Translate this page into:
Retrospective analysis of lung function abnormalities of Bhopal gas tragedy affected population
Reprint requests: Dr Sajal De, Qr No-8, Type III, Vivekananda Block, MGIMS Campus, Sevagram 442 102, India e-mail: sajalde@yahoo.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
A large numbers of subjects were exposed to the aerosol of methyl isocyanate (MIC) during Bhopal gas disaster and lung was one of the most commonly affected organs. The aim of the present study was to analyze retrospectively the lung function abnormalities among the surviving MIC exposed population (gas victims) and to compare it with the non-MIC exposed (non gas exposed) population.
Methods:
The spirometry data of both gas victims and non gas exposed population who attended the Bhopal Memorial Hospital & Research Centre for evaluation of their respiratory complaints from August 2001 to December 2009, were retrospectively evaluated and compared.
Results:
A total 4782 gas victims and 1190 non gas exposed individuals performed spirometry during the study period. Among the gas victims, obstructive pattern was the commonest (50.8%) spirometric abnormality followed by restrictive pattern (13.3%). The increased relative risk of developing restrictive abnormality among gas victims was observed in 20-29 yr age group only (adjusted relative risk: 2.94, P<0.001). Male gas victims were more affected by severe airflow obstruction than females and the overall increased relative risk (1.33 to 1.45, P<0.001) of developing obstructive pattern among gas victims was observed.
Interpretation & conclusions:
The present study showed that the relative risk for pulmonary function abnormalities in gas victims was significantly more among those who were young at the time of disaster. Increased smoking habit among gas victims might have played an additive effect on predominance of obstructive pattern in spirometry.
Keywords
Bhopal gas tragedy
Lung function
MIC
spirometry
obstructive
respiratory
In December 1984, the residents of Bhopal at Madhya Pradesh, India experienced one of the worst chemical disasters of the world. The exact nature of the toxic substance responsible for this disaster is disputed and multiple chemical substances are attributed1. It is suspected that the disaster was mainly due to leakage of methyl isocyanate (MIC), an intermediate product in the manufacturing of carbamate pesticide from the Union Carbide plant. The MIC aerosol was also super-added with its pyrolytic products i.e. hydrogen cyanide, nitrogen oxides and carbon monoxide and contaminants such as phosgene and monomethylamine which were also used for manufacturing of MIC2.
Eyes and respiratory system were mainly affected by the MIC. Acute respiratory symptoms were primarily due to inhalation of volatile and irritant fumes of MIC causing severe necrotizing lesions on the lining of the upper and lower respiratory tract3. Most of the immediate deaths after the disaster were due to involvement of lung. Within 5 days of the disaster, more than 3800 deaths were occurred and the rest became disabled4.
Various studies have documented the high incidence of respiratory morbidity among the surviving population (gas victims) due to single high level exposure of MIC56. Chronic inflammation of the respiratory tract is attributed for the long-term morbidity and respiratory function abnormality. Study conducted within a few months after the disaster had demonstrated the presence of bronchiolitis obliterans5. Subsequent study reported the presence of pulmonary fibrosis that was also confirmed histopathologically by the presence of interstitial pneumonia in autopsy sample36. One year after the disaster, Rastogi et al7 evaluated spirometry of gas victims and observed that the mixed pattern was the commonest lung function abnormality.
Ten years after the disaster, Cullinan et al8 assessed the respiratory morbidity in surviving population. After this study, no study was carried out to evaluate the extent and nature of long-term sequelae of MIC on respiratory system. Bhopal Memorial Hospital and Research Centre (BMHRC), a multi-specialty centre was set up in 2000 to provide tertiary care facility to the gas victims as well as to non MIC exposed population. Approximate 3,80,000 gas victims are registered with this hospital for free treatment and these patients are first evaluated at the primary care level in the eight mini units (satellite health centres) spread around the city and then referred to specialized departments of BMHRC, if required.
The purpose of the present study was to analyze the patterns of lung function abnormalities among gas victims (surviving mic0 exposed individuals) and to compare with the non-MIC exposed population (non gas exposed).
Material & Methods
The records of spirometry data of gas victims and non gas exposed subjects from the Pulmonary Medicine department of BMHRC that were done as part of evaluation of their respiratory complaints from August 2001 to December 2009, were analyzed retrospectively. The non gas exposed individuals included both the MIC unexposed population of Bhopal and also the surrounding areas. Only the acceptable and reproducible spirometric data were included in the analysis. If spirometry was performed more than once on a subject during this period, initially performed spirometric recording was included in data analysis. This study was approved by the local ethics committee.
