Translate this page into:
Rare case of congenital generalized lipodystrophy type 1
*For correspondence: kavsendo@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
A 17 yr old female child† was presented to the department of Endocrinology, Andhra Medical College, Visakhapatnam, India, in October 2019, with pathological bilateral radial neck fracture. She was born of third-degree consanguineous marriage second in birth order, with normal secondary sexual characters, secondary amenorrhoea for five years, diagnosed diabetes mellitus three years ago, and was on basal bolus insulin regimen at 2 U/kg body weight for the last two years. Elder sister also has diabetes and secondary amenorrhoea.
On examination, body mass index was 26.55 kg/m2; acanthosis nigricans, generalized absence of subcutaneous tissue, acromegaloid features (Figs 1 and 2), muscular appearance, phlebomegaly and clitoromegaly were present. Further evaluation showed hypertriglyceridaemia and multiple cysts in the tubular bones (Figs 3 and 4). The features were suggestive of congenital generalized lipodystrophy type I. The patient was managed with basal bolus insulin, statins, fibrates and conservative management for fracture. Congenital generalized lipodystrophy should be suspected in patients with loss of subcutaneous tissue, insulin resistance and acromegaloid features.

- Loss of subcutaneous tissue over abdomen.

- Acromegaly of feet.
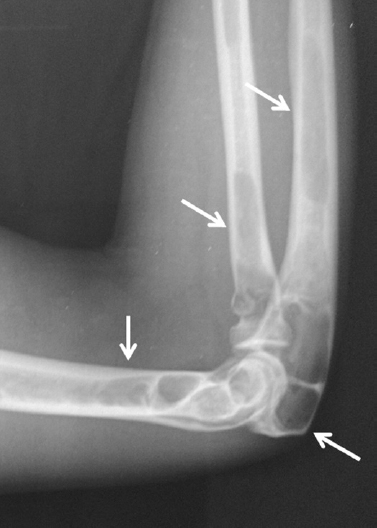
- X-ray of the right elbow showing multiple bone cysts in radius, ulna and humerus (arrows).

- X-ray of the right ankle showing bone cysts in the tibia (arrow).
Conflicts of Interest: None.





