Translate this page into:
Mobilizing community-based health insurance to enhance awareness & prevention of airborne, vector-borne & waterborne diseases in rural India
Reprint requests: Dr Pradeep Panda, Micro Insurance Academy, 86, Okhla Industrial Estate, Phase III, New Delhi 110 020, India e-mail: pradeep@mia.org.in
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Despite remarkable progress in airborne, vector-borne and waterborne diseases in India, the morbidity associated with these diseases is still high. Many of these diseases are controllable through awareness and preventive practice. This study was an attempt to evaluate the effectiveness of a preventive care awareness campaign in enhancing knowledge related with airborne, vector-borne and waterborne diseases, carried out in 2011 in three rural communities in India (Pratapgarh and Kanpur-Dehat in Uttar Pradesh and Vaishali in Bihar).
Methods:
Data for this analysis were collected from two surveys, one done before the campaign and the other after it, each of 300 randomly selected households drawn from a larger sample of Self-Help Groups (SHGs) members invited to join community-based health insurance (CBHI) schemes.
Results:
The results showed a significant increase both in awareness (34%, p<0.001) and in preventive practices (48%, P=0.001), suggesting that the awareness campaign was effective. However, average practice scores (0.31) were substantially lower than average awareness scores (0.47), even in post-campaign. Awareness and preventive practices were less prevalent in vector-borne diseases than in airborne and waterborne diseases. Education was positively associated with both awareness and practice scores. The awareness scores were positive and significant determinants of the practice scores, both in the pre- and in the post-campaign results. Affiliation to CBHI had significant positive influence on awareness and on practice scores in the post-campaign period.
Interpretation & conclusions:
The results suggest that well-crafted health educational campaigns can be effective in raising awareness and promoting health-enhancing practices in resource-poor settings. It also confirms that CBHI can serve as a platform to enhance awareness to risks of exposure to airborne, vector-borne and waterborne diseases, and encourage preventive practices.
Keywords
Airborne disease
awareness campaign
community-based health insurance
preventive healthcare
rural India
vector-borne disease
waterborne disease
Despite remarkable reduction in airborne, vector-borne and waterborne diseases, the morbidity and mortality associated with these conditions continue to be high in India. India accounted for 21 per cent of the world's burden of disease in 20101. Diseases such as tuberculosis, malaria, filariasis, dengue, diarrhoea, typhoid, etc. are endemic in India2. According to Cohen3, 1.6 million deaths were caused in India by indoor and outdoor air pollution in 2010. Similarly, India had close to one million confirmed cases of malaria, and many malaria deaths (estimates varied from 15,0004 to 200,000 individuals every year5). On waterborne diseases (e.g. cholera, acute diarrhoea, typhoid and viral hepatitis) the estimates vary widely because of a lack of reporting and poor surveillance, yet one report estimated that around 14 million people suffered from some of these conditions in 20126.
Many such diseases are preventable through low-cost preventive practices. Public health experts and researchers have recognised that health education is an important tool to encourage individual health-promoting choices789. However, the evidence is inconsistent. One study reported that an awareness campaign in Vietnam was successful in enhancing people's early access to health care after they acquired more knowledge about avian influenza9. Another study reported that in China, short-term health education was not associated with adoption of health protecting behaviour10. In the Indian scenario, one study found that information, education and communication (IEC) campaigns were effective in enhancing awareness on tuberculosis11. Another, in Karnataka, informed that local folk theatre generated a significant impact on awareness, which led to a reduction in malaria incidence7. A study in tribal areas of Odisha concluded that after the awareness campaign about mosquito bites, most participants adopted the recommended preventive measure of using insecticide treated bed nets (ITBN)12. In rural Tamil Nadu, awareness generation to waterborne diseases left gaps in understanding the connection between using contaminated drinking water and disease13. Finally, in high chikungunya prevalent areas in urban India, there was no significant association between respondents’ education level and emptying/drying of water containers14.
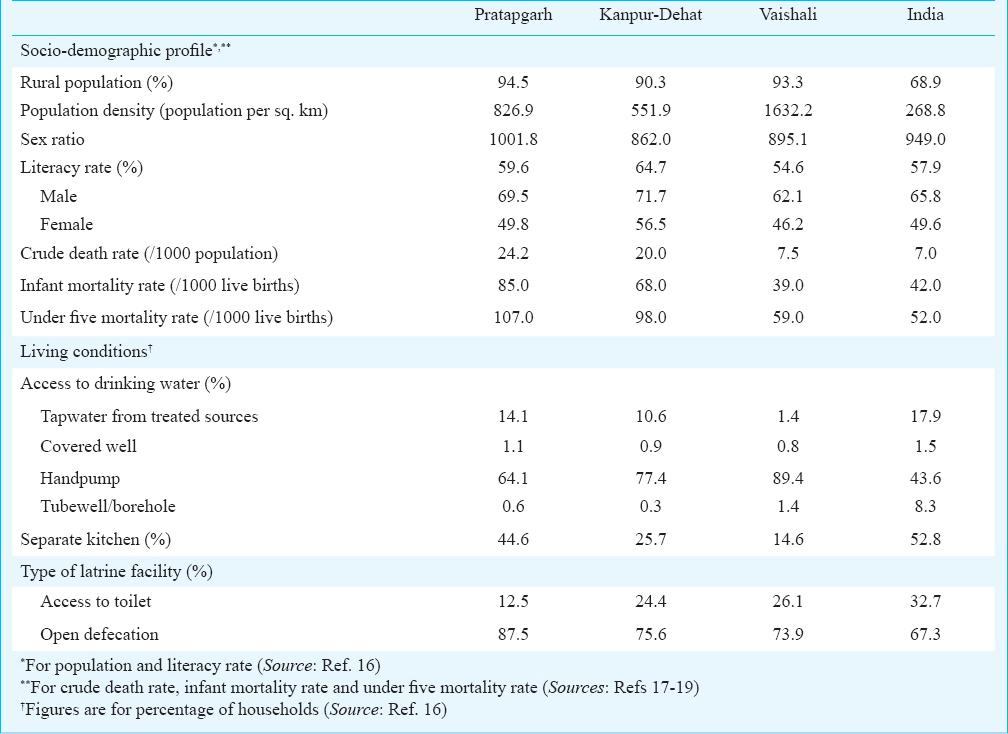
In this study, we evaluated the effectiveness of awareness campaigns in increasing knowledge about airborne, vector-borne and waterborne diseases, as well as enhancing preventive practices among rural communities. The study was conducted in Pratapgarh and Kanpur-Dehat districts in Uttar Pradesh and Vaishali district in Bihar, India; all located in humid semi-arid climate in the Ganges River plain15. All the three sites are predominantly rural and more than the one-third of the population is illiterate (Table I). Crude death rates and under five mortality rates are higher than the all India rural average.
