Translate this page into:
Potential benefit of optimizing atrioventricular & interventricular delays in patients with cardiac resynchronization therapy
Reprint requests: Dr. Bozena Urbanek, Department of Electrocardiology, Medical University of Lodz, 251 Pomorska St, 92-213 Lodz, Poland e-mail: bozena_urbanek@op.pl
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
The clinical benefit of optimization (OPT) of atrioventricular delay (AVD) and interventricular delay (VVD) in cardiac resynchronization therapy (CRT) remains debatable. This study was aimed to determine the influence of AVD and VVD OPT on selected parameters in patients early after CRT implantation and at mid-term follow up (FU).
Methods:
Fifty two patients (61±10 yr, 23 males) with left bundle branch block, left ventricular ejection fraction (LVEF) ≤35 per cent and heart failure were selected for CRT implantation. Early on the second day (2DFU) after CRT implantation, the patients were assigned to the OPT or the factory setting (FS) group. Haemodynamic and electrical parameters were evaluated at baseline, on 2DFU after CRT and mid-term FU [three-month FU (3MFU)]. Echocardiographic measures were assessed before implantation and at 3MFU. The AVD/VVD was deemed optimal for the highest cardiac output (CO) with impedance cardiography (ICG) monitoring.
Results:
On 2DFU, the AVD was shorter in the OPT group, LV was paced earlier than in FS group and CO was insignificantly higher in OPT group. At 3MFU, improvement of CO was observed only in OPT patients, but the intergroup difference was not significant. At 3MFU in OPT group, reduction of LV in terms of LV end-diastolic diameter (LVeDD), LV end-systolic diameter, LV end-diastolic and systolic volume with the improvement in LVEF was observed. In FS group, only a reduction in LVeDD was present. In OPT group, the paced QRS duration was shorter than in FS group patients.
Interpretation & conclusions:
CRT OPT of AVD and VVD with ICG was associated with a higher CO and better reverse LV remodelling. CO monitoring with ICG is a simple, non-invasive tool to optimize CRT devices.
Keywords
Cardiac resynchronization therapy
impedance cardiography
left ventricular remodelling
non-invasive optimization
Cardiac resynchronization therapy (CRT) improves left ventricular (LV) performance. Optimization (OPT) of two important adjustable pacing parameters the atrioventricular delay (AVD) and the interventricular delay (VVD) may play an important role in the further improvement of clinical and echocardiographic benefits of CRT. The AVD and VVD programming influence on LV capacity assessed either with echocardiography measures or with alternative methods12. However, randomized and non-randomized trials evaluating the effects of AVD and/or VVD OPT on various clinical or echocardiographic outcomes at mid-term or long-term follow up (FU) have not clearly defined whether CRT OPT provides incremental benefit over empiric device programming3456. We undertook this study to examine the impact of AVD and VVD OPT on haemodynamic, echocardiographic and electrical outcomes in patients in early and mid-term FU after CRT implantation.
Material & Methods
Patients (n=52) who were admitted for the primary implant with biventricular pacemakers or defibrillators (CRT) were prospectively enrolled. All patients were implanted CRT due to stable but advanced heart failure according to the I/IIa Class Criteria recommended by the European Cardiac Society in 20107. The patients were enrolled at the department of Electrocardiology, Medical University of Lodz, Lodz, Poland, between March 2011 and April 2013. Electrical and haemodynamic evaluations were performed at baseline and early on the second day FU (2DFU) and mid-term FU - three-month FU (3MFU) after implantation of CRT. Echocardiographic outcomes were evaluated at baseline and 3MFU. On the 2DFU, patients were randomly assigned into impedance cardiography (ICG) AVD/VVD OPT group versus factory setting (FS) group. Exclusion criteria were as follows: acute cardiac failure, coronary artery bypass graft or myocardial infarction within the previous three months, valvular stenosis, atrial fibrillation, supraventricular and ventricular tachyarrhythmias, premature ventricular extrasystolic. The study was approved by the Institutional Ethics Committee, and all patients gave written informed consent.
Implantation and lead position: Biventricular systems were implanted with LV pacing lead inserted transvenously through the coronary sinus with the help of an 8 Fr guiding catheter into the ventricular branches. A coronary sinus venogram was routinely obtained before the introduction of LV lead. LV leads were positioned in right anterior oblique 30° and left anterior oblique 40° projection. The final position of LV lead was as described in the guidelines for cardiac pacing and CRT8. After the placement of the LV lead, the right ventricular (RV) lead was positioned at the apex and the right atrial lead in the atrial appendage, following routinely and widely accepted techniques9. After implantation, the devices were programmed with DDDBiV (biventricular sequential pacing) mode at 40 ppm with AVD 120 msec and VVD 0 msec until OPT.
