Translate this page into:
Radiological evaluation of metastatic lymph nodes in carcinoma cervix with emphasis on their infiltrative pattern
For correspondence: Dr Ekta Dhamija, Room Number 137, First Floor, Department of Radiodiagnosis, Dr B.R. Ambedkar Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, New Delhi 110 029, India e-mail: drektadhamija.aiims@gmail.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Imaging has been added to the International Federation of Gynecology and Obstetrics (FIGO) 2018 staging system of cervical carcinoma. This study was performed to assess the impact of imaging in staging and to ascertain the prevalence and pattern of nodal metastasis on contrast-enhanced computed tomography (CECT) in patients with cervical carcinoma who were treated based on FIGO 2009 staging system.
Methods:
This retrospective study was conducted to evaluate all patients with biopsy-proven cervical carcinoma who underwent CECT of abdomen at a tertiary cancer centre in north India from April 2017 to April 2019 and for whom either baseline or follow up scans were available. In patients with enlarged or necrotic lymph nodes, the location, size and pattern of infiltration of adjacent organs were recorded.
Results:
A total of 602 patients of cervical carcinoma had undergone CT during the study period, of whom 138 (22.9%) underwent CT at baseline and 464 (77.1%) patients during follow up. The FIGO (2009) stage distribution at the time of presentation was stage IB: 109 (18.1%); stage IIA: 14 (2.3%), stage IIB: 118 (19.6%), stage IIIA: 12 (2%), stage IIIB: 277 (46%), stage IVA: 20 (3.3%) and stage IVB: 52 (8.6%). Ninety of the 138 (65.22%) patients underwent a stage shift according to the FIGO 2018 because of the presence of enlarged lymph nodes at baseline scan. Sixteen (2.7%) patients had infiltrative nodal masses most commonly involving the blood vessels (n=14) followed by ureter (n=8), bones (n=5), muscle and bowel (n=3, each). The majority (14/16) of these patients presented with vague abdominal pain, discomfort and vomiting, while two had bone pain.
Interpretation & conclusions:
CECT at baseline helps in accurately assessing the stage in cervical carcinoma. It helps in the identification of lymph node metastasis in cervical carcinoma, which is crucial for guiding accurate management.
Keywords
Carcinoma cervix
FIGO staging
infiltrative lymph node
metastatic lymph nodes
pelvic lymphadenopathy
Cervical carcinoma is the second most common cause of cancer in Indian women, with significant associated morbidity and mortality1. Multiparity, immunodeficiency, smoking, use of oral contraceptive pills, sexual intercourse at an early age and low socio-economic status are among the risk factors for cervical carcinoma2, and abnormal bleeding per vaginum is the most common presentation. Treatment is based on the International Federation of Gynecology and Obstetrics (FIGO) staging for cervical carcinoma, which has traditionally been based on clinical examination with limited role for imaging. However, the recent modifications incorporated in the FIGO 2018 revision allow findings on imaging and pathology to change the stage3. One of the major amendments is inclusion of lymph node involvement, which is known to greatly affect the prognosis and survival, in the staging system. The five-year survival rate which is upto 90 per cent for patients who receive post operative irradiation for lymph node metastases; drops to less than 50 per cent in those who do not receive radiation therapy4. Malignant cells within the lymph nodes tend to proliferate and infiltrate into the adjacent viscera, making their surgical resection impossible. Hence, the presence of enlarged lymph nodes on imaging places the patient in stage IIICr according to the latest FIGO staging system, irrespective of the size of the primary tumour3. Any lymph node with short-axis dimension more than 10 mm or with necrosis within may be considered as involved on cross-sectional imaging by computed tomography (CT) or magnetic resonance imaging (MRI) 5.