Study population: Age, gender, height, weight, smoking status and spirometry results were noted from the records. The indications for spirometry were as part of evaluation of their respiratory symptoms.
Pulmonary function test: Jaeger Masterscope PC (Jaeger Co, Germany) was used for the spirometry and it was calibrated daily before use. Three acceptable and at least two reproducible maximal expiratory flow volume curves were obtained from each subject and the highest forced vital capacity (FVC) and forced expiratory volume in one second (FEV1) were recorded as per American Thoracic Society guideline9. Each patient was given two puffs of salbutamol (200 μg) and second spirometry was performed 15 min after the administration of salbutamol. The bronchodilator reversibility was defined as change of FEV1 and/or FVC 12 per cent and 200 ml compared with the baseline value.
Predicted values for FVC, FEV1 and FEV1/FVC were generated separately for men and women based on age and height using the north Indian reference equation10. Lower limits of normal (LLN) for FVC, FEV1 and FEV1/FVC were calculated as the difference between the predicted value and 1.645 times the standard error of estimate of the regression equation. Any observed value lower than its corresponding LLN was considered abnormal. If the FEV1/ FVC ratio and FVC values were more than LLN, these were categorized as normal pulmonary function.
If the FEV1/FVC was less than the LLN, it was categorized as an obstructive pattern and the severity of obstruction was classified as per American Thoracic Society (ATS/ERS) guideline11 i.e. mild obstruction if predicted > 70, moderate if 60-69, moderately severe if 50-59, severe if 35-49 and very severe if FEV1% predicted < 35.
If the FEV1/FVC value was above the LLN with FVC less than LLN, then it was categorized as restrictive pattern. American Thoracic Society guideline recommended that if the total lung capacities were not measured in restrictive pattern, the severity of restriction can be classified on the basis of largest value of FVC (pre- or post-bronchodilator FVC)9. Classification of severity of restriction was as follows: mild if % FVC is < LLN but > 70 per cent; moderate if %FVC < 70 and > 60; moderately severe if %FVC < 60 and > 50; severe if %FVC < 50 and > 34, and very severe if %FVC < 34.
Reversibility tests were not performed in 53 obstructive patterns and these cases were excluded while analyzing the reversibility of obstruction.
Statistical analysis: The SPSS for Windows version 9.0 software package (SPSS Inc, Chicago IL, USA) was used for statistical analysis. The study population was categorized in six age groups. For each age group, adjusted relative risks of developing restrictive and obstructive pattern in spirometry were computed by logistic regression analysis and P < 0.05 was considered significant.
Results
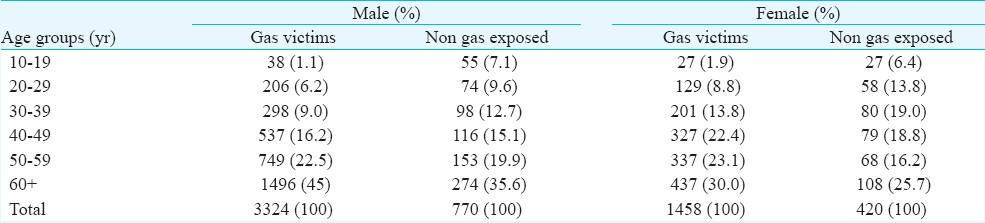
A total of 7412 spirometry procedures were performed in our pulmonary function laboratory between August 2001 and December 2009. After excluding the unacceptable and repeat tests, 5972 spirometry were included in the analysis. Of the 4782 gas victims who performed spirometry during this period, 3324 (69.5%) were males (Table I).
Obstructive pattern was the commonest abnormality observed in 2430 (50.8%) cases, restrictive pattern in 638 (13.3%) cases and normal spirometry was observed in 1714 (35.8%) cases. Irreversible and reversible obstruction was seen in 24 and 26.8 per cent, cases, respectively.
A total of 1190 non gas exposed individuals and 770 were male (64.7%) performed spirometry during the same period. Obstructive pattern was the commonest abnormal pattern among this group also and was observed in 515 (43.3%) cases, restrictive pattern in 163 (13.7%) cases and normal spirometry was observed in 512 (43%) cases.