Cardiac resynchronization therapy (CRT) optimization (OPT) protocol: The AVD and VVD OPT were performed with ICG monitoring. The ICG measures were taken in a silent environment to minimize the impact of sympathetic activation. All patients were in a supine position and initially remained 10 min rested for stabilization and equilibration. During the collection of ICG data and OPT, all pacemakers were programmed in a DDD mode with a lower rate limit of 40 ppm to avoid effects of atrial pacing on the AVD10. During ICG data acquisition, at each pacemaker setting, telemetry between the pacemaker and programmer was turned off to minimize interference11. Simultaneously to the ICG, the 12-surface electrocardiogram (ECG) was collected. The period for each measurement of cardiac output (CO) in both groups was preceded by a stabilization period of 1 min, and at each stage, measurements were made four times, with 20 beats for each reading. The average of all readings was calculated. The optimal setting was defined as the result of the highest CO value. In both groups, the value of CO at baseline [without pacing (CRT-off)] and then with AVD and VVD FS was measured. Next, in the OPT group, the standard CRT OPT protocol was performed. The OPT procedure started with OPT of the AVD from 80 to 140 msec in increased steps of 20 msec during simultaneous biventricular pacing with VVD set at 0 msec. The optimal AVD was defined as the AVD that showed the highest CO. AVD values longer than 140 msec were not analyzed because of possible fusion with native AV conduction. When the AVD was optimized, the optimal VVD was searched. The VVD OPT was performed starting with LV pacing preceding right ventricular (RV) pacing. The range of VVD contained LV and RV pre-excitation values (from −60 to +60 msec; minus stands for LV being paced first) in 20 msec altered according to the previously published methods12. The VVD producing the highest CO was set as an optimal. Finally, the device was programmed with a combination of optimal AVD and VVD (optimal AVD/VVD). The same evaluations were repeated at 3MFU.
Impedance cardiography (ICG): Reocardiography is a repetitive, non-invasive, relatively easy and cheaper method than the echocardiography, and therefore, it has already found application in selection of optimal AVD and VVD in patients with implanted CRT pacemaker1314. The measurement of the resistance of the chest during cycle of a heart beat is the essence of the ICG. Fluctuations of the resistance of blood flow in the aorta during the heart beating allows to calculate CO and other haemodynamic parameters such as stroke volume (SV), preload (the measurement of thoracic fluid content), afterload [the measurement of systemic vascular resistance (SVR), the SVR index], the velocity index, the pre-ejection period (PEP) and LV ejection time. ICG was performed with a commercially available NICCOMO system (the CardioScreen®-device, Medizinische Messtechnik GmbH).
Echocardiographic examination: All patients underwent a comprehensive examination including M-mode, B-mode and Doppler echocardiography with Sonos 5500, S3 probe (Hewlett Packard, USA) before and three months after CRT implantation. Harmonic option was used to enhance the visualization of the endocardium. Measurements were averaged from three cardiac cycles. Pulse-wave Doppler LV and LV outflow tract velocities were obtained at end expiration, from the apical and parasternal windows, respectively, at a sweep speed of 50-100 mm/sec. LV end-diastolic diameter (LVeDD) and LV end-systolic diameter (LVeSD) and LV end-systolic volume (LVeSV) and LV end-diastolic volume (LVeDV) were measured using Simpson's biplane method15; LV ejection fraction (LVEF) and mitral regurgitation were assessed. LV and RV PEPs were measured as the time from the onset of the QRS complex on the ECG to the onset of systolic flow from the LV and RV outflow tracts. VV dyssynchrony was evaluated by means of the interventricular mechanical delay (IVMD) calculated as the difference between the left and right PEP.
Statistical analysis: The data are presented as mean and standard deviation for continuous variables and as proportions for categorical variables. The differences between normally distributed variables were assessed by Student's t test. Continuous skewed data were compared with Mann–Whitney test and Wilcoxon rank test for independent and dependent observations, respectively. Discrete variables were compared using the Chi-square test or Fisher's exact test, where appropriate.