The 2018 FIGO staging system recommends the use of available imaging modality for assessments and has not mandated a particular modality. However, the role and efficacy of each modality have been emphasized, for example, MRI is the preferred modality for local staging of the disease due to its superior contrast resolution and CT is acceptable in the advanced stages3. Unavailability of baseline imaging may lead to underdiagnosis of nodal metastases, and these patients may present later with an advanced disease and varied non-specific clinical manifestations. Haematogenous or contiguous infiltration of bones in cervical carcinoma patients has been documented by a few investigators678.
This study was performed to assess the impact of imaging in staging and to ascertain the prevalence and pattern of nodal metastasis on CT in patients with cervical carcinoma who were treated based on the FIGO 2009 staging system.
Material & Methods
This retrospective observational study was conducted in the department of Radiodiagnosis of a dedicated cancer centre (Dr. B.R. Ambedkar Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, New Delhi, India) after obtaining approval from the institute ethics committee with a waiver of informed consent. All patients who underwent CT in the department between April 2017 and April 2019, either at baseline or during follow up, were identified from the radiology reporting data system and included in the study. Imaging done outside this centre was not included for analysis. The clinical staging (FIGO 2009) and treatment plan were obtained from the patients’ record files.
Image acquisition: All CT scans were performed after administration of intravenous iodinated contrast agent on Definition AS+ 64 slice scanner (Siemens Healthcare, Erlangen, Germany), and the images were acquired in the venous phase. Delayed scans were obtained whenever necessary. All CT scans were reported by the radiologists with 5-10 yr of experience in oncoradiology. Discordance, if any, was resolved by consensus agreement between the two radiologists.
Image interpretation and data acquisition: Demographic details were recorded and patients with reported nodal involvement were assessed and classified based on whether they had undergone a baseline or a follow up scan. In patients with enlarged or necrotic lymph nodes-location, site and size of the lymph nodes in short-axis dimension were recorded. Nodes with infiltration were assessed for the structures infiltrated, morphology (discrete or conglomerate), enhancement pattern, presence or absence of necrosis and presence or absence of calcification.
Infiltration of vessels was defined as encasement of vascular surface for >90° of the circumference, surface irregularity or luminal narrowing. Ureteric infiltration was defined as circumferential encasement with or without upstream dilatation; bowel infiltration as wall thickening or irregularity with or without upstream obstruction; bone infiltration as cortical irregularity to frank destruction; muscle infiltration as loss of interface or obvious infiltration of muscles or abnormal enhancement within. The study flowchart is summarized in Fig. 1.

- Study flowchart.
Statistical analysis: All observations were tabulated and frequencies were calculated. Statistical analysis was performed using Stata Data Analysis Software version 14.2 (StataCorp. Texas, USA). Association between size of the cervical mass and the presence of enlarged lymph nodes in baseline imaging was assessed using Wilcoxon rank-sum test, as the size of cervical mass was not normally distributed. All statistical tests were two-sided and statistical significance was taken as P<0.05.
Results
A total of 602 patients with cervical carcinoma underwent CT of abdomen (with or without chest) during the study period, of whom CT scans were done for 138 (22.9%) at the time of initial staging and for 464 (77.1%) patients scans were taken during follow up. The mean age of the patients was 52 ± 10.8 yr (range 24-92 yr).
Staging and treatment received: Of the 602 patients, 109 (18.1%) were classified as stage IB cervical cancer, 14 (2.3%) in stage IIA, 118 (19.6%) in stage IIB, 12 (2%) in stage IIIA, 277 (46%) in stage IIIB, 20 (3.3%) in stage IVA and 52 (8.6%) in stage IVB at the time of presentation. Patients in stage IB had received treatment in the form of surgery with chemoradiation (44/109, 40.4%) or surgery with radiotherapy (28/109, 25.7%); only chemoradiation (20/109, 18.3%); or only radiotherapy (17/109, 15.6%). Patients in stage IIA underwent surgery and radiotherapy (1/14, 7.1%) or chemoradiation (5/14, 35.7%) or concurrent chemoradiation (8/14, 57.1%). Most of the patients in stage IIB received definitive chemoradiotherapy (91/118, 77.1%), while others underwent adjuvant chemoradiation (16/118, 13.6%), adjuvant radiotherapy (6/118, 5.1%) or radiotherapy alone (5/118, 4.2%). Patients with stage IIIA disease received chemoradiation (10/12, 83.3%) or radiotherapy alone (2/12, 16.7%) and those with stage IIIB disease received chemoradiation (235/277, 84.8%), radiotherapy alone (34/277, 12.3%), or adjuvant chemoradiation (8/277, 2.9%). Among those with stage IVA and IVB, 12/20 (60%) and 35/52 (67.3%) received chemoradiation, respectively, while 8/20 (40%) and 17/52 (32.7%) received radiotherapy alone.