Forty three per cent gas victims (59.4% male and 6.4% female) were either active or ex-smoker and obstructive pattern was observed in (48.6%) of them. The age wise distribution of smoking status among study population showed that the gas victims especially those 50 yr or more of age were more active smoker (P < 0.001) than the non gas exposed individuals of same age (Table II).
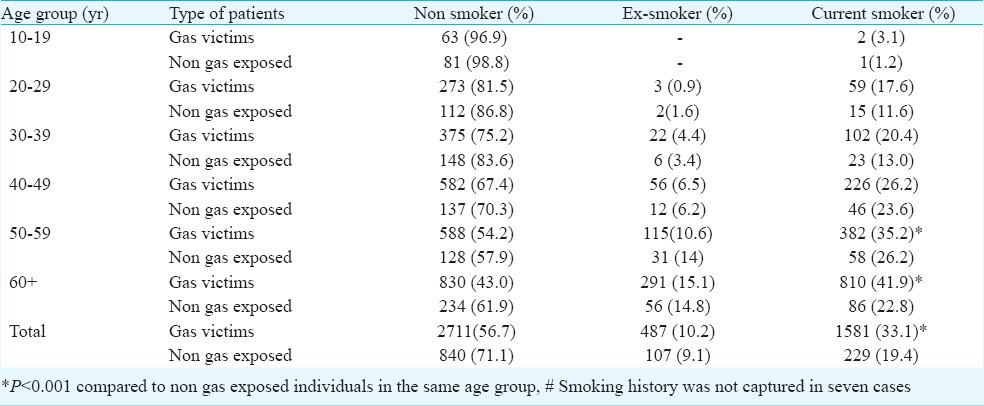
The age wise distributions of different spirometric abnormalities of study population were compared (Table III).The relative risk with 95 per cent confidence interval (CI) of developing different spirometric abnormalities among gas victims were assessed by logistic regression analysis. No overall increase in relative risk for developing restrictive abnormality among gas victims was observed except for 20-29 yr age group (adjusted relative risk: 2.94, P<0.001). The overall adjusted relative risks of developing reversible and irreversible obstruction among gas victims were 1.45 (95% CI 1.23 to 1.71, P<0.001) and 1.33 (95% CI 1.12 to1.58, P<0.001) respectively.
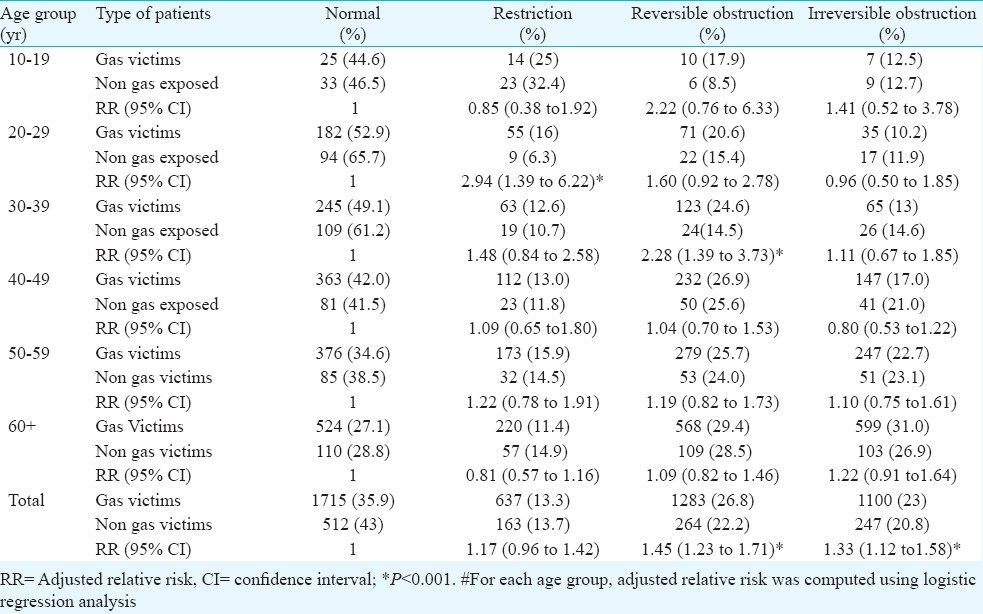
The distribution of severity of restriction among gas victims were as follows: mild 29.3 per cent, moderate 30.7 per cent, moderately severe 22.1 per cent, severe 13.8 per cent and very severe 4.1 per cent. The severity of obstruction among the gas victims were: mild 19.5 per cent, moderate 13.1 per cent, moderately severe 15.6 per cent, severe 26.7 per cent and very severe 25.1 per cent.