Results
A total of 52 patients were enrolled (23 males, mean age 60±10 yr). Thirty seven patients were assigned to the OPT group and 15 to the FS group. One patient from the FS group did not complete the 3MFU because of death. Baseline clinical and echocardiographic characteristics of the study population are shown in Table I. There were no significant differences in clinical characteristics between the two study groups at baseline.

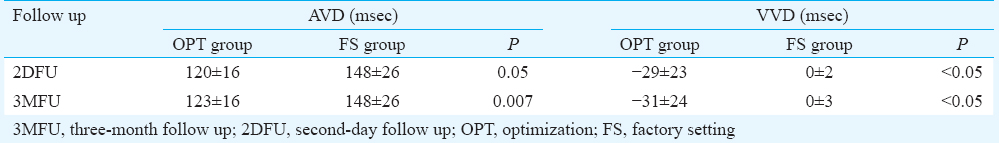
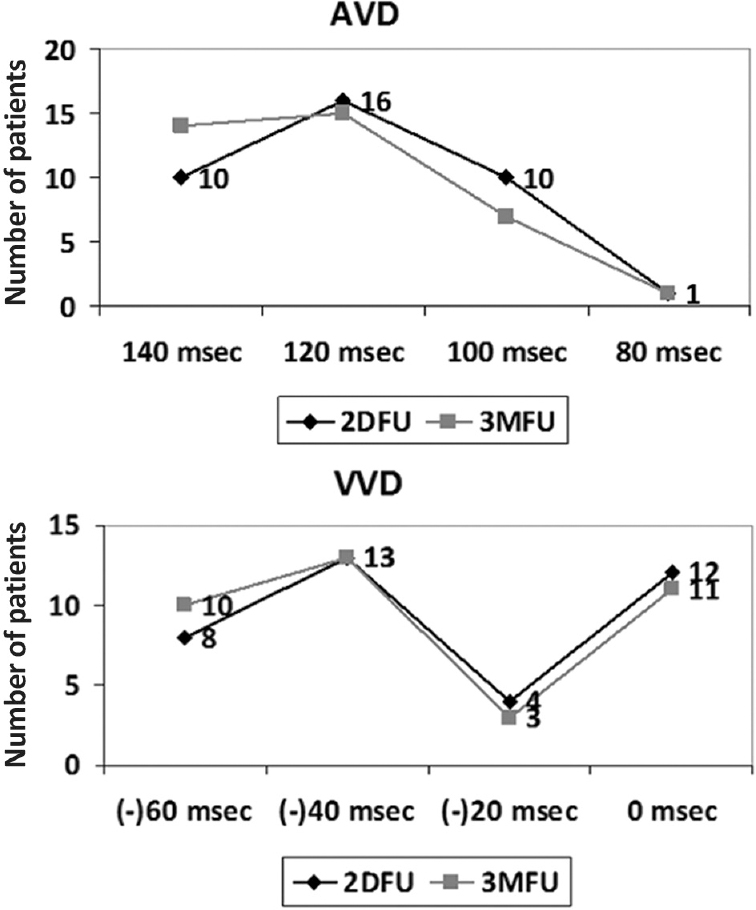
Early post-implantation effect of atrioventricular and interventricular delays (AVD and VVD) optimization (OPT): On the 2DFU, the value of CO between both groups did not differ significantly (OPT: 4.64±1.2 vs. 4.48±0.9 l/min in FS). Compared to the baseline, post-implantation, an improvement of CO was observed in both groups on the FS (OPT: 3.72±0.9 vs. 4.34±1.1 l/min, FS: 4.22±1 vs. 4.48±0.9 l/min, for both: P<0.05). Furthermore, in the OPT group, the OPT of AVD/VVD insignificantly increased CO (4.34±1.1 l/min vs. 4.64±1.2 l/min). Compared to the baseline, CO increased by 0.92 l/min (3.72±0.9 l/min vs. 4.64±1.2 l/min, P<0.05) (Fig. 1). The haemodynamic improvement (defined as >10% increase of CO) was observed in both groups. On the 2DFU, there was a trend toward better hemodynamic response among patients in OPT group [25 (67%) vs. 3 (21%) patients, P<0.05]; however, at 3MFU, the difference between groups was lower and non-significant [29 (78%) vs. 7 (50%) patients]. The AVD after the OPT was shorter in OPT group (120±16 msec vs. 148±26, P<0.05). In OPT group, LV was paced significantly earlier than in FS group where the simultaneous biventricular pacing was set (−29±23 vs. 0±2 msec, P<0.05) (Table II). The majority of the patients in the OPT group were finally set on AVD 120 msec and VVD 40 msec with LV pre-activation (Fig. 2).