Imaging evaluation: Radiological involvement of the lymph nodes could be appreciated in 226 of 602 patients (37.5%): 90 of 138 (65.2%) at baseline and 136 of 464 (29.3%) at the time of follow up. The average largest diameter of the cervical mass on baseline imaging in patients with lymphadenopathy was 6.05 cm, with a range of 2-8 cm. There was no significant association between the size of the cervical mass and the presence of enlarged lymph nodes in baseline imaging (P=0.17).
Of the 226 patients with lymph node involvement, isolated pelvic lymphadenopathy was present in 103 patients (45.6%) (Fig. 2). Isolated retroperitoneal nodes were seen in 57 patients (25.2%), while pelvic as well as retroperitoneal lymph nodes were found in 49 patients (21.7%). In addition to these sites, abnormal nodes were also noted in inguinal (29, 12.8%), mediastinal (10, 4.4%) and supraclavicular locations (7, 3.1%) (Figs 3 and 4).
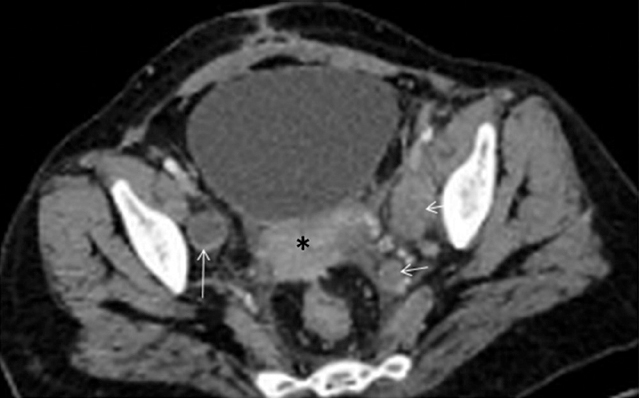
- Recurrence of carcinoma cervix at the local site and iliac lymph nodes in a 37 yr old woman: axial contrast-enhanced computed tomography (CECT) section at the level of pelvis shows recurrent soft tissue mass in the region of cervix (asterisk) along with enlarged external as well as internal iliac lymph nodes (arrows).

- Mediastinal lymph node involvement in follow up computed tomography (CT)scan of a 59 yr old woman who was treated for carcinoma cervix: axial CECT image shows conglomerate lymph nodal mass in the pre-vascular location (black asterisk) encasing internal mammary vessels (bright dot within), infiltrating the chest wall with extra-thoracic extension in parasternal location. Also note right lung metastasis (white asterisk).
