Translate this page into:
Oculomotor nerve palsy in dengue encephalitis - a rare presentation
*For correspondence: drsourenpal@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 14 yr old female presented to the department of Medicine, Nilratan Sircar Medical College and Hospital, Kolkata, India, in August 2013 with a history of high fever and headache for the last 13 days followed by drooping of right upper eyelid with diplopia. She had neck rigidity with positive kernig sign. There was ptosis in right eye (Fig. 1) with absence of light reflex (Figs. 2, 3) (direct & consensual) and right eye movements were restricted in all direction except for abduction and intorsion.

- Drooping of right upper eyelid - weakness of levetor palpabrae superioris supplied by third cranial nerve.

- Absence of ipsilateral light reflex - pupil of right eye remains dilated even after fall of light beam along with ipsilateral drooping of upper eye lid.

- Absence of ipsilateral light reflex - pupil of right eye remains dilated even after fall of light beam.
She had dengue specific IgM reactive serum and CSF showed viral picture with no reactivity for dengue, chikungunia, and Japanese encephalitis (JE). Magnetic resonance imaging (MRI) scan of brain showed hyperintensity in T2 and FLAIR (Fluid Attenuated Inversion Recovery), involving supratentorial, both posterior periventricular and left frontotemporoparietal lobes with effacement of the cortical sulci and hyperintense in FLAIR at temporo parietal lobe (Figs. 4, 5, 6). MR angiography showed no abnormality. This clinical picture revealed a rare aetiology in oculomotor paralysis1.
The patient was treated with intravenous fluids and antipyretics. Her diplopia was resolved completely but ptosis was partially resolved at the time of discharge after two weeks.
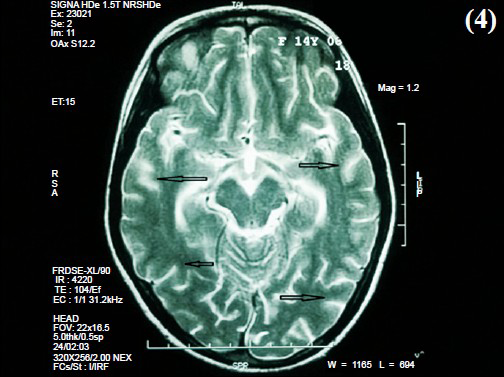
- Effacement of cortical sulci (arrows) - Sequelae of encephalomyelitis.
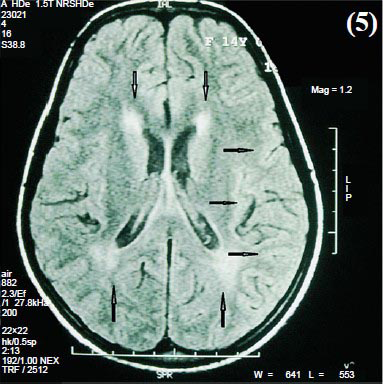
- White matter hyper intensity involving both posterior periventricular and left frontotemporoparietal lobes (arrows) - Sequelae of encephalomyelitis.
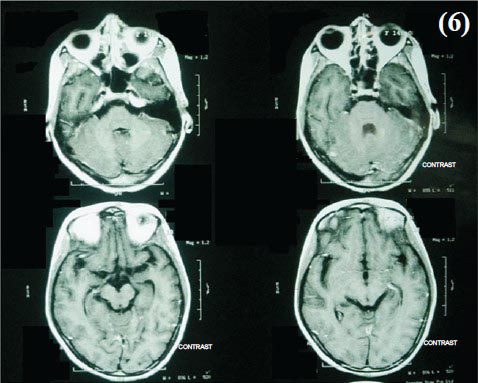
- No abnormal parenchymal and meningeal enhancement was noted.