Material & Methods
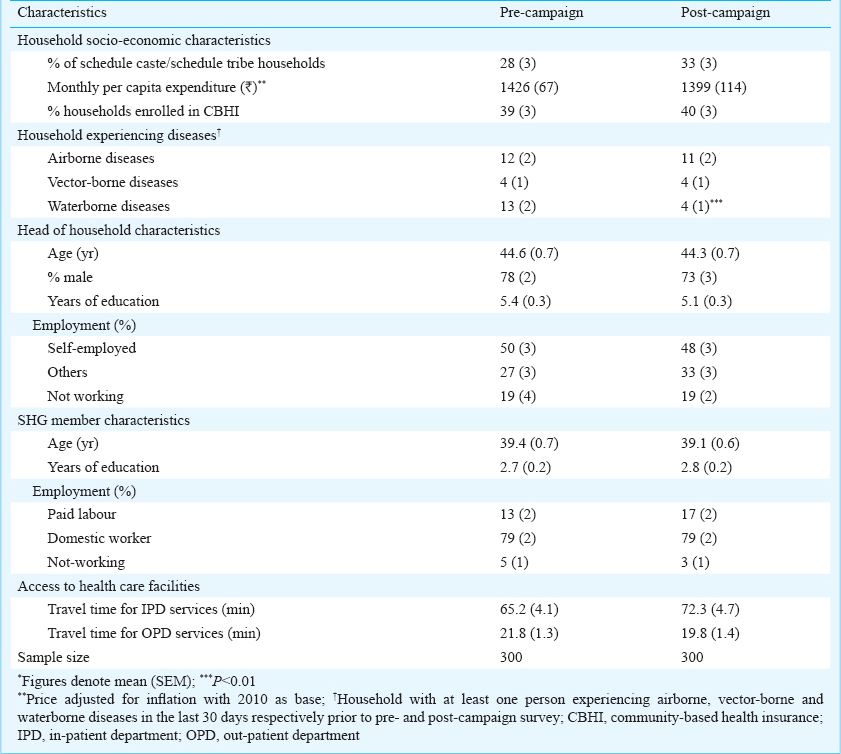
Project background: The awareness campaigns were part of a larger project carried out by Micro Insurance Academy, New Delhi, India, that included the launch of three community-based health insurance (CBHI) schemes in 2011 in these locations. The CBHI schemes under this project were designed as a cluster randomized control trial20, located 50-100 km outside major urban centres in poor rural areas. There were three waves of enrollment, in 2011, 2012 and 2013. In total, 3,685 households (1,283, 1,039 and 1,363 from Pratapgarh, Kanpur-Dehat and Vaishali, respectively) were selected as treatment cohorts, and all filled the condition that in each household, at least one woman was registered in March 2010 as a member of a Self-Help Group (SHG) facilitated by the three field partners. The treatment groups were exposed to insurance education programmes prior to being invited to join the schemes. Households were characterised by low levels of education, and limited access to healthcare (Table II).
The CBHI schemes targeted communities sharing a common background (geographical, economic, occupational, ethnic, gender, etc.). The communities were involved in the design and selection of the benefit packages. The schemes were characterized by low premium and mutual-aid structure, i.e. the CBHI schemes were owned and managed by the enrolled community members and operated on a not-for-profit basis21. The prevalence was estimated by using the baseline data (collected prior to the launch of CBHIs); more than half of the households had experienced at least one chronic illness episode, and more than two-third reported an acute illness in the family during one month before the survey. More specifically to our study, more than 25 per cent of the sampled households reported an airborne or a vector-borne or a waterborne ailment. Hence, the awareness campaigns were launched, which were open to insured and uninsured households alike.