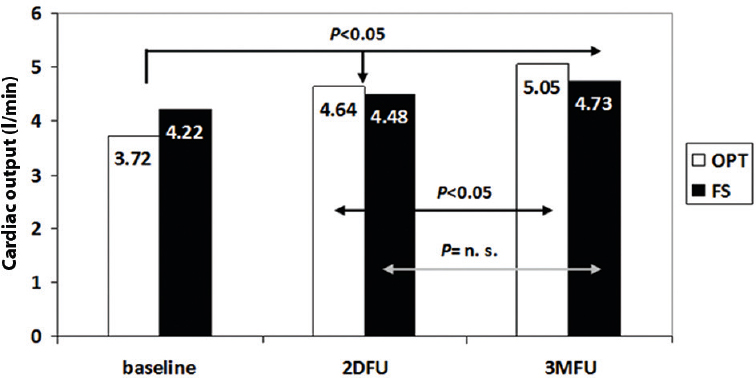
- The value of cardiac output in optimization (OPT) and factory setting (FS) groups. 2DFU, second day follow up; 3MFU, three month follow up; n.s., not significant.
- Atrioventricular (AVD) and interventricular delays (VVD) on the second day and at three-month follow up (2DFU, 3MFU) in the optimization group.
An improvement of QRS duration at 2DFU was observed in the OPT group from 173±29 to 156±29 msec (P<0.05). In the FS group, shortening of QRS was not observed. No difference between the groups was observed.
Mid-term effect of atrioventricular and interventricular delays (AVD and VVD) optimization (OPT): At 3MFU, the haemodynamic outcome was slightly higher in the OPT group (5.05±1.2 vs. 4.73±0.9 l/min). In addition, compared to 2DFU in this group, increased CO by 0.41 l/min (4.64±1.2 vs. 5.05±1.2 l/min, P<0.05, respectively) was observed. However, in FS group, the CO did not change significantly at 3MFU (4.48±0.9 vs. 4.73±0.9 l/min) (Fig. 1).
In the OPT group, re-OPT of AVD and VVD was performed and CRT was reprogrammed in some patients (Fig. 2). However, the AVD still remained shorter in OPT group (123±16 vs. 148±26 msec, P=0.007), and similarly to 2DFU, LV was paced significantly earlier in OPT than in FS group (−31±24 vs. 0±3 msec, P<0.05) (Table II).
At 3MFU, lack of an improvement of QRS duration in both groups was observed, but there was a significant difference across groups (OPT vs. FS: 156±31 vs. 165±15 msec, P<0.01). In the OPT group, significant LV reverse remodelling and capacity improvement were observed at baseline to 3MFU. LVeDV decreased from 246±68 to 227±76 ml (P<0.05), whereas LVeSV decreased from 179±55 to 156±66 ml (P<0.05). LVeDD and LVeSD decreased as follows: 73±9 vs. 70±10 and 61±10 vs. 55 ± 12 mm, for both P<0.05, respectively. This resulted in an increase of the LVEF from 26±4 to 33±10 per cent (P<0.05).
In the FS group, LV reverse remodelling was observed only in LVeDD from 72±8 to 69±8 mm (P<0.05). In both groups, echo demonstrated a reduction in IVMD (OPT from 50±23 to 40±18 msec, FS from 53±23 to 30±20 msec, for both, P<0.05). However, no significant differences in echocardiographic response were found between the two groups.
