelial neoplasia; ASCUS, atypical squamous cells of undetermined significance; LSIL, low-grade squamous intraepithelial lesion; HSIL, high-grade squamous intraepithelial lesion.
Patients who underwent LEEP were assessed for minor and major complications. Minor complications noted were pain, spotting per vaginum (7/16) and discharge (3/16). There were no major complications. Significant haemorrhage did not occur in any case. Bleeding was assessed on the basis of haemostatic agent required intraoperatively. Haemostasis was achieved by the routine use of roller ball coagulation using 50 mV current in 6 patients. Monsel's paste was required in 8 (50%) women. Only one patient required suturing.
Of the 36 abnormal smears on cytology, 25 belonged to VIA/VILI positive women who had colposcopy at their first visit. Three of them had Reid score <3 but cytology was abnormal (2 LSIL, 1 HSIL). They returned for second visit colposcopy and biopsy was normal. They required LEEP in view of discrepancy between cytology and histology, but did not return for treatment. Of the 11 women who were VIA/VILI negative but had abnormal cytology, three (2 HSIL, 1 LSIL) were lost-to-follow up in the 3-step protocol. They made a second visit for colposcopy and biopsy. Biopsy report was normal in these three women. They also needed LEEP in view of discrepancy between cytology and histology, but did not return for treatment. Hence, six of the 36 women were lost-to-follow up with a rate of 16.6 per cent.
Discussion
The inability to reduce the morbidity and mortality from a preventable disease like cervical cancer continues to be an important public health problem in developing countries due to various logistic reasons9. Even if the possibility of a pre-neoplastic condition is recognized during screening, a second visit is required for colposcopy, a third visit to collect the biopsy report and further visits may be required for treatment. Thus, a minimum of three visits are required resulting in loss to follow up. This led to the development of the “See-and-treat” approach, with the aim of minimizing loss-to-follow up. It also enabled maximal utilization of scarce medical resources in remote areas. One of the main criticisms of the “See-and-treat” approach is the risk of unnecessary overtreatment11. In areas with high disease prevalence the risk of overtreatment is correspondingly low11.
The majority of reported studies on the “see-and-treat” strategy have been based on women referred to colposcopy with HSIL on cytology, which minimizes the possibility of overtreatment11–14. There was no difference in the final histological diagnosis of patients treated by conventional 3-step protocol and “See-and-treat” LEEP protocol12. Colposcopically-directed LEEP after a report of HSIL on Pap smear may actually reduce the interval between diagnosis and treatment with a similar accuracy as compared to the standard 3-step protocol12. As the major problem in the developing countries is the inability to perform universal Pap smears, this study was conducted based on the simple, low-cost, immediate result method of VIA / VILI, which makes it truly a single-session approach. There were nine cases negative on cytology but had CIN on biopsy emphasizing the validity of an alternative screening strategy. VIA/VILI can be easily performed by trained paramedical staff and has been found to be as sensitive as cytology for detection of high grade CIN in women in the reproductive age group15. Colposcopy is a good secondary testing tool to triage women found positive on visual screening tests16.
The characteristics of VIA as a screening test have been evaluated in several cross-sectional studies. Overall, the rates of VIA positivity have been reported to vary from 12-27 per cent. In a study from South Africa, only 3.1 per cent of the women screened were VIA positive, probably because of more stringent criteria - only distinct acetowhite areas were considered positive17. In an Indian study in which distinct acetowhite areas were considered positive, 9.8 per cent of the women screened were VIA positive18. In the present study, VIA positivity was 19.1 per cent, which was somewhat higher than in other studies, perhaps because the study subjects were symptomatic women seeking treatment19. We had similar experience previously in a symptomatic hospital population15. The detection rates of visual screening in a community based screening study was reported to be 3.7/1000 women for VIA and 3.3/1000 women for VILI to detect CIN 2 and CIN 3 lesion20.
There have been relatively few studies reporting VILI as a screening method compared to VIA. The sensitivity of VILI ranges from 50-90 per cent and specificity from 75-85 per cent21–24. Our study showed better results with VILI than with VIA, due to its easily recognizable colour patterns. The parallel performance results of combination of VIA and VILI have been reported to have a better positive predictive value in literature also25.
On the basis of the model depicted in the Fig, it is seen that if the entire population was subjected to VIA/VILI, about a quarter would be positive. Focusing limited Pap smear resources on this 1/4th population could identify 85.7 per cent cases of CIN at both ASCUS and LSIL cut-off, but the specificity was better at LSIL cut-off. Thus only 5.5 per cent of women need to be referred to a District Hospital to undergo colposcopy using visual screening methods for triage.
Reid score cut-off >3 was taken as the criterion for enrollment in single-session management of VIA/VILI positive cases. Of the 18 cases with Reid score >3 on colposcopy, one was VIA/VILI negative, diagnosed on the basis of an abnormal Pap smear and recalled for colposcopy, hence could not be included for SVA. Seventeen were VIA/VILI positive and eligible for the single-session “See-and-treat” protocol. One was excluded because colposcopy suggested invasive cancer. Thus 16 patients underwent LEEP as single session management. Taking Reid score of >3 as cut-off missed two (14.2%) CIN cases while allowing 85.7 per cent to be treated in a single visit approach, with only 12.5 per cent overtreatment and remarkably reducing the rate of loss to follow up (6.25%). Taking Reid=3 as cut-off would have allowed 92 per cent treatment by SVA but would increase the overtreatment rate three-fold to 36 per cent. It has been reported that if LEEP is done for pathological discrepancy between Pap smear and cervical biopsy, two-thirds of the patients will have CIN 2+. Women with previous treatment of CIN are more likely to have CIN 2+ detected on the LEEP specimen26. Hence, the level of overtreatment seen in the present study appears acceptable.
