Translate this page into:
Methicillin resistant Staphylococcus aureus (MRSA) in India: Prevalence & susceptibility pattern
Reprint requests: Dr Sangeeta Joshi, Department of Microbiology, Manipal Hospital, 98 Rustom Bagh, Old Airport Road, Bangalore 560 017, India e-mail: sangeetajo@yahoo.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Methicillin resistant Staphylococcus aureus (MRSA) is endemic in India and is a dangerous pathogen for hospital acquired infections. This study was conducted in 15 Indian tertiary care centres during a two year period from January 2008 to December 2009 to determine the prevalence of MRSA and susceptibility pattern of S. aureus isolates in India.
Methods:
All S. aureus isolates obtained during the study period in the participating centres were included in the study. Each centre compiled their data in a predefined template which included data of the antimicrobial susceptibility pattern, location of the patient and specimen type. The data in the submitted templates were collated and analysed.
Results:
A total of 26310 isolates were included in the study. The overall prevalence of methicillin resistance during the study period was 41 per cent. Isolation rates for MRSA from outpatients, ward inpatients and ICU were 28, 42 and 43 per cent, respectively in 2008 and 27, 49 and 47 per cent, respectively in 2009. The majority of S. aureus isolates was obtained from patients with skin and soft tissue infections followed by those suffering from blood stream infections and respiratory infections. Susceptibility to ciprofloxacin was low in both MSSA (53%) and MRSA (21%). MSSA isolates showed a higher susceptibility to gentamicin, co-trimoxazole, erythromycin and clindamycin as compared to MRSA isolates. No isolate was found resistant to vancomycin or linezolid.
Interpretation & conclusions:
The study showed a high level of MRSA in our country. There is a need to study epidemiology of such infections. Robust antimicrobial stewardship and strengthened infection control measures are required to prevent spread and reduce emergence of resistance.
Keywords
Antimicrobial susceptibility
India
MRSA
prevalence
Staphylococcus
Staphylococcus aureus continues to be a dangerous pathogen for both community-acquired as well as hospital-associated infections. S. aureus resistant to methicillin were reported soon after its introduction in October 19601. Methicillin resistant S. aureus (MRSA) is now endemic in India. The incidence of MRSA varies from 25 per cent in western part of India2 to 50 per cent in South India3. Community acquired MRSA (CA-MRSA) has been increasingly reported from India4.
A network of microbiology laboratories (Indian Network for Surveillance of Antimicrobial Resistance - INSAR) at premier medical colleges and hospitals in India was formed with support from the World Health Organization (Figure). The network aims to monitor antimicrobial resistance and to review the magnitude of its problem in India. Initially, a few organisms of public health importance have been chosen for monitoring their prevalence and antimicrobial resistance patterns, with S. aureus being chosen among the Gram-positive organisms. All participating laboratories shared their antimicrobial susceptibility data and provided technical support to other members. The present study provides a national level initiative to understand emerging trends of antimicrobial resistance among clinical isolates of S. aureus and provides a platform to initiate epidemiological studies for staphylococcal infections.

- Places marked with red dots are INSAR members whose data one oncluded in teh study. Places marked *are INSAR members whose data are not included in the study.
Material & Methods
The present study was a two year (January 2008 to December 2009) retrospective study. Each centre provided their susceptibility data for S. aureus isolates for the study period in a defined template. The data were collated and analysed. The template included patient's location, source/specimen of the isolate and the antibiotic susceptibility profiles. The antibiotic susceptibility testing was performed at different study sites by the Kirby Bauer‘s’ disc diffusion technique5 and/or minimum inhibitory concentration (MIC) testing, using Clinical and Laboratory Standards Institute (CLSI) recommendations5. Cefoxitin (30 μg) and/or oxacillin (1 μg) were used for methicillin resistance.
The other antibiotics tested included penicillin (10 units), gentamicin (10 μg), co-trimoxazole (1.25/23.75 μg), ciprofloxacin (5 μg), erythromycin (15 μg), clindamycin (2 μg), vancomycin (30 μg) and linezolid (30 μg). Discs from Hi-media (Mumbai) and Oxoid (UK) were used by the participating laboratories. Inoculum was prepared by making a direct saline suspension of isolated colonies selected from an 18- to 24-h blood agar plate. Turbidity of the suspension was adjusted to achieve a turbidity equivalent to a 0.5 McFarland standard and five discs were applied on a 100mm Mueller Hinton agar plate as per CLSI guidelines. S. aureus ATCC 25923 was used as the quality control strain for disc diffusion.