Among the gas victims, presence of mild restriction and severe obstruction (reversible or irreversible) were more among males than in females (Figs 1 & 2). The obstructive pattern remained the predominant spirometric abnormalities among the newly registered gas victims during the entire study period.
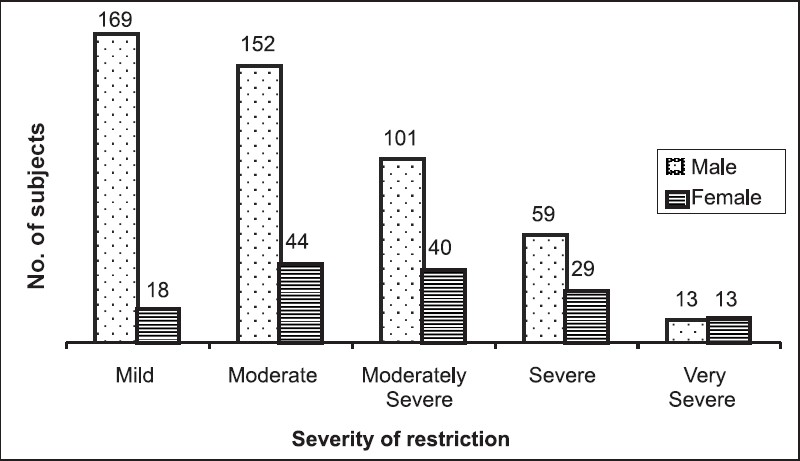
- Sex wise distribution of severity of restriction.
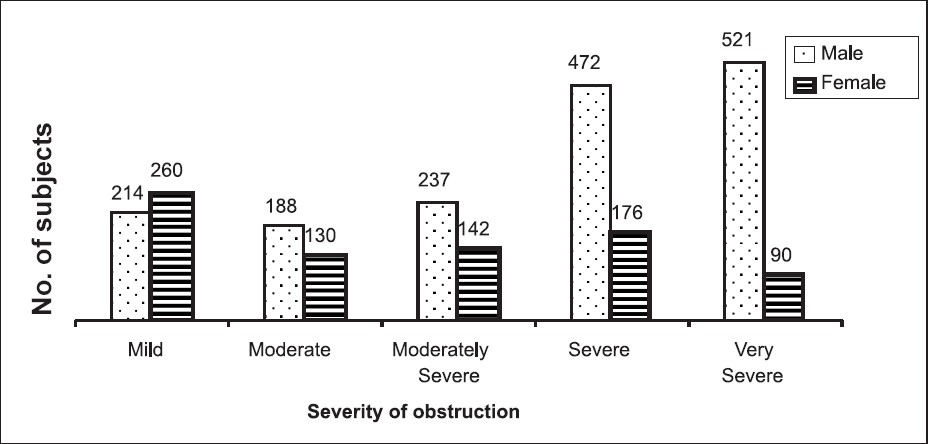
- Sex wise distribution of severity of obstruction.
Discussion
Immediately after the disaster and during the subsequent years epidemiological studies were carried out to evaluate the respiratory symptoms and spirometric abnormalities among the surviving gas victims. Kamat et al12 carried out spirometry on 113 persistently symptomatic gas-victims between 7 to 90 days after the disaster and found no significant changes in FVC and FEV1 during the three months follow up. The same group13 evaluated spirometry of 82 subjects between 7 and 53 days after the disaster and observed restrictive pattern in 78 per cent cases. Four weeks after the disaster, Bhargava et al14 conducted spirometry on 224 gas victims and observed normal spirometry in 56.3 per cent, obstructive pattern in 10.7 per cent, restrictive and mixed pattern in 17 per cent and 16 per cent, respectively.
Fifteen weeks after the disaster, Naik et al15 carried out spirometry of 326 subjects who were residing within 0.5-2 km from the Union Carbide plant. Restrictive pattern was observed as the commonest abnormality (49.1%), followed by obstructive pattern (21.2%). During the same period, another group evaluated spirometry in pediatric population residing within 2 km and 8-10 km from the factory and observed obstructive pattern in 84.8 and 66.6 per cent of cases, respectively16. A study conducted on 1109 gas victims in 1985 found abnormal findings on chest X-ray in 4.3 per cent due to exposure to MIC17.