The awareness campaigns: The campaigns on awareness to preventive care were an application of the theory of “reasoned action and planned behaviour” (a theory about the link between beliefs and behaviour, which suggests that a person's behaviour is determined by his/her intention to perform the behaviour, which in turn reflects his/her attitudes and his/her subjective norms)22. The awareness campaigns entailed training of all the SHG groups that were under the CBHI project. The campaign was organized as a Training of Trainers (ToT) activity; trainers from the lead institution trained representatives of the three field partners about the use of various tools and the key messages; this unfolded during September-October 2011 in all three locations. The field partners’ trainers, in turn, trained representatives selected by the SHG members at clusters of villages. These trained SHG members conducted group discussions at SHG meetings on awareness to airborne, vector-borne and waterborne diseases; messages included key identifiable symptoms and associated preventive measures that everyone could practice on a daily basis without reliance on professional assistance or supervision. Pursuant to group discussions, practical exercises followed, like preparation of ORS (oral rehydration solution). Following group discussions, the trainers facilitated follow up discussions at household level of families of SHG members, to cascade the effect of the campaign beyond only the SHG participants.
The campaign tools included group discussion and flipbooks. The flipbooks contained written and pictorial messages, developed by trained physicians of the lead institution, with inputs from the community representatives of the three sites on local beliefs and practices. The flipbooks were written in English, translated into Hindi (the local language).
Data and methodology: Two sources of data were used for this study:
Pre-campaign survey data - In August 2011, 300 households (100 each in Pratapgarh, Kanpur-Dehat and Vaishali), randomly selected from the CBHI project sample of 3,685, were asked to respond to questions as to how airborne, vector-borne and waterborne diseases could be identified, how these spread and how these could be prevented. Information of the socio-economic characteristics of respondents, health events in the household during one month prior to the survey and about their access to healthcare facilities was also collected. All data collection tools were pretested and finalized. Trained researchers collected information from the selected households, and the female SHG members were the respondents, using the non-prompted questionnaire.
Post-campaign survey data - In August 2012, the same questionnaire was re-used to probe 300 randomly selected households (not necessarily the same, but selected randomly from the CBHI project sample of 3,685 households; 100 households each in Pratapgarh, Kanpur-Dehat and Vaishali).
Comparison of pre- and post-campaign respondents: Although only seven of the 300 households were sampled in both the pre- and the post-campaigns, the two groups of households were comparable considering the key household indicators, incidence rates, characteristics of household heads and SHG members and access to health care facilities (Table II). Participation in the survey was based on informed consent, voluntary and confidential.
Calculation of awareness and practice scores: We measure the degree of awareness about preventive care and habits regarding preventive practices by scoring replies to a series of questions. Each correct answer was assigned a value of one and each incorrect reply a value of zero. For questions where multiple correct responses were possible, a score of one was assigned for each correct response. All individual scores were added for a single total score per respondent, reflecting all replies relating to airborne, vector-borne and waterborne diseases. Thus, the total scores for awareness could range from zero to 38 (0-12, 0-11 and 0-15 for airborne, vector-borne and waterborne, respectively); and for practice, the total scores could range between 0 and 25 (0-8, 0-8 and 0-9 for airborne, vector-borne and waterborne, respectively). For ease of comparison and comprehension, all total individual scores were divided by the number of questions, to obtain the average scores per question, which now range from zero to one.
Statistical analysis: Descriptive statistics were used for the analysis of changes in respondents’ awareness and practice responses. Differences between pre- and post-campaigns were assessed by using student t-test. Ordinary least square (OLS) regression was used to examine the factors explaining the overall awareness and practice scores, both in pre-campaign and post-campaign.
Results
Changes in awareness and practice scores: After the campaign, the results (Table III) showed that the average awareness scores on airborne diseases increased moderately, 20 per cent but significantly (P<0.001) for the entire sample and for Kanpur-Dehat and Vaishali. As for practice scores on airborne diseases, average scores increased significantly in all three locations after the campaign (+40% on reported practice score for the entire sample).
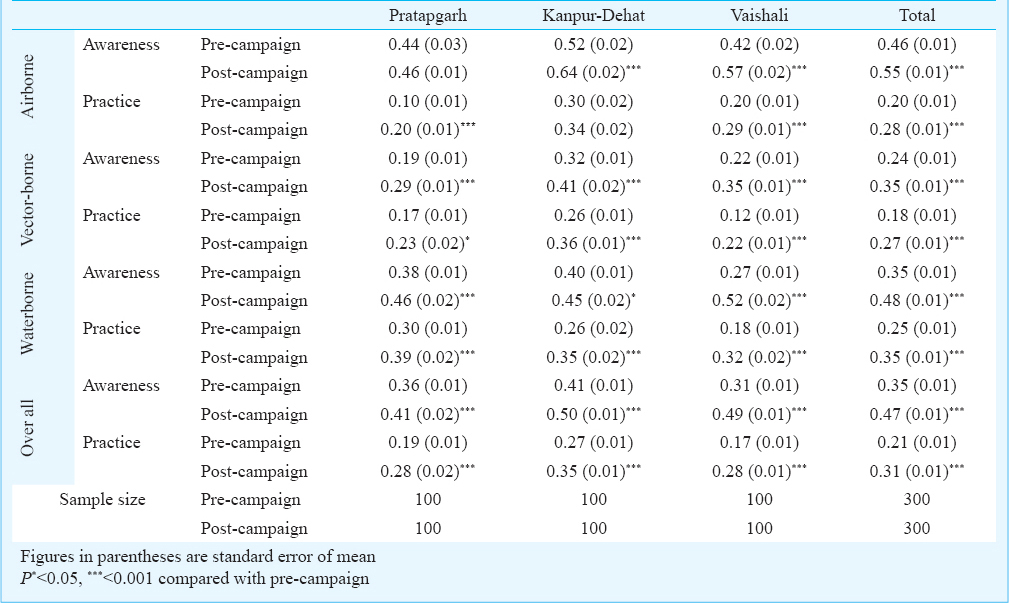
The average post-campaign awareness scores about vector-borne diseases were significantly higher in all three locations (Kanpur-Dehat 0.41; Vaishali 0.35; and Pratapgarh 0.29). The average practice scores increased by about 50 per cent in all locations after the campaign (P<0.001), but only 27 per cent of the sample reported practicing prevention post-campaign.