Discussion
In clinical practice, AVD and VVD OPT are not routinely performed after CRT implantation in the majority of centres. The individual adjustment of the VV interval is often underestimated in clinical practice16. Clinical studies have shown that the OPT of the VVD can improve cardiac function in addition to the improvement obtained with simultaneous biventricular pacing6171819. ICG was positively evaluated as a valuable tool for CRT OPT1819. Turcott et al20 showed that AV and VV adjustment done with ICG, as well as echocardiography, led to haemodynamic improvement in the majority of patients. Other authors revealed that ICG OPT in CRT population significantly increased CO1221. Heinroth et al21 showed that early after implantation (3-5 days), modification of both AV and VV intervals in patients with CRT significantly improved CO compared with standard simultaneous biventricular pacing and ICG was a useful non-invasive technique for guiding this modification. They found that mean CO was significantly higher during simultaneous biventricular pacing than without any pacing. In our group, on the second day after implantation (2DFU), we also observed a similar tendency. The CO value was approximately 1 l/min higher after CRT implantation and AVD/VVD OPT and only slightly better if CRT was programmed on default manufacturer settings. Khan et al12 in a similar population performed AVD/VVD OPT with the non-invasive CO monitoring (NICOM). They were evaluated on the 14th day after implantation, and a significant increase of CO was observed in all patients with optimized settings (AVD/VVD optimal) if compared with baseline (5.66 vs. 4.35 l/min, P<0.001). Similar improvements were seen in velocity time integral (VTI) of aortic flow, and there was a good correlation between paired VTI and NICOM readings (r=0.67, P<0.01). Other studies2223 showed that CRT optimized with VTI determined SV improvement by 10-20 per cent in the vast majority (even up to 81%) of patients. Our study prospectively evaluated the potential benefit gathered with AVD and VVD OPT by ICG over FSs programmed CRT patient. It was found that the AVD/VVD OPT led to the trend for haemodynamic improvement more often than the FSs acutely and even lower insignificant tendency in mid-term FU. The average AVD in optimized CRT patients ranges from 95±22 to 132±27 msec1124, which is similar to our findings (120±16 msec). In CRT patients, VVD OPT may lead to further haemodynamic improvement6. Bogaard et al25 showed that VVD OPT performed additionally to AVD led to haemodynamic improvement in 23-45 per cent patients. The most beneficial VVD was 40 msec LV pre-activation25 which was similar to our findings. Moreover, we did not observe a difference between optimized AVD and/or VVD early after implantation and in mid-term FU. O’Cochlain et al26 have shown CRT OPT influence on QRS width. Only six patients of their group (23%) had maximal shortening of the paced QRS with simultaneous activation of the LV and RV. The shortest paced QRS duration was most often produced by an LV to RV interval of −30 msec. This OPT of VVD resulted in an additional 13 per cent shortening of the paced QRS if compared to simultaneous pacing. In our study, OPT of AVD/VVD reduced pacing QRS which was coherent with findings of other authors.
Several studies suggested beneficial influence of CRT OPT on echocardiographic parameters. Khan et al11 revealed that non-invasive CRT OPT was associated with favourable echocardiographic response. In optimized patient, lower LVeSV (108±51 vs. 126±60 ml, P=0.01) and higher LVEF (30±7 vs. 27±8%, P=0.01) were observed if compared to empiric settings. The positive influence of CRT on LV reverse remodelling was observed in another study by Khan et al12. Compared to baseline, optimized biventricular pacing caused a significantly reduced LVeSV associated with an increased LVEF similar to our mid-term FU (three months). Sogaard et al16 showed that simultaneous CRT resulted in an increase of LVEF from 22.4±6 to 29.7±5 per cent (P<0.01), but AVD/VVD OPT led to further increase (from 29.7±5 to 33.9±6%, P<0.01). Surprisingly, these authors observed further improvement in the 3MFU, when LVEF per cent increased from 33.6±6 to 38.6±7.2 per cent, (P<0.01). CRT OPT in our study led to LV reverse remodelling. A decrease in LVeDV, LVeSV, LVeDD and LVeSD was observed, whereas LVEF was significantly increased. In FS group, LV reverse remodelling was observed only in LVeDD. In both groups, a reduction was noticed in IVMD (OPT from 50±23 to 40±18 msec, FS from 53±23 to 30±20 msec, for both, P<0.05), which was also observed in another study27. Thus, CRT caused a significant reduction in the disorders in VV conduction regardless of AVD and VVD OPT.
Our study had some limitations. The investigated group was relatively small which could influence the analysis. The benefit of OPT of CRT settings may be different in patients with ischemic and non-ischemic cardiomyopathy.
In conclusion, the OPT of AVD and VVD in CRT patients with NICOM may provide an additional benefit in terms of haemodynamic improvement and LV reverse remodelling. NICOM is a simple, reliable method to the optimal programming of CRT devices.
Conflicts of Interest: None.
References
- How should we optimize cardiac resynchronization therapy? Eur Heart J. 2008;29:2458-72.
- [Google Scholar]
- Why, how and when do we need to optimize the setting of cardiac resynchronization therapy? Europace. 2009;11(Suppl 5):v46-57.
- [Google Scholar]
- Atrioventricular delay optimization by doppler-derived left ventricular dP/dt improves 6-month outcome of resynchronized patients. Pacing Clin Electrophysiol. 2006;29:564-8.