Chi square test was used to compare antimicrobial susceptibility data.
Results
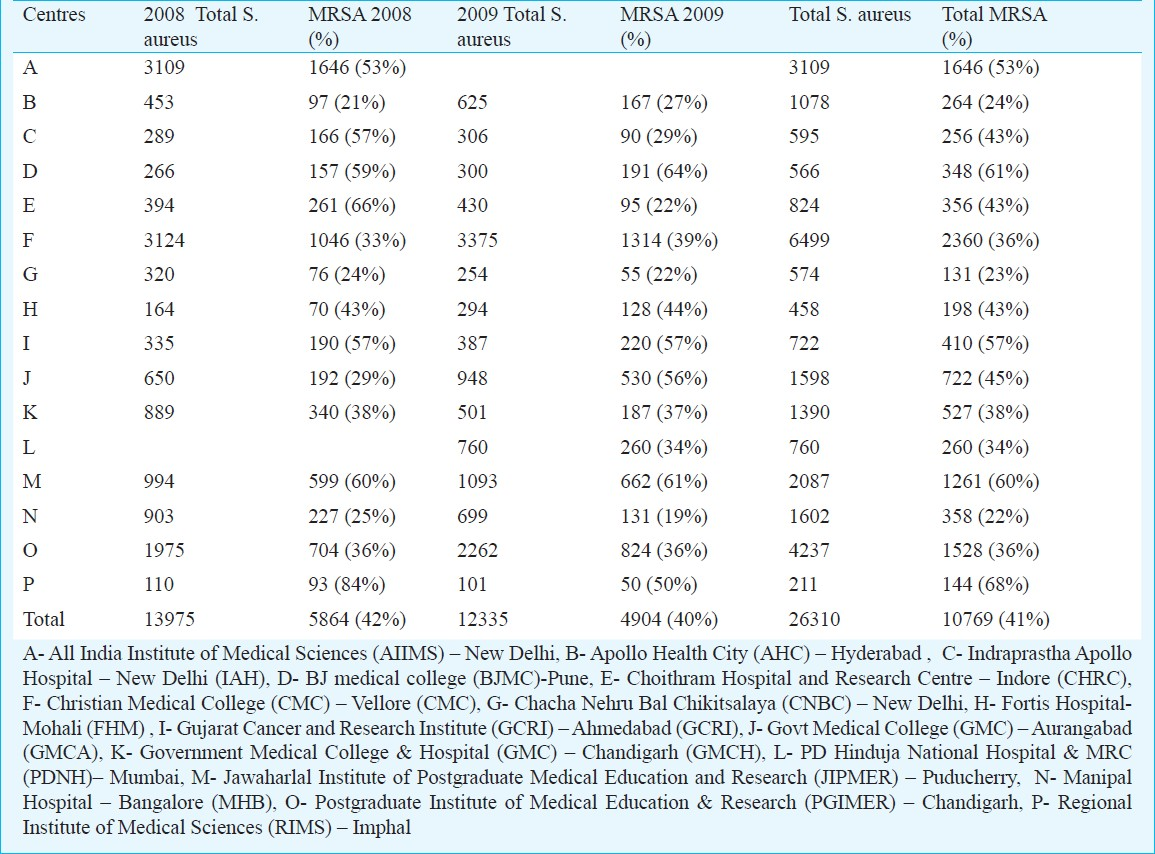
Of the 13975 isolates of S. aureus in 2008, 5864 (42%) were MRSA. In 2009, of the 12335 isolates, 5133 (40%) were MRSA. (Table I). Details of 5354 isolates in 2008 and 7088 isolates in 2009 were available (Table II). The majority of the isolates were obtained from inpatients - 3664 in 2008 and 4487 in 2009. The MRSA rates among outpatients, non-ICU inpatients and ICU patients were 28, 42 and 43 per cent, respectively in 2008 and 27, 49 and 47 per cent, respectively in 2009.