For waterborne diseases, the average awareness scores increased by +37 per cent (P<0.001); this reflected a very pronounced increase in Vaishali (+92%; P<0.001), and a modest improvement in Kanpur-Dehat (+12.5% P<0.05). Combining all three diseases, the average awareness post-campaign scores were higher than the pre-campaign scores (increase by 34%, P<0.001). This was the case for all three locations, but the extent of the increase was different (in Vaishali it was +58%, in Kanpur-Dehat it was +22%, and in Pratapgarh the change was merely +14%). As for the practice scores, the average scores increased by 48 per cent in the post-campaign for the entire sample (P<0.001); and in all three locations compared to the pre-campaign scores, but they were quite lower than the awareness scores, both before and after the campaign (Table III). It is noted that the campaign led to a higher improvement in practice scores than in awareness scores, with percentage changes of +65 per cent in Vaishali, +30 per cent in Kanpur-Dehat, and +47 per cent in Pratapgarh.
Changes in awareness and practices for airborne, vector-borne and waterborne diseases: The overall low scores even after the campaign (less than one-third correct replies), especially for practice, necessitated further analysis, which is shown in Tables IV, V and VI for airborne, vector-borne and waterborne diseases, respectively, for the entire sample.
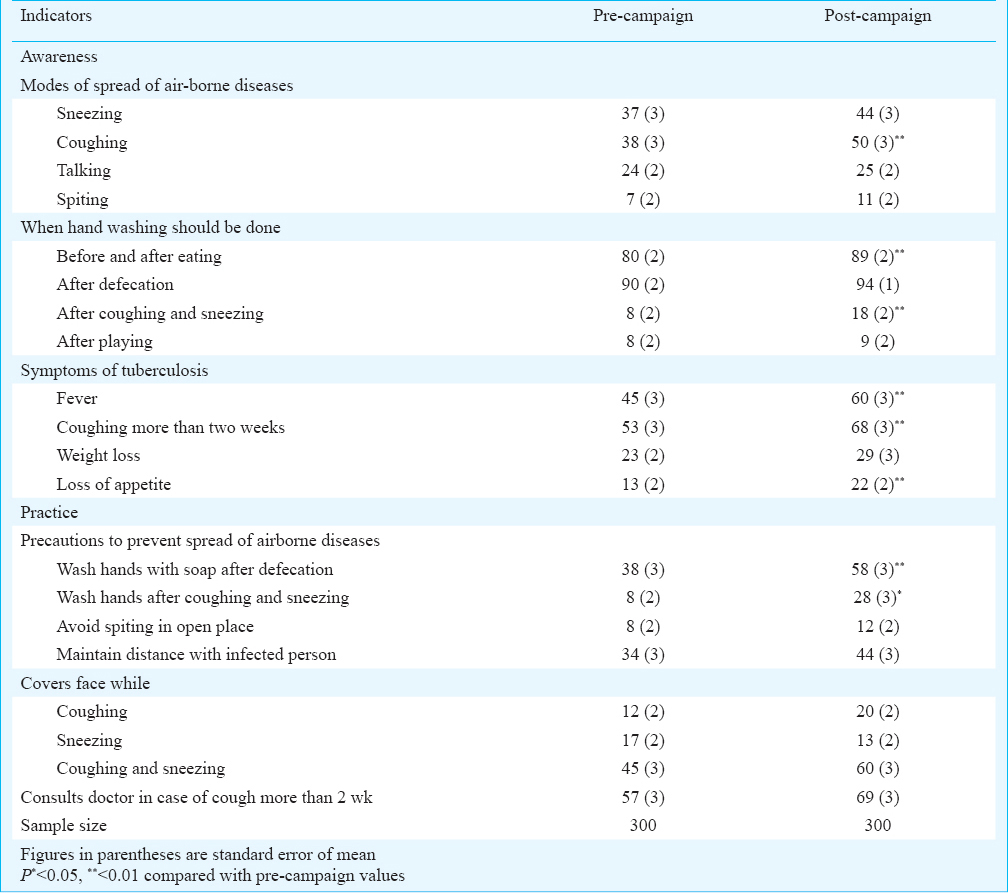

Airborne diseases: Overall, an increased number of respondents in the post-campaign period were aware that airborne diseases spread through sneezing and coughing (Table IV). Most of the respondents understood that washing hands before and after eating, and after defecation, prevented diseases. More than 60 per cent of the respondents recognized that fever and extended coughing (more than two weeks) were symptoms of TB, but most did not know, even after the campaign, that weight and appetite-loss were also possible indications of TB (less than 30%).
An increased number of respondents reported having adopted preventive practices, e.g. washing hands with soap after defecation (increase from 38 of 58% P<0.01) and after coughing and sneezing (28% in post-campaign vs. 8% in pre-campaign; P<0.05). In addition, 60 per cent of the respondents reported that they were covering faces while coughing and sneezing, and 69 per cent consulted a doctor when their coughing persisted for more than two weeks (Table IV).