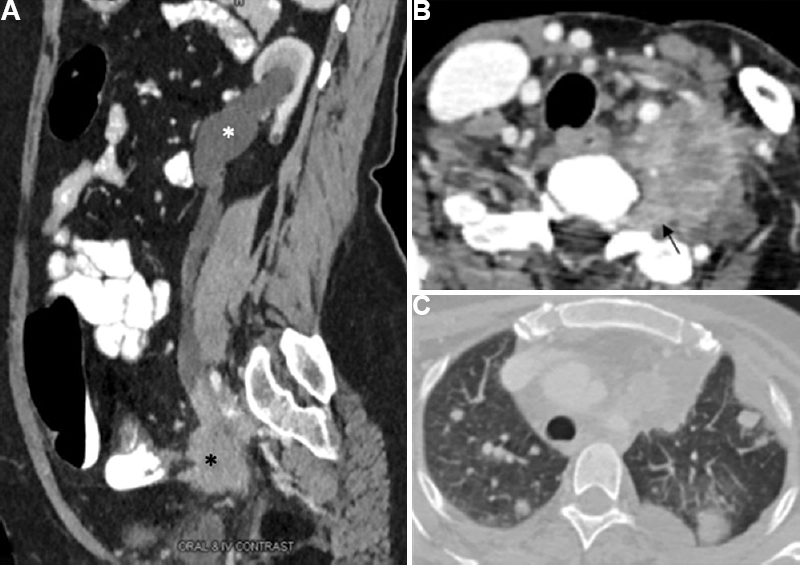
- Infiltrative nature of the metastatic lymph nodes in a 50 yr old women with proven carcinoma cervix: (A) sagittal reformatted image showing presence of a spiculated irregular nodal mass in left iliac location (asterisk) infiltrating and occluding the lower ureter with upstream hydroureteronephrosis. (B) Enlarged heterogeneously enhancing soft tissue mass in left supraclavicular and paraspinal location encasing the vertebral artery and having intraspinal extension along the neural foramina (arrow) mimicking nerve sheath tumour on imaging, if seen in isolation. (C) Same patient also had multiple lung metastases.
Baseline evaluation with imaging (CT) was available for 138 patients. Of the 90/138 (65.22%) patients with enlarged lymph nodes, 72 underwent a stage shift, who were clinically classified as stage IB (n=12, 16.6%), stage IIA (n=2, 2.7%), stage IIIA (n=3, 4.2%) and stage IIIB (n=45, 62.5%) according to the FIGO 2009; and would now be categorized as stage IIIC1r (19/72) and IIIC2r (43/72) according to the FIGO 2018 because of the presence of enlarged lymph nodes at baseline scan, while two (2.7%) and eight (11.1%) patients were assigned to stages IVA and IVB, respectively, following the imaging evaluation. Remaining 18/90 patients were already belonging to stage IV.
Of the 464 patients who underwent follow up imaging after treatment, 136 (29.3%) had enlarged nodes and were considered as nodal involvement or metastases. Among those who had nodal involvement, 30 patients (22%) had recurrent cervical mass as well (Fig. 2). However, 106 patients (78%) had only nodal involvement without any local site mass. Further, 33 patients (24.2%) had isolated retroperitoneal nodal involvement. Table I summarizes the lymph node involvement in carcinoma cervix patients.
| Parameters | n (%) |
|---|---|
| Total number of cases | 602 |
| Baseline imaging | 138 (22.9) |
| Follow up imaging | 464 (77.1) |
| Number of cases with lymph node involvement | 226 (37.5) |
| On baseline imaging | 90/138 (65.2) |
| On follow up imaging | 136/464 (29.3) |
| Average largest diameter of cervical mass on baseline imaging | |
| With lymphadenopathy (mean±SD) (cm) | 6.05±0.66 |
| Without lymphadenopathy (mean±SD) (cm) | 5.89±0.34 |
| Number of patients with lymphadenopathy | 226 |
| Pelvic nodes only | 103 (45.6) |
| Para-aortic nodes only | 57 (25.2) |
| Pelvic and para-aortic nodes | 49 (21.7) |
| Inguinal nodes | 29 (12.8) |
| Nodes at distant sites | 17 (7.5) |
| Number of patients with recurrence/residual disease | 136 |
| Disease at local site with nodal involvement | 30 (22) |
| Nodal involvement only | 106 (78) |
| Number of patients with infiltrative nodes | 16 (2.7) |
Sixteen (16/602, 2.7%) patients had infiltrative nodal masses at the time of imaging, which were categorized as stages IB (4/16, 25%), IIA and IIB (2/16, 12.5% each), IIIB (6/16, 37.5%) and IVB (2/16, 25%) according to the FIGO 2009 staging system. According to the FIGO 2018 staging, these would be redesignated as stage IIIC1r (n=5/14, 35.7%) and IIIC2r (n=9/14, 64.3%). These lymph nodes were conglomerate with mean size of 4.5 cm (range 2.5-9 cm) at the time of scan acquisition. The shape was irregular and margins were ill-defined (11/16) and lobulated (5/16), with variable amounts of necrosis within. No lymph node was discrete and none showed calcification within (Table II).