- [Google Scholar]
- Randomized comparison of simultaneous biventricular stimulation versus optimized interventricular delay in cardiac resynchronization therapy. The Resynchronization for the HemodYnamic Treatment for Heart Failure Management II implantable cardioverter defibrillator (RHYTHM II ICD) study. Am Heart J. 2006;151:1050-8.
- [Google Scholar]
- Reduced ventricular volumes and improved systolic function with cardiac resynchronization therapy: A randomized trial comparing simultaneous biventricular pacing, sequential biventricular pacing, and left ventricular pacing. Circulation. 2007;115:2136-44.
- [Google Scholar]
- Randomized controlled trial comparing simultaneous versus optimized sequential interventricular stimulation during cardiac resynchronization therapy. Am Heart J. 2012;164:735-41.
- [Google Scholar]
- 2010 focused update of ESC guidelines on device therapy in heart failure. Europace. 2010;12:1526-36.
- [Google Scholar]
- Guidelines for cardiac pacing and cardiac resynchronization therapy: The Task Force for Cardiac Pacing and Cardiac Resynchronization Therapy of the European Society of Cardiology. Developed in collaboration with the European Heart Rhythm Association. Eur Heart J. 2007;28:2256-95.
- [Google Scholar]
- Clinical cardiac pacing, defibrillation and resynchronization therapy (4th ed). Philadelphia, United States: Elsevier-Health Sciences Division; 2011.
- Right atrial pacing impairs cardiac function during resynchronization therapy: Acute effects of DDD pacing compared to VDD pacing. J Am Coll Cardiol. 2005;45:1482-7.
- [Google Scholar]
- Cardiac resynchronization therapy optimization using noninvasive cardiac output measurement. Pacing Clin Electrophysiol. 2011;34:1527-36.
- [Google Scholar]
- Non-invasive cardiac output measurements based on bioreactance for optimization of atrio- and interventricular delays. Europace. 2009;11:1666-74.
- [Google Scholar]
- Impedance cardiography for cardiac output estimation in pacemaker patients: Review of the literature. Pacing Clin Electrophysiol. 1993;16(7 Pt 1):1412-22.
- [Google Scholar]
- Variability of cardiac output as determined by impedance cardiography in pacemaker patients. Am J Cardiol. 1993;72:183-7.
- [Google Scholar]
- Optimization of AV and VV delays in the real-world CRT patient population: An international survey on current clinical practice. Pacing Clin Electrophysiol. 2009;32(Suppl 1):S236-9.
- [Google Scholar]
- Sequential versus simultaneous biventricular resynchronization for severe heart failure: Evaluation by tissue Doppler imaging. Circulation. 2002;106:2078-84.
- [Google Scholar]
- Simultaneous vs.sequential biventricular pacing in dilated cardiomyopathy: An acute hemodynamic study. Eur J Heart Fail. 2003;5:305-13.
- [Google Scholar]
- Echocardiographic parameters of ventricular dyssynchrony validation in patients with heart failure using sequential biventricular pacing. J Am Coll Cardiol. 2004;44:2157-65.
- [Google Scholar]
- Measurement precision in the optimization of cardiac resynchronization therapy. Circ Heart Fail. 2010;3:395-404.
- [Google Scholar]
- Impedance cardiography: A useful and reliable tool in optimization of cardiac resynchronization devices. Europace. 2007;9:744-50.
- [Google Scholar]
- Cardiac resynchronization with sequential biventricular pacing for the treatment of moderate-to-severe heart failure. J Am Coll Cardiol. 2005;46:2298-304.
- [Google Scholar]
- Tailored echocardiographic interventricular delay programming further optimizes left ventricular performance after cardiac resynchronization therapy. Heart Rhythm. 2005;2:1066-72.
- [Google Scholar]
- Association between frequent cardiac resynchronization therapy optimization and long-term clinical response: A post hoc analysis of the Clinical Evaluation on Advanced Resynchronization (CLEAR) pilot study. Europace. 2013;15:1174-81.
- [Google Scholar]
- Cardiac resynchronization therapy beyond nominal settings: Who needs individual programming of the atrioventricular and interventricular delay? Europace. 2012;14:1746-53.
- [Google Scholar]
- The effect of variation in the interval between right and left ventricular activation on paced QRS duration. Pacing Clin Electrophysiol. 2001;24:1780-2.
- [Google Scholar]
- Clinical versus echocardiographic parameters to assess response to cardiac resynchronization therapy. Am J Cardiol. 2006;97:260-3.
- [Google Scholar]