In SVA group, one woman who had positive margins failed to return after single-session management and LEEP. Thus, the loss-to-follow up rate in this group of single-session management was 6.3 per cent. This is low compared to 16.6 per cent in three step protocol. The number of cases missed by an SVA protocol based on VIA and LEEP was acceptable, taking in consideration the cost saved. Our study has important implications for the cervical cancer screening strategy in low resource countries. However, all 450 women were not biopsied due to ethical reasons leading to verification bias. Thus, the exact test characteristics could not be evaluated. Larger trials of “See-and-Treat” approach based on visual screening need to be conducted.
To conclude, LEEP is a safe and easy to learn method which can be performed as an outpatient procedure under local anaesthesia. It has an acceptable efficacy when performed at the first visit “See-and-treat” protocol. However, since it is technically more difficult than cryotherapy with more potential morbidity, it needs to be performed by a doctor while cryotherapy can be performed by a nurse. A combination of the two therapeutic methods depending on the lesion may provide the best solution for single visit approach management at the community level.
References
- Globocan 2008, Cancer incidence and mortality worldwide. In: Cancer Base no. 10. Lyon France: International Agency for Research on Cancer Press; 2010.
- [Google Scholar]
- Epidemiology of cancer of cervix: Global and national perspective. J Indian Med Assoc. 2000;98:49-52.
- [Google Scholar]
- Cancer care inequity for women in resource-poor countries. Rev Obstet Gynecol. 2010;3:122-32.
- [Google Scholar]
- One session management of cervical intraepithelial neoplasia: A solution for developing countries. Gynecol Oncol. 1996;61:11-5.
- [Google Scholar]
- Loop electrosurgical excision procedure for squamous intraepithelial lesions of cervix: Advantages and potential pitfalls. Obstet Gynecol. 1996;87:332-7.
- [Google Scholar]
- ‘See and treat’ electrosurgical loop excision of the cervical transformation. J Fam Pract. 1996;42:253-7.
- [Google Scholar]
- IARC Technical Publication, No. 41. In: A practical manual on visual screening for cervical neoplasia. Lyon, France: IARC Press; 2003.
- [Google Scholar]
- Low cost methods for secondary prevention of cervical cancer in developing countries. Niger Postgrad Med J. 2007;14:242-6.
- [Google Scholar]
- Colposcopy and treatment of cervical intraepithelial neoplasia: A beginner's manual. Lyon, France: IARC Press; 2003.
- A prospective evaluation of “see and treat” in women with HSIL Pap smear results: is this an appropriate strategy? J Low Genit Tract Dis. 2005;9:2-6.
- [Google Scholar]
- Treatment of high-grade squamous intraepithelial lesions: a “see and treat” versus a three-step approach. Eur J Obstet Gynecol Reprod Biol. 2007;131:73-5.
- [Google Scholar]
- Treatment of the patients with abnormal cervical cytology: a “see-and-treat” versus three-step strategy. J Gynecol Oncol. 2009;20:164-8.
- [Google Scholar]
- Three-step versus “see-and-treat” approach in women with high-grade squamous intraepithelial lesions in a low-resource country. Int J Gynaecol Obstet. 2009;106:202-5.
- [Google Scholar]
- Visual inspection for cervical cancer screening: evaluation by doctor versus paramedical worker. Indian J Cancer. 2004;41:32-6.
- [Google Scholar]
- Evaluation of colposcopy vs cytology as secondary test to triage women found positive on visual inspection test. Indian J Cancer. 2010;47:308-13.
- [Google Scholar]
- Acetic acid visualization of the cervix: an alternative to cytologic screening. Obstet Gynecol. 1996;88:383-6.
- [Google Scholar]
- Visual inspection of the uterine cervix after the application of acetic acid in the detection of cervical cancer and its precursors. Cancer. 1998;83:2150-6.
- [Google Scholar]
- Shanxi Province Cervical Cancer Screening Study: a cross-sectional comparative trial of multiple techniques to detect cervical neoplasia. Gynecol Oncol. 2001;83:439-44.
- [Google Scholar]
- Evaluation of cervical screening in rural North India. Int J Gynaecol Obstet. 2009;105:145-9.
- [Google Scholar]
- Visual inspection as a cervical cancer screening method in a primary health care setting in Africa. Int J Cancer. 2006;119:1389-95.
- [Google Scholar]
- IARC Multicentre Study Group on Cervical Cancer Early Detection. Accuracy of visual screening for cervical neoplasia: Results from an IARC multicentre study in India and Africa. Int J Cancer. 2004;110:907-13.
- [Google Scholar]
- Concurrent evaluation of visual, cytological and HPV testing as screening methods for the early detection of cervical neoplasia in Mumbai, India. Bull World Health Organ. 2005;83:186-94.
- [Google Scholar]
- Evaluation on the visual inspection with Lugol's iodine in cervical cancer screening program. Zhonghua Liu Xing Bing Xue Za Zhi. 2006;27:15-8.
- [Google Scholar]
- Cervical cancer screening with naked-eye visual inspection in Colombia. Int J Gynecol Obstet. 2010;109:230-4.
- [Google Scholar]
- Diagnostic loop electrosurgical excisional procedure for discrepancy: do preoperative factors predict presence of significant cervical intraepithelial neoplasia? J Low Genit Tract Dis. 2007;11:69-72.
- [Google Scholar]