Acquilla et al18 conducted spirometry on 476 subjects and observed abnormalities of FVC, FEV1 and FEV1/FVC ratio in 15.5 per cent cases. Dhara et al19 in 1994 had evaluated the exposure-response relationship among 1618 gas victims and observed largest difference in FEF25-75 between high and low exposed groups.
Several studies were carried out by various investigators from 1985 to 19942021. Within three months after the disaster, spirometry of 129 symptomatic patients residing within 2 km from the Union Carbide plant was done. Using the cut-off points 75 per cent for FVC and FEV1/FVC, spirometry data showed 55.8 per cent had normal, 10.1 per cent had obstructive pattern, 12.4 per cent had restrictive pattern and 21.7 per cent had mixed pattern. In another study 119 very severely affected gas victims were evaluated and 22.2 per cent had restrictive, 11.8 per cent had obstructive and 25.2 per cent had mixed pattern (based on 75% as the cut-off point for FVC and FEV1). These patients were first followed after 6-12 months and then at 4-5 years after the initial visit and no further deterioration of lung function was detected. From mid October 1985 to April 1988, spirometry of 4938 gas victims showed normal spirometry in 36 per cent cases, restrictive pattern in 50 per cent cases, obstructive pattern in 7 per cent cases and mixed pattern in 7 per cent cases (cut-off point between normal and impaired lung function was 80% of predicted). No deterioration in spirometric abnormalities was observed among severely affected gas victims during five year follow up.
The last study that evaluated the respiratory morbidity of gas victims was conducted by Cullinan et al8 in 1995. They evaluated spirometry of 74 subjects and observed that FVC, FEV1, FEV1/FVC ratio and FEF25-75 were reduced due to exposure of MIC. They did not categorize the pattern of spirometric abnormality, but observed that obstructions were mostly irreversible8.
The studies that were carried out more than one year after the disaster documented the reduction in prevalence of restrictive pattern20. The prevalence of restrictive disorders across the studies were variable due to use of different cut off value of FVC. The distributions of severity of restrictive pattern in our study was similar to an earlier study15. The increased relative risk of restrictive abnormality among gas victims was limited in 20-29 yr age group only. So, the gas victims who were infants at the time of disaster were possibly more affected by the residual fibrotic changes in lung. Infant mortality rate among gas victims was high in initial two years. Subsequently, the mortality rate among > 50 yr of age was increased21. The gas victims who were exposed to massive to sub-massive MIC developed severe restrictive defects i.e. interstitial lung disease and probably died within a few years of the disaster. The gas victims with restrictive abnormalities in present study might have exposed to lesser amount of MIC and thus no overall increase in relative risk for development of restrictive pattern was observed. Earlier studies also failed to detect any further deterioration of lung function during follow up2021. The registrations of new restrictive abnormalities remained static throughout our nine year study period suggesting that restrictive defects were possibly non progressive.
The prevalence of obstruction in gas victims varied from 10.1 to 21.2 per cent141520. We observed obstructive pattern in 50.8 per cent gas victims and among whom 51.8 per cent were suffering from severe to very severe obstruction and 29.3 per cent had mild obstruction. So, the present study showed that with the passage of time, both the incidence and the severity of obstruction among gas victims had increased. The overall relative risks of developing reversible and irreversible airflow obstruction among gas victims were 1.45 and 1.33, respectively. These observations suggest that the gas victims irrespective of their age are at higher risk of developing obstructive lung disease. Without any pre-existing respiratory illness, single exposure to high levels of an irritating vapour, fume, or smoke may cause asthma like symptoms known as reactive airways dysfunction syndrome (RADS)22. The increased relative risk for reversible obstructive pattern in 30-39 yr age group are may either be due to development of RADS as a consequence of MIC inhalation or MIC might have reactivated the latent asthma or worsened the pre existing asthma23.
Smoking is an important risk factor for developing airflow obstruction; 9.9 per cent gas victims were found to be smoker during the survey conducted by ICMR in 198521. Earlier studies failed to observe any effect of smoking on pulmonary function71920. In the present study, 43.3 per cent gas victims were current or ex-smokers, and smoking was significantly more among those > 50 yr age. Our study also showed a significant relationship between smoking and presence and severity of obstruction (P<0.001).