The increase in awareness about airborne diseases from pre-campaign to post-campaign was much higher in Vaishali and Kanpur-Dehat than Pratapgarh (data not shown). But when it came to practicing preventive methods for airborne diseases, in Kanpur-Dehat respondents were well behind those from Pratapgarh and Vaishali.
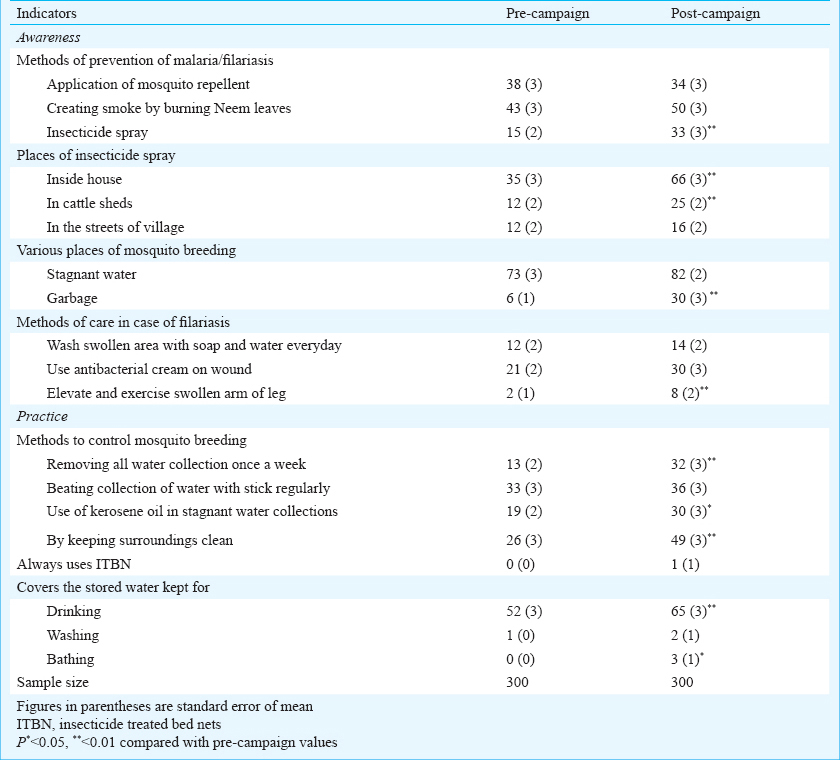
Vector-borne diseases: The respondents’ awareness rose significantly post-campaign about the effectiveness of spraying insecticide inside houses and cattle sheds to prevent malaria/filariasis (+18%; of correct replies; P<0.01) (Table V), and about the places that are prone to mosquito breeding. Awareness to various curative methods of filariasis also increased significantly. As regards practices, an increased number of respondents reported post-campaign that they were controlling mosquito breeding by removing water collections once a week (32%; P<0.01), using kerosene in stagnant water (30%; P<0.05) and keeping surroundings clean (49%; P<0.01). Close to two-thirds of the respondents reported that they kept drinking water containers covered.
The increase in awareness about vector-borne diseases was significantly higher in Vaishali, followed by Pratapgarh and Kanpur-Dehat (data not shown). Awareness to curative methods of filariasis also increased significantly in Pratapgarh and Vaishali (but remained very low even after the campaign).
The most notable increase in practices was in applying three methods to control mosquito breeding: removing water collections once a week, use of kerosene in stagnant water, and keeping surroundings clean. However, sleeping under ITBN was extremely rare in all three locations, even after the campaign (Table V).
Waterborne diseases: After the campaign, awareness increased on three of the four sources of water contamination, and on the three ways to prevent worm infection and two of the three symptoms of scabies (Table VI). Respondents exhibited better knowledge on how long ORS can be kept in store, how to clean clothes of scabies patients, and minimum time for boiling of drinking water and cooking non-vegetarian dishes. Moreover, in post-campaign replies, about 70 per cent of the respondents knew that babies with diarrhoea should be breastfed (Table VI).
More than half of the respondents reported after the campaign that they purified their water by boiling and filtering it, but only a few used chlorination and alum. Most people reported using homemade solutions for diarrhoea prevention and care (like salt and sugar solutions, daal-paani, etc.). Although 44 per cent reported using ORS for diarrhoea post-campaign, only a few reported following the suitable practice to prepare ORS, even after the campaign. The effect of the campaign on enhancing awareness and practices relating to waterborne diseases was most pronounced in Vaishali, compared to Pratapgarh and Kanpur-Dehat (data not shown).
Determinants of awareness and practices in the pre- and post-campaign periods: While the average scores of awareness and reported practice were higher after the campaign (Table III), those scores were still quite low. We, therefore, analysed other factors that could influence people's scores. The overall average awareness and practices scores (combined average scores of airborne, vector-borne and waterborne diseases - Table III) for the OLS regressions were used as dependent variable, and regression was performed both for the pooled data (Table VII) and for the three locations separately (data not shown). Several explanatory variables were considered, e.g. household characteristics, households experiencing diseases, head-of-household characteristics, access to health services, SHG member characteristics and locational characteristics. It was also tested whether awareness led to reported practice, by considering the average awareness score as an explanatory variable for the determinants of reported practice.