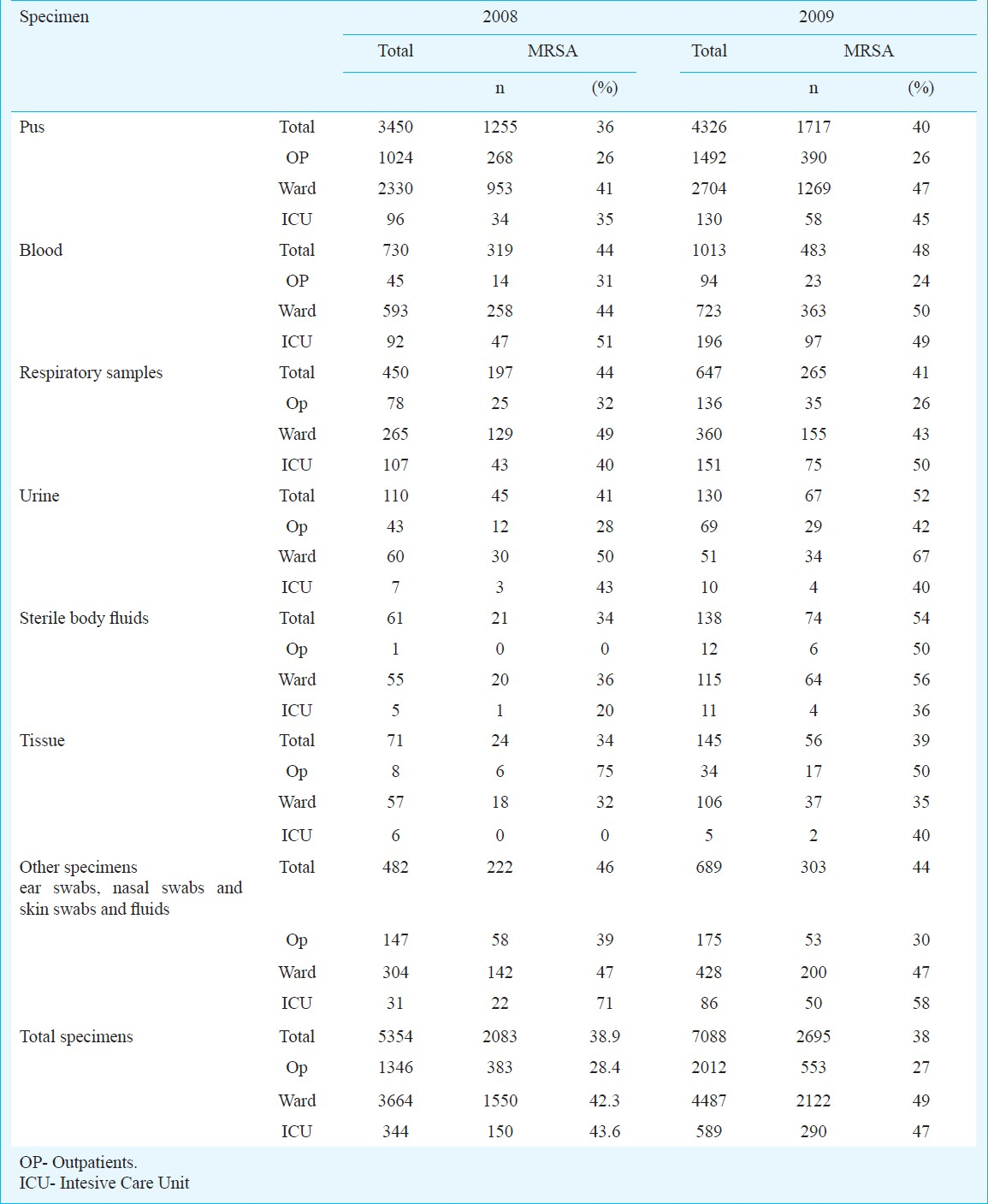
The details of the specimen were available for 12442 isolates. S. aureus was mainly isolated from skin and soft tissue infections (64% in 2008 and 61% in 2009) followed by blood and respiratory samples including bronchial washings, endotracheal secretions and sputum (Table II). Throat swab and genital specimens were received mainly from outpatients whereas S. aureus isolated from tissue, catheter tips and fluid from sterile body sites were predominantly from inpatients. Other specimens received included ear swabs, nasal swabs and skin swabs and fluids.