Socio-economic status is a known risk factor for the development of airflow obstruction24. In 1985, the monthly income of 96 per cent gas victims was below  300/month, and only 1.25 per cent earned more than
300/month, and only 1.25 per cent earned more than  1000/month and 73 per cent had no occupation21. Gupta et al17 also reported that per capita income 89.5 per cent gas victims was
1000/month and 73 per cent had no occupation21. Gupta et al17 also reported that per capita income 89.5 per cent gas victims was  300/month or less. So the poor socio-economic status might also played a role in development of predominance of obstructive pattern among the surviving gas victims.
300/month or less. So the poor socio-economic status might also played a role in development of predominance of obstructive pattern among the surviving gas victims.
Rastogi et al7 observed more respiratory impairments in female population. Present study showed that the restrictive defects were more common in males than in females, but as the severity of restriction increased, the difference of prevalence between males and females were lost. In case of obstructive defects, severe obstructions were more among males than in females and this could be possibly due to additive effect of smoking.
The use of reference equations for Caucasian leads to misinterpretation of spirometric data in a significant proportion of Indian population25. There is no uniform predicted equation for the Indian population. In comparison to north Indian reference equation for spirometry, the south Indian and west Indian reference equation under predict the LLN of FEV1 and FVC and hence we had used north India reference equation in our study10. Lower limit of FEV1/FVC 70 per cent results in a significant false-positive result in male > 40 yr of age and female > 50 yr age and there is increased risk of over-diagnosis of obstruction in asymptomatic elderly never-smoker subjects2627. Use of different cut-off value and reference equations leads to variable interpretation of spirometry. Previous studies had used the value of FEV1 and FVC less than 75 or 80 per cent of predicted as abnormal. In the present study, the predicted equation for north Indian was used to define the normal and LLN of FVC, FEV1 and FEV1/FVC and thus reduced the risk of over diagnosis.
The limitation of this study was that the study population was hospital based and only those who had respiratory symptoms were evaluated. The collection of spirometric data was started 16 yr after the disaster and severely affected gas victims might have died by then or were incapable to visit this hospital due to severity of their disease status. During the long interval between the disaster and data collection, many affected individuals might have migrated out. The actual recall of the disaster after 16 yr was difficult and thus the exposure history might be unreliable. To avoid the recall bias, the exposure-effect relationship was not attempted. The presence of RADS among the patient with normal spirometry and chronic respiratory symptoms was not evaluated in present study. The hospital had no paediatrics department, so very few paediatric patients were enrolled in study. The socio-economic status of the study population was not collected. Even excluding smoking status and advanced lesion on chest X-ray, previous history of pulmonary tuberculosis is a risk factor for developing obstructive pattern in spirometry. Some of our study population had prior pulmonary tuberculosis, but the effect of tuberculosis on lung function was not explored.
The diagnosis of restrictive defects in present study was based on the results of spirometry. In spirometry, reduced vital capacity with a normal or even slightly increased FEV1/FVC may be observed due to sub maximal effort or patchy airflow obstruction. The predictive value of spirometric diagnosis of restriction i.e. FVC < LLN and FEV1/FVC ≥ LLN varies from 26.3 to 73.9 per cent28. Thus, the confirmation of restrictive defect requires the measurement of total lung capacity (TLC) and that was not measured in all cases of our restrictive pattern. So, all mild restrictive patterns observed in the present study might not have the actual restriction.
A mixed pattern in spirometry is co-existence of both obstructive and restrictive defects and is characterized by reduction of both FEV1/FVC and TLC below the 5th percentiles of predicted values. FVC can be reduced in both obstructive and restrictive defects. So the presence of a restrictive component in obstructive pattern required measurement of TLC by body plethysmography. Since TLC was not evaluated in the present study, the presence of mixed pattern cannot be ruled out.
In conclusion, this study showed that the obstructive pattern was the commonest spirometric abnormality among the surviving gas victims with respiratory symptoms and the prevalence of it (either reversible or irreversible) was more in gas victims compared to non-exposed subjects. Tobacco smoking and poor socio-economic condition might have played a significant role in development of predominant obstructive pattern.
Acknowledgment
The author thanks to Prof N K Tyagi, Mahatma Gandhi Institute of Medical Sciences (MGIMS), Sevagram for statistical analysis and all staffs of Pulmonary Medicine Department of Bhopal Memorial Hospital & Research Centre for their help in collecting data.