| n (%) | |
|---|---|
| Number of patients with infiltrative nodes | 16/602 (2.7) |
| Mean size±SD (cm) (range) | 4.5±2.1 SD (2-5.9) |
| Site/structure involved (n=16) | |
| Vascular | 14 (87.5) |
| Osseous | 5 (31.3) |
| Bowel | 3 (18.8) |
| Ureter | 8 (50) |
| Muscle | 3 (18.8) |
| Other sites (pleura/kidney/spleen/pancreas/ovary) | 5 (31.3) |
| Shape | |
| Well defined | 0 |
| Irregular | 16 (100) |
| Margins | |
| Circumscribed/well defined | 0 |
| Ill defined | 11 (68.8) |
| Lobulated | 5 (31.3) |
| Enhancement | |
| Heterogeneous | 16 (100) |
| Homogeneous | 0 |
| Necrosis | 16 (100) |
| Calcification | 0 |
Infiltration of vessels was the most common pattern of infiltration and was seen in 14 of 16 patients. Para-aortic lymph nodes were the most common group of nodes that showed vascular infiltration (Fig. 5). Inferior vena cava and aorta were involved in majority of the cases (8/14), based on the pre-defined criteria. Other vessels found to be involved were the common iliac, external and internal iliac and renal vessels. One patient showed involvement of superior and inferior mesenteric arteries. Five patients showed infiltrative bone metastasis to the iliac bone and vertebrae (Fig. 5). Lymph nodes infiltrating the ureter were seen in eight patients (Figs 4 and 5), of whom the majority (n=6) showed involvement of the left ureter. Pelvic nodes more commonly showed infiltration into the ureter (n=5) than retroperitoneal nodes (n=3). Muscle involvement was seen in three of the 16 patients. Bowel involvement was also seen in three patients: colon (n=2) and duodenum (n=1). Other structures that were involved by lymph nodes were pleura, kidney, spleen, pancreas and ovary, each in one patient. Infiltration into a single structure was seen in six patients (vessels, n=4; ureter, n=1; pleura, n=1), while infiltration into multiple structures was seen in the remaining patient.
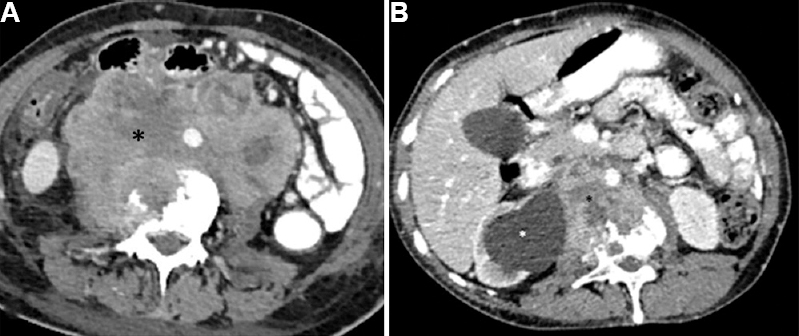
- Infiltrative retroperitoneal nodes in follow up CT scan of a 42 yr old women with history of carcinoma cervix. (A) Axial CECT image in soft tissue window shows large conglomerate nodal mass in retroperitoneum with necrosis within (black asterisk). The mass is infiltrating aorta, inferior vena cava, psoas muscle and is causing erosion of the adjacent vertebral body. Anteriorly, it is infiltrating the colon also. (B) Metastatic retroperitoneal lymph nodes in a 54 yr old woman with carcinoma cervix, post treatment: Follow up CECT scan shows metastatic retroperitoneal lymph nodes (black asterisk) infiltrating aorta, vertebral body, right psoas muscle and the ureter causing upstream hydronephrosis (white asterisk). Inferior vena cava cannot be appreciated suggesting infiltration and occlusion with appearance of dilated tortuous collateral channels in the subcutaneous plane of abdominal wall.