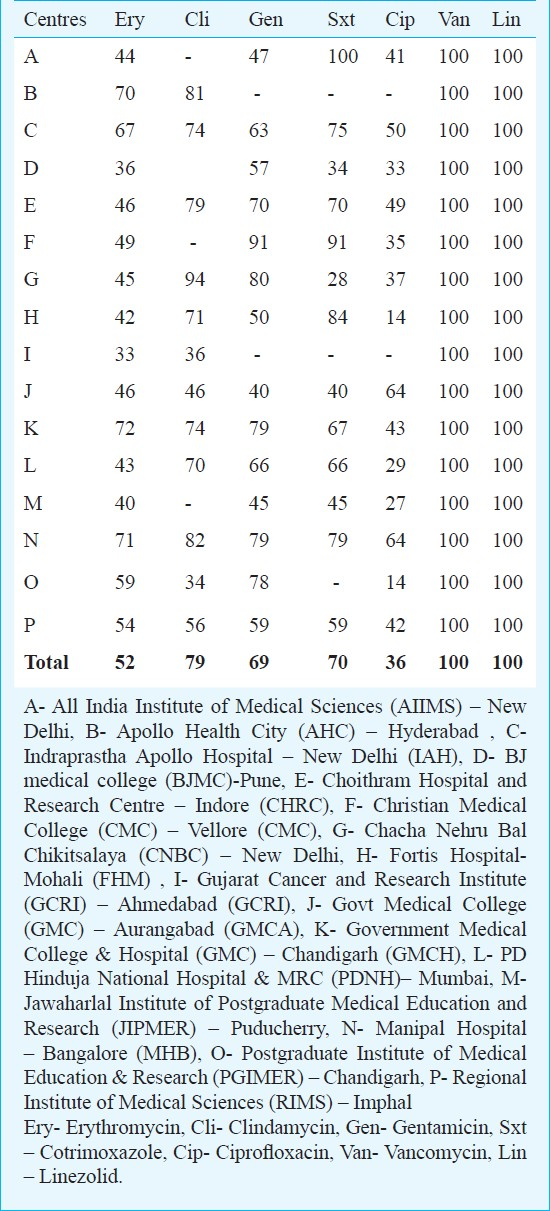
Antibiotic susceptibility testing data for erythromycin, clindamycin, co-trimoxazole, gentamicin, vancomycin and linezolid were compiled. There was no resistance documented against vancomycin and linezolid. Resistance to antibiotics amongst the MRSA isolates was more than that in methicillin sensitive S. aureus (MSSA) (P<0.001) (Table III). The susceptibility to other antibiotics from different centres was analysed. (Table IV). There was no uniform difference in the susceptibilities between centres of north, south and west India.

Discussion
Among the Gram-positive pathogens, S. aureus continues to cause skin and soft tissue infections (SSTI) in the community as well as invasive infections in the hospitalized patients. In a recent Europe-wide survey, the most common organisms in SSTIs were S. aureus (71% cases) with 22.5 per cent being MRSA6. The proportion of MRSA varied among countries ranging from 0.4 per cent in Sweden to 48.4 per cent in Belgium6. In a study in US7spanning over 10 years, there was an increase in the overall incidence of S. aureus during this period with an increase in community onset MRSA SSTI.
The overall MRSA prevalence in our study was 42 per cent in 2008 and 40 per cent in 2009. The prevalence of MRSA in a study from Chennai3 was reported as 40-50 per cent. S. aureus constituted 17 per cent of catheter related blood stream infections (CRBSIs) in that centre. A high prevalence of MRSA (35% in ward and 43% in ICU) was observed from blood culture specimens in a study in Delhi8. In the present study, MRSA isolation rates from ICU and wards were higher than that seen among outpatients. Patel et al2 reported a change in the blood stream infections with S. aureus emerging as the predominant pathogen in recent years.
Around 60 per cent of the S. aureus isolates in our study were from SSTI. The prevalence of MRSA varies between regions and between hospitals in the same region as seen in a study from Delhi9 where the MRSA prevalence in nosocomial SSTI varied from 7.5 to 41.3 per cent between three tertiary care teaching hospitals. In our study, the MRSA isolation varied between different hospitals. The participating centres included teaching hospitals, tertiary care private hospitals and a children's hospital. The patient profile varied between these centres and may account for the different MRSA isolation rates. Verghese et al10 reported Gram-negatives being predominantly isolated from their samples. S. aureus accounted for less than 25 per cent of SSTI among their patients and the overall MRSA rate was 35 per cent10.