References
- Bhopal gas disaster: Unidentified compounds in the residue of the MIC Tank-610. J Indian Acad For Sci. 1991;30:13-8.
- [Google Scholar]
- The Union Carbide Disaster in Bhopal: A review of health effects. Arch Environ Health. 2002;57:391-404.
- [Google Scholar]
- Disaster at Bhopal: the accident, early findings and respiratory health outlook in those injured. Bull Eur Physiopathol Respir. 1987;23:587-90.
- [Google Scholar]
- Chronic lung inflammation in victims of the toxic gas leak at Bhopal. Resp Med. 1995;89:105-11.
- [Google Scholar]
- Effect of exposure to toxic gas on the population of Bhopal. II. Respiratory impairment. Indian J Exp Biol. 1988;26:161-4.
- [Google Scholar]
- Bhopal respiratory morbidity 10 years after the Union Carbide gas leak at Bhopal: a cross sectional survey.The International Medical Communication on Bhopal. BMJ. 1997;314:338-42.
- [Google Scholar]
- American Thoracic Society. Lung function testing: selection of reference values and interpretative strategies. Am Rev Respir Dis. 1991;144:1202-18.
- [Google Scholar]
- Pulmonary function laboratory in the tropics: needs, problems and solutions. In: Sharma OP, ed. Lung Disease in the Tropics. New York: Marcel Dekker; 1991. p. :523-42.
- [Google Scholar]
- Sequential respiratory changes in those exposed to the gas leak at Bhopal. Indian J Med Res. 1987;86:20-38.
- [Google Scholar]
- Early observations on pulmonary changes and clinical morbidity due to the isocyanate gas leak at Bhopal. J Postgrad Med. 1985;31:63-72.
- [Google Scholar]
- Early observations on lung function studies in symptomatic “gas”-exposed populations of Bhopal. Indian J Med Res. 1987;86:1-10.
- [Google Scholar]
- Medical survey of methyl isocyanate gas affected population of Bhopal. Part II. Pulmonary effects in Bhopal victims as seen 15 weeks after M.I.C. exposure. J Postgrad Med. 1986;32:185-91.
- [Google Scholar]
- A survey of Bhopal children affected by methyl isocyanate gas. J Postgrad Med. 1986;32:192-95.
- [Google Scholar]
- Effect of exposure to toxic gas on the population of Bhopal.Epidemiological, clinical, radiological and behavioral studies. Indian J Exp Biol. 1988;26:149-60.
- [Google Scholar]
- Long-term morbidity in survivors of the 1984 Bhopal gas leak. Natl Med J India. 1996;9:5-10.
- [Google Scholar]
- Personal exposure and long-term health effects in survivors of the Union Carbide disaster at Bhopal. Environ Health Perspect. 2002;110:487-500.
- [Google Scholar]
- Technical Report on Population Based Long Term Clinical Studies (1985-1994): Indian Council of Medical Research, New Delhi. Available from: http://www.icmr.nic.in/final/tech_rep_clinical.pdf
- [Google Scholar]
- Indian Council of Medical Research. Health effects of the toxic gas leak from the union carbide methyl isocyanate plant in Bhopal. Technical report on population based long term epidemiological studies (1985-1994) Available from: http://www.icmr.nic.in/final/bgdrc-technical%20report.pdf
- [Google Scholar]
- Reactive Airways Dysfunction Syndrome (RADS).persistent asthma syndrome after high level irritant exposures. Chest. 1985;88:376-84.
- [Google Scholar]
- Late consequences of accidental exposure to inhaled irritants: RADS and the Bhopal disaster. Eur Respir J. 1996;9:1973-6.
- [Google Scholar]
- Socioeconomic status and chronic obstructive pulmonary disease. Thorax. 1999;54:737-41.
- [Google Scholar]
- Applicability of commonly used Caucasian prediction equations for spirometry interpretation in India. Indian J Med Res. 2005;122:153-64.
- [Google Scholar]
- Spirometric reference values from a sample of the general US population. Am J Respir Crit Care Med. 1999;159:179-87.
- [Google Scholar]
- Risk of over-diagnosis of COPD in asymptomatic elderly never-smokers. Eur Respir J. 2002;20:1117-22.
- [Google Scholar]
- The utility of spirometry in diagnosing pulmonary restriction. Lung. 2008;186:19-25.
- [Google Scholar]