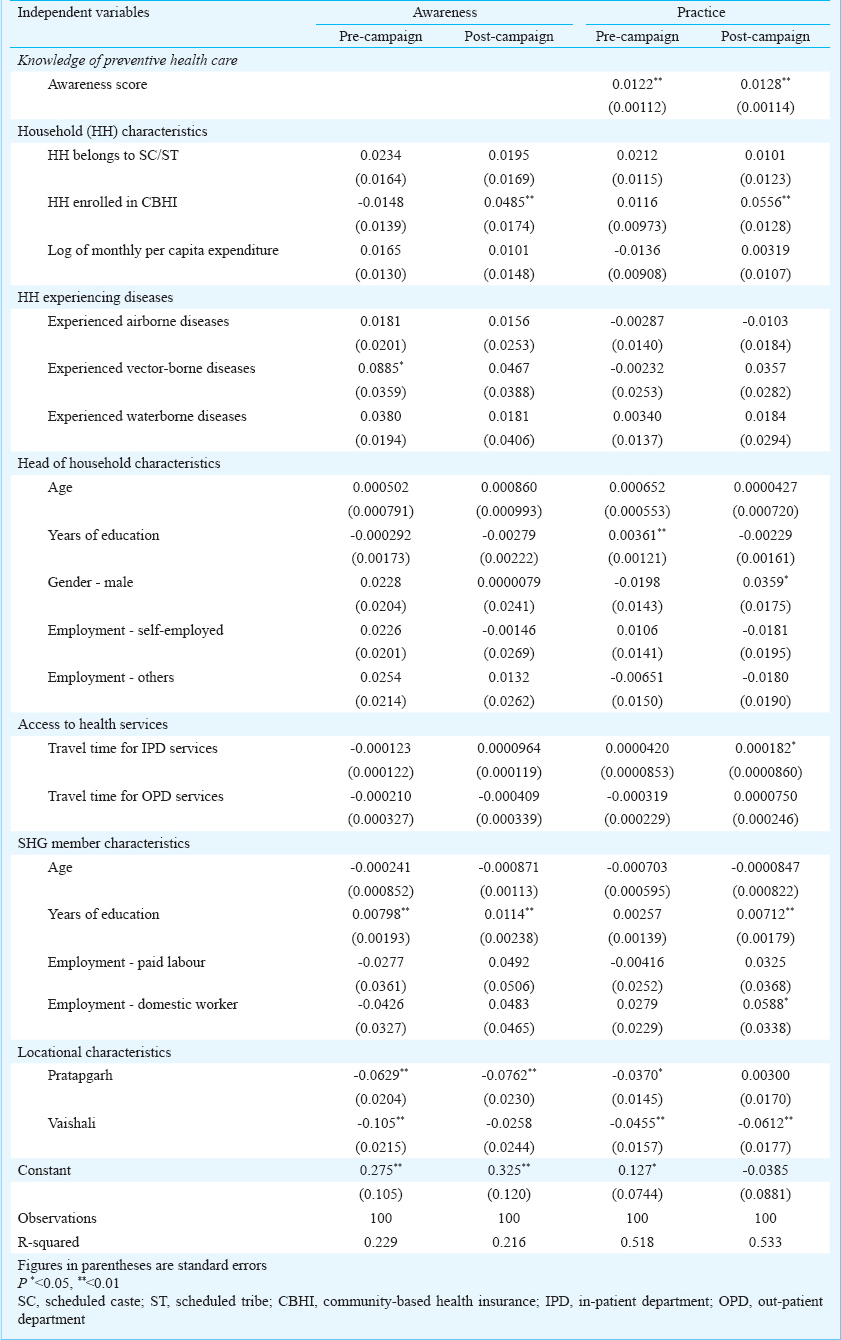
Determinants of preventive care awareness: Before the campaign, awareness was positively associated with prior exposure of the households to vector-borne and waterborne diseases (Table VII). The education of the SHG member was significantly and positively linked with awareness (but the education of the household head and the monthly per-capita expenditure (log of MPCE) were not significant explanatory variables). Residents of Pratapgarh and Vaishali had lower awareness than residents of Kanpur-Dehat.
After the campaign, affiliation to CBHI increased the probability of higher awareness (P<0.01). Similar to the pre-campaign results, education levels of SHG membership were positively associated with awareness. Households in Pratapgarh demonstrated lower effect of the campaign as scores did not change very much compared to Kanpur-Dehat, and for Vaishali the dummy turned out to be insignificant.
The comparison across locations showed that before the campaign, households in Kanpur-Dehat were aware to airborne, vector-borne or waterborne diseases in cases they reported prior exposure to these conditions (data not shown). In Vaishali, the average awareness score was negatively associated with travel time for inpatient care (IPD). And, in all three locations, the education of SHG members was a positive and significant determinant of awareness.
In post-campaign results, enrollment in CBHI and income (proxy used was per capita monthly expenditure (log of monthly per capita expenditure) were positively associated with awareness in Kanpur Dehat. In addition, in Kanpur-Dehat and in Pratapgarh, awareness was also positively associated with prior exposure to airborne diseases. Travel time to outpatient care (OPD) was negatively associated with awareness in Kanpur-Dehat.
Determinants of reported preventive care practices: In the pre-campaign phase, reported preventive care practices were positively and significantly determined by awareness (P<0.01) (Table VII). Scheduled caste/scheduled tribe households were more likely to practice preventive health as compared with household from higher castes. Education of both head of households (P<0.01) and the SHG member (P<0.1) were positive and significant determinants of reported practices. Households in Kanpur-Dehat were more likely to report preventive practices, compared to households in Pratapgarh and Vaishali.