Pelvic and retroperitoneal nodes showed similar incidence of infiltration into the vessels (n=6 vs. n=7) and bones (n=3 vs. n=2). Among the 16 patients who showed infiltrative nodal masses, the majority (14, 87.5%) presented with vague abdominal pain or discomfort and vomiting. None of these patients had local disease clinically or on imaging at the time of presentation. Two patients (12.5%) had bone pain at the time of follow up imaging, and both had infiltrative bone metastasis. There was one patient with conglomerated lymph nodal mass showing extension into the neural foramina.
Distant metastases were seen in 93 of 602 (15.4%) patients: to lungs, bone, liver, adrenal, brain and omentum (Figs 3 and 4).
Discussion
Cervical carcinoma is the fourth most common cancer in women worldwide with an estimated 604,127 new cases annually9. It is the second most common cancer in Indian women after breast cancer with an estimated 75,209 new cases annually10. Although the incidence has shown a reducing trend over the past few years, yet the patients continue to present in the advanced stages and it is associated with significant morbidity. The present study highlights the role of imaging for staging and evaluation of patients with cervical carcinoma at the baseline and the peculiar infiltrative nature of its metastatic lymph nodes.
Cervical carcinoma is a locally invasive disease in its early stages, which makes it amenable to clinical assessment. Since nearly 85 per cent of cases occur in low- and middle-income countries where resources are limited, FIGO continued to recommend only clinical staging with a few basic investigations allowed to change the stage11. Being a tertiary care centre, most of the patients were referred to us after work up and surgery performed at a peripheral centre. Therefore, the baseline imaging of most of the patients could not be assessed in this study.
Cervical carcinoma can be treated by surgery or chemoradiation. It is desirable to select the most appropriate treatment modality. Advancements in diagnostic modalities, surgical techniques and radiation therapy have led to a revolution in the field of oncology. Cross-sectional imaging such as MRI depicts parametrial infiltration and local extent of the tumour with greater sensitivity and specificity as compared to clinical examination12. However, due to logistic reasons and resource constraints, CT is the most common imaging modality used for staging of this cancer. The revised FIGO 20183 highlighted the role of imaging and incorporated it into the staging system with major modifications in the stages II and III. Since the mode of spread of cervical cancer is local infiltration and lymphatic spread, it is only logical that it extends into the parametrium and infiltrates pelvic lymph nodes most commonly13. The five-year survival drops to 56 per cent in patients with pelvic and 17 per cent with distant nodal involvement, in contrast to 92 per cent when the disease is confined to cervix alone14.
Primary route of cervical cancer spread is by direct extension into the parametrium, vagina, uterus and adjacent organs, i.e. bladder and rectum. This pattern follows a path of least resistance for spread. Haematogenous spread occurs commonly via Batson’s venous plexus, and systemic haematogenous metastasis to distant organs is unusual15. Involvement of spaces surrounding the basement membrane can lead to lymphatic embolization of tumour and spread to adjacent lymph nodes. This lymphatic spread occurs usually in an orderly fashion in which it courses through the parametria and drains into the external iliac, hypogastric, obturator and common iliac nodes. Further spread can reach up to scalene nodes through the involvement of retroperitoneal nodes, cistern chyli and thoracic duct. However, at times, direct spread to para-aortic nodes can also be seen. Enlarged supraclavicular lymph nodes have also been reported in cases of cervical carcinoma16.