CA-MRSA isolates are now being increasingly reported from India. D’ Souza et al4 studied 412 confirmed cases of MRSA and found that 54 per cent were true CA-MRSA possessing the SCCmec IV and SCC mec V genes. These were mainly isolated from SSTIs. CA-MRSA isolates also showed variable resistance to ciprofloxacin, erythromycin, clindamycin and tetracycline. Chatterjee et al11 found the overall prevalence of S. aureus nasal colonization was 52.3 per cent and that of MRSA was 3.89 per cent in the community.
In a study from north India12, the prevalence of MRSA was 46 per cent and MRSA isolates were found to be more resistant to other antibiotics than MSSA. Significant difference was observed in case of erythromycin, ciprofloxacin, gentamicin and amikacin.
Vancomycin is considered inferior to β-lactams for the treatment of MSSA bacteraemia and endocarditis13. Therefore, the first-generation cephalosporins are the drugs of choice for the treatment of MSSA infections in patients who are unable to tolerate antistaphylococcal penicillins. De-escalation of vancomycin to β-lactams should be encouraged in all cases of MSSA. With MRSA isolates being widespread, it is imperative that treating physicians de-escalate to β-lactams once the culture sensitivity results reveal a MSSA isolate. Preservation of glycopeptides and linezolid for use only in MRSA cases should be encouraged.
Our study had the following limitations. Firstly, the data obtained from all the centres were not uniform with respect to the antibiotics tested. Hence an accurate determination of multidrug resistance in all the MRSA isolates could not be done. Secondly, molecular studies have not been done for these isolates to differentiate between CA-MRSA and healthcare associated MRSA (HA-MRSA).
In conclusion, this study demonstrates that MRSA is a problem in India. More number of MRSA isolates were multidrug resistant as compared with the MSSA isolates. Glycopeptides and linezolid continue to remain the mainstay for treatment for MRSA infections.
Acknowledgment
This work and the INSAR group is supported by the World Health Organization. Authors acknowledge the help of Drs Sujatha Sistla, Sheetal Chitnis, Benu Dhawan, Vaishali Dohe and Shri Kareem for their help in data acquisition.
References
- Time trends in the epidemiology of microbial infections at a tertiary care center in west India over last 5 years. J Assoc Physicians India. 2010;58(Suppl):37-40.
- [Google Scholar]
- Changing trends in antimicrobial susceptibility and hospital acquired infections over an 8 year period in a tertiary care hospital in relation to introduction of an infection control programme. J Assoc Physicians India. 2010;58(Suppl):25-31.
- [Google Scholar]
- Molecular characterization of Methicillin-resistant Staphylococcus aureus with emergence of epidemic clones of sequence type (ST)22 and ST 772 in Mumbai, India. J Clin Microbiol. 2010;48:1806-11.
- [Google Scholar]
- Clinical and Laboratory Standards Institute (2008) Performance standards for antimicrobial susceptibility testing. In: Eighteenth Informational supplement. CLSI document M100-S18. Wayne PA: Clinical and Laboratory Standards Institute;
- [Google Scholar]
- Antimicrobial susceptibility of Gram-positive cocci isolated from skin and skin-structure infections in European medical centres. Int J Antimicrob Agents. 2010;36:28-32.
- [Google Scholar]
- Staphylococcus aureus infections in US veterans, Maryland, USA, 1999-2008. Emerg Infect Dis. 2011;17:441-8.
- [Google Scholar]
- Surveillance of multidrug resistant organisms in tertiary care hospital in Delhi, India. J Assoc Physicians India. 2010;58(Suppl):32-6.
- [Google Scholar]
- Clinical and molecular characteristics of nosocomial methicillin-resistant Staphylococcus aureus skin and soft tissue isolates from three Indian hospitals. J Hosp Infect. 2009;73:253-63.
- [Google Scholar]
- Bacterial organisms and antimicrobial resistance patterns. J Assoc Physicians India. 2010;58(Suppl):23-4.
- [Google Scholar]
- A community based study on nasal carriage of Staphylococcus aureus. Indian J Med Res. 2009;130:742-8.
- [Google Scholar]
- Prevalence of Methicillin- resistant Staphylococcus aureus (MRSA) in a tertiary care hospital in northern India. J Lab Physicians. 2010;2:78-81.
- [Google Scholar]
- Clinical practice guidelines by the infectious disease society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adult and children. Clin Infect Dis. 2011;52:e18-e55.
- [Google Scholar]