After the campaign, practice scores continued to be positively and significantly associated with awareness scores (P<0.01). Affiliation to CBHI had a positive effect on practice scores (P<0.01). Male-headed households were more likely to report preventive health practices than female-headed households (P<0.05). An increase in average travel time to IPD services was associated with an increase in the reported practice scores (P<0.05). As in the pre-campaign phase, educational level of the SHG members was positively associated with practice scores (P<0.01). SHG members that were domestic workers had higher practice scores than non-working members (P<0.1). Households in Vaishali were less likely to practice preventive health compared to households in Kanpur-Dehat.
The average awareness scores were the most consistent explanatory variable for the practice scores in all locations, both before and after the campaign. CBHI-enrolled households were more likely to obtain higher practice scores in Pratapgarh before and after the campaign, while in Vaishali such positive relationship was observed only after the campaign (data not shown). The education of SHG member had a significant and positive effect on practice scores in Pratapgarh and Vaishali after the campaign.
Discussion
This study was carried out to establish the evidence on three research questions:First, was the campaign to enhance people's awareness to the risks of airborne, vector-borne and waterborne diseases effective? Secondly, were the campaigns also effective in inculcating preventive practices? Thirdly, is it possible to identify and confirm the associations between key demographic and socio-economic factors and awareness and/or preventive practices?
The findings offered a clear response to the first research question: the average awareness score was 14-58 per cent higher after the campaign, an improvement in people's awareness to the risks of airborne, vector-borne and waterborne diseases. The findings on the second question were equally compelling: the post-campaign average practice score was higher by 30-65 per cent compared to pre-campaign score showing that the campaign improved reported preventive practices. But the campaign was not equally effective everywhere: it was more effective in Vaishali than in Pratapgarh and Kanpur-Dehat.
The score improvements differed for the three types of diseases studied. For airborne diseases, the increase in average practice score was 40 per cent, but these results were better in Kanpur-Dehat and Vaishali, lesser in Pratapgarh. Awareness about tuberculosis increased significantly, but remained low; our findings corroborated those reported in other studies2324. For vector-borne diseases, the increase in awareness (46%) and practice (50%) was similar, but the absolute scores remained low, and the average practice score was lower than the one for awareness, even after the campaign. Other studies from developing countries suggested that the adoption of practices followed exposure to health incidence, even among people who were aware to the risks2425. As for waterborne diseases, average awareness and practice scores increased by 37 and 40 per cent respectively after the campaign. The average scores increased in Vaishali more than in Pratapgarh and Kanpur-Dehat. The responses on the practice of using ORS were very low, confirming similar findings in India reported by others26, even though awareness scores increased, especially in Vaishali. The post-campaign score on awareness about worm infection increased significantly, corroborating similar findings from China27.
The disease specific analysis suggested that the campaign was effective in raising awareness about airborne and waterborne diseases (an improvement of almost 50% in post-campaign score) and less so about vector-borne diseases (an improvement of about 33% in post-campaign score). Preventive practice scores were generally lower (between 28 and 35%); Kanpur-Dehat respondents stood out as more aware and more engaged in preventive measures; and Vaishali respondents stood out for their impressive improvement post-campaign, both in better awareness and in higher practices.
It was shown that education of women SHG members was a significant determinant of better awareness (confirming similar findings by others2428, which was assumed to facilitate adoption of preventive practices29. Affiliation to CBHI was one of the consistent determinants for higher awareness and practice scores after the campaign. As enrollment was open to female SHG members, and the CBHI entails participatory practices, these might have provided a platform for regular interaction and dissemination of information on the diseases and prevention.
It was concluded that campaigns organized as part of implementation of CBHI schemes targeting women members of SHGs in three locations in rural India enhanced awareness to the risks of airborne, vector-borne and waterborne diseases. The campaigns were effective in encouraging application of preventive practices (based on self-reported preventive practices), indicating that better awareness to the risks was a necessary first step to adoption of preventive practices. This also suggests that repeating the campaigns may lead to better adoption of preventive practices. The second important conclusion is that the CBHI schemes can serve as a platform to impart better awareness. This conclusion was based on the finding that better awareness and better practice were associated with membership in CBHI. Moreover, the CBHI activities provided the opportunity for regular gatherings and knowledge exchanges between the members. Thirdly, considering that the implementation of CBHI schemes was based on targeting women members of SHGs, the potential of success in achieving greater awareness to preventive care and subsequent adoption of suitable practices might be enhanced by organizing similar awareness campaigns through such groups on a wide scale.
Our study had certain limitations. Though almost similar results were observed in all three study locations, such a small study would not justify making generalizations that awareness campaigns led to improved preventive practices everywhere. Secondly, although our results were based on random samples of respondents drawn over two points in time, we did not assert a general pattern of cause-and-effect everywhere. Thirdly, due to the absence of a control group, it was not possible to conclude that the enhanced awareness and reported practice scores were solely due to the campaign. However, the fact that key socio-economic and demographic indicators, health incidence rates and access to health care facilities were similar in the pre- and post-campaign periods, the observed changes in awareness and reported practices might largely be attributed to the awareness campaigns. Fourthly, the information on preventive practices was sourced from self-reporting, so the habitual limitations of self-reporting must be considered. More research would be needed to confirm affirmatively the impact of better awareness on the adoption of preventive health practices, and in turn on the reduction of disease burden and the related healthcare costs.