Considering the importance of lymph node metastasis in prognosis and survival, the FIGO has incorporated it into the 2018 modified staging system3. Any size of tumour mass with lymphadenopathy is upgraded to stage IIIC in the latest staging. Presence of enlarged lymph nodes on CT, MRI or positron emission tomography (PET) has implications in management protocol in the form of addition of radiotherapy to the respective sites17. The incidence of pelvic and para-aortic lymph node metastases in carcinoma cervix reported in previous studies ranges from 3.7 to 21.7 per cent for the former and five to 25 per cent for the latter, through various stages of cervical cancer18. In comparison, a higher incidence of nodal metastases was observed in our study with 29 per cent of patients presenting with recurrence in the form of retroperitoneal and pelvic lymphadenopathy. This may be due to the fact that ours is a tertiary care centre, and hence, we receive more referrals for advanced diseases. The prognosis of a relapsed case is usually poor as it is often associated with a systemic spread of disease. Our study also revealed involvement of inguinal (4.8%), mediastinal (1.7%) and supraclavicular (1.2%) lymph nodes. No significant association was found between the mass size and lymph nodal involvement or recurrence in our study. This is in contrast to previous reports19 and may be attributed to the large percentage of follow up and treated cases in our study.
Of the 138 patients who underwent baseline evaluation with CT in our study, 90 (65.22%) patients underwent a stage shift. Similar to our results, a study included 22 articles which assessed the safety and impact of pre-treatment para-aortic lymph node surgical staging; found that 18 per cent of patients with stage IB-IVA cervical cancer had para-aortic lymph node metastases20. In another study, up to 35 per cent of clinically assessed stage IIB and 20 per cent of stage III tumours were reported to have positive para-aortic nodes21. In the revised staging, all these cases would undergo stage shift and will be assigned to stage IIIC. This also suggests that CT may be considered as an acceptable modality for stating of carcinoma cervix patients, in resource-constraint settings.
There have been reports on continuous infiltration of enlarged metastatic lymph nodes into adjacent bones in cervical carcinoma. Many authors have described direct lumbar spine infiltration from metastatic para-aortic lymph nodes2223. In our study, 2.7 per cent cases were observed with infiltrative metastatic lymph nodes in follow up patients. These patients usually present with vague abdominal pain or discomfort in case of vascular involvement, decreased urine output or flank pain due to obstructive uropathy in case of ureteric involvement. Bone infiltration can cause bone pain and pathological fractures. In our study, 14 of 16 patients with infiltrative nodes presented with vague abdominal pain, discomfort and vomiting. Majority of these patients were having vascular invasion. Two patients with bone pain at the time of follow up imaging showed infiltrative bone metastasis. It is important to note that none of these patients had mass in the region of vault or cervix at the time of presentation, which re-emphasizes multi-disciplinary approach and clinic-radiological correlation that can avoid biopsies in appropriate clinical scenario.
This study highlights the vital role of cross-sectional imaging in baseline assessment and staging of the patients with carcinoma cervix. It emphasizes to recognize the propensity of nodal metastases to infiltrate the adjoining organs in these patients. This extranodal extension of the tumor has significant impact on the prognosis and survival of the cancer patients2425. The study had limitations due to its retrospective nature and inclusion of predominantly follow up scans. Since it was a cross-sectional and retrospective study, it could not be evaluated whether the nodal masses on follow up imaging were present as discrete lymph nodes at the time of baseline evaluation which could have added to the further understanding and yield of the study.
In conclusion, our study findings emphasized on the role of CT for staging and evaluation of patients with cervical carcinoma at the baseline. It would help in identification of lymph node metastasis in cervical carcinoma, which is crucial for guiding accurate management. Further, a small proportion of nodal metastases show infiltration into the adjacent organs and such findings on imaging can significantly alter the management plan.
Financial support & sponsorship: None.
Conflicts of Interest: None.