Acknowledgment
The first (PP) and the last author (DMD) acknowledge funding provided by European Commission 7th Framework Programme; grant ID HEALTH-F2-2009-223518 – Community-based Health Insurance in India. The authors acknowledge substantive contribution of the Micro Insurance Academy and its staff in data collection and cleaning as well as in analytical inputs; and the implementing partners (BAIF, Shramik Bharti and Nidan) and the respondents, for their ongoing willingness to share information on the implementation. The authors thank Drs Nidhi Bhatt and Dinesh Baliga for their assistance in the development of awareness campaign materials and also for training.
Conflicts of Interest: None.
References
- World Health Organization: Country cooperation strategy at a glance: India 2012. Available from: http://www.who.int/countryfocus/cooperation_strategy/ccsbrief_ind_en.pdf?ua=1
- [Google Scholar]
- Government of India. Report of the Working Group on Disease Burden for the 12th Five Year Plan. New Delhi: Planning Commission; 2011.
- [Google Scholar]
- Global Burden of Disease 2010. In: Global burden of disease 2010. 2013. Available from: http://www.cseindia.org/userfiles/global_burden_aaron.pdf
- [Google Scholar]
- Adult and child malaria mortality in India: a nationally representative mortality survery. Lancet. 2010;376:1768-74.
- [Google Scholar]
- Central Bureau of Health Intelligence (CBHI). National health profile of India 2012. New Delhi: CBHI, Directorate of Health Services, Government of India; 2013.
- [Google Scholar]
- A community-based health education programme for bio-environmental control of malaria through folk theatre (Kalajatha) in rural India. Malar J. 2006;5:123.
- [Google Scholar]
- Effect of hand hygiene on infectious disease risk in the community setting: a meta-analysis. Am J Public Health. 2008;98:1372-81.
- [Google Scholar]
- Impact of educational intervention concerning awareness and behaviors relating to avian influenza (H5N1) in a high-risk population in Vietnam. PloS One. 2011;6:e23711.
- [Google Scholar]
- Evaluation of an educational intervention on villagers’ knowledge, attitude and behaviour regarding transmission of Schistosoma japonicum in Sichuan province, China. Acta Trop. 2013;127:226-35.
- [Google Scholar]
- The impact of an IEC campaign on tuberculosis awareness and health seeking behaviour in Delhi, India. Int J Tuberc Lung Dis. 2005;9:1259-65.
- [Google Scholar]
- Knowledge, attitude and practice on malaria: a study in a tribal belt of Orissa state, India with reference to use of long lasting treated mosquito nets. Acta Trop. 2009;112:137-42.
- [Google Scholar]
- Preventing waterborne diseases: analysis of a community health worker program in rural Tamil Nadu, India. J Community Health. 2012;37:513-9.
- [Google Scholar]
- Retrospective study of chikungunya outbreak in urban areas of India. Indian J Med Res. 2012;135:351-8.
- [Google Scholar]
- Spatial access to inpatient health care in northern rural India. Geospatial Health. 2014;8:545-56.
- [Google Scholar]
- Census of India. Primary Census Abstract. 2011. Available from: http://www.censusindia.gov.in/pca/default.aspx
- [Google Scholar]
- Office of the Registrar General & Census Commissioner. Annual health survey 2010-11: Fact sheet, Bihar. 2012. Available from: http://www.censusindia.gov.in/vital_statistics/AHSBulletins/AHS_Baseline_Factsheets/Bihar.pdf
- [Google Scholar]
- Office of the Registrar General & Census Commissioner. Annual health survey 2010-11: Fact Sheet, Uttar Pradesh. 2012. Available from: http://www.censusindia.gov.in/vital_statistics/AHSBulletins/AHS_Baseline_Factsheets/U_P.pdf
- [Google Scholar]
- Sample Registration System. Vital rates: Figures at a glance, India 2012. 2012. New Delhi: Census of India; Available from: http://www.censusindia.gov.in/2011-Common/Vital%20Rates.pdf
- [Google Scholar]
- Reconciling research and implementation in micro health insurance experiments in India: study protocol for a randomized controlled trial. Trials. 2011;12:224.
- [Google Scholar]
- Micro-insurance: extending health insurance to the excluded. Int Soc Secur Rev. 1999;52:71-97.
- [Google Scholar]
- Understanding attitudes and predicting social behaviour. New Jersey, USA: Prentice-Hall; 1980.
- [Google Scholar]
- Prevalence of self-reported tuberculosis, knowledge about tuberculosis transmission and its determinants among adults in India: results from a nation-wide cross-sectional household survey. BMC Infect Dis. 2013;13:16.
- [Google Scholar]
- Knowledge about tuberculosis transmission among ever-married women in Bangladesh. Int J Tuberc Lung Dis. 2011;15:379-84.
- [Google Scholar]
- Caregivers's knowledge, attitude and practice on childhood malaria and treatment in urban and rural communities in Enugu, south-east Nigeria. Public Health. 2005;119:409-14.
- [Google Scholar]
- Performance of a community-based health and nutrition-education intervention in the management of diarrhoea in a slum of Delhi, India. J Health Popul Nutr. 2010;28:553-9.
- [Google Scholar]
- Health-education package to prevent worm infections in Chinese schoolchildren. N Engl J Med. 2013;368:1603-12.
- [Google Scholar]
- Awareness of dengue and practice of dengue control among the semi-urban community: a cross sectional survey. J Community Health. 2011;36:1044-9.
- [Google Scholar]
- Diarrhea prevention through household-level water disinfection and safe storage in Zambia. Am J Trop Med Hyg. 2002;66:584-9.
- [Google Scholar]






