Translate this page into:
Medication adherence patterns in aortic dissection survivors
For correspondence: Dr. Ashish Chaddha, Frankel Cardiovascular Center, University of Michigan, Michigan Cardiovascular Outcomes Research & Reporting Program, Domino's Farms, 24 Frank Lloyd Wright Drive, Lobby A/3201, Ann Arbor, MI 48106-0384, USA e-mail: Ashish.Chaddha@beaumont.org
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Beta-blockers have been shown to improve survival in both type A and type B acute aortic dissection (AAD) patients. Calcium channel blockers have been shown to selectively improve survival only in type B AAD patients. There is a lack of data on medication adherence in AAD survivors. The purpose of this study was to assess medication adherence in patients who survived an AAD.
Methods:
This was a cross-sectional survey-based study of individuals from a single medical centre which was part of the larger International Registry of Acute Aortic Dissection (IRAD). Patients with type A or B AAD who survived to discharge were included in this study. Individuals who were deceased based on the results of an online Social Security Death Index were excluded from the study. Data were obtained from both a survey and also from abstraction from the local academic institution's IRAD registry. A survey packet was sent to patients. One section of this survey was dedicated to assessing medication adherence using the 4-item Morisky scale.
Results:
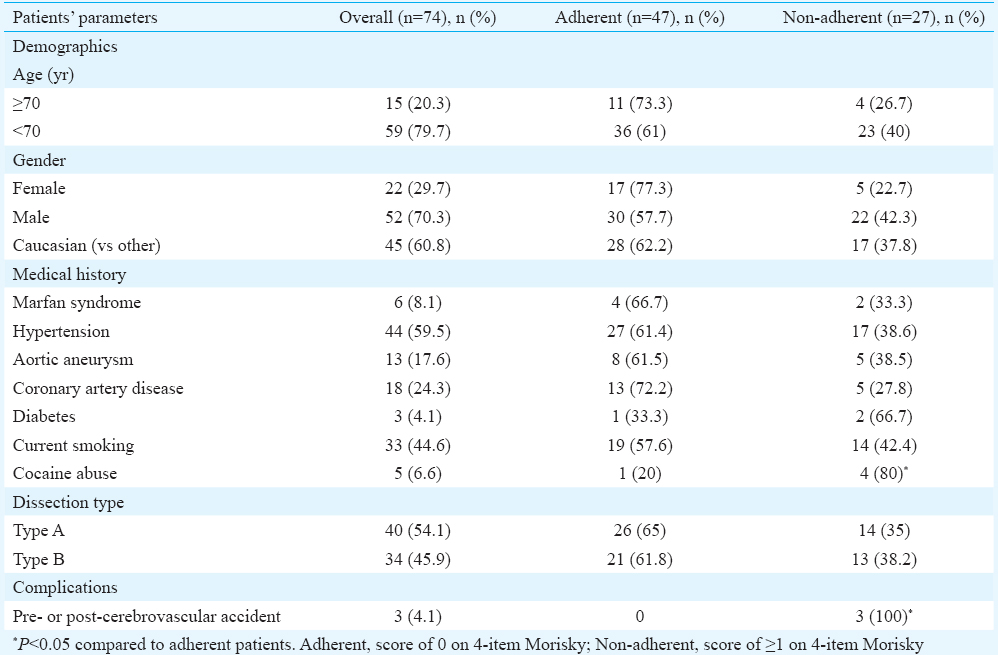
Eighty two completed surveys were returned; 74 patients completed the section of the survey pertaining to medication adherence (response rate 38%). Morisky score was ≥1.0 for 27 (36%) patients and 0 for 47 (64%) patients. Thirty three patients reported yes to ‘forget to take medications’ and eight reported yes to ‘careless with medications.’ Medication non-adherence (defined as a score of ≥1.0 on Morisky) was associated with increased follow up recurrence of chest pain at one year of follow up. Only two patients stopped their antihypertensive on their own and did not cite a reason for doing this.
Interpretation & conclusions:
The medication adherence rate for patients who survived an AAD was 64 per cent at a median (Q1, Q3) of 7.1 yr (5.6, 11.5) after discharge, as per the Morisky scale. The clinicians should educate their patients on the importance of antihypertensive therapy and assess for forgetfulness and carelessness at each clinic visit, as well as understand patients’ beliefs about drug therapy, all of which have been shown to increase medication adherence.
Keywords
Angiotensin-converting enzyme inhibitors
antihypertensive
aorta
aortic disease
aortic dissection
beta-blockers
blood pressure
calcium-channel blockers
An aortic dissection involves a tear in the intima creating a false lumen. Blood can enter this false lumen, the intima-media space, leading to further propagation of the dissection. Most often the aorta is already weakened due to degenerative changes from ageing, atherosclerosis, hypertension and genetic conditions. Although an aortic dissection is a life-threatening emergency, the one and three years survival rates in type A and type B aortic dissection, managed medically, surgically or with endovascular therapy, are quite high. However, it is important to note that three years survival rates are higher in type A aortic dissection survivors (about 90%) compared to type B aortic dissection survivors (about 75%)12. Survival rates can likely be further improved by focusing on and increasing medication adherence in aortic dissection survivors.
Blood pressure and heart rate control is felt to be an important medical intervention in the follow up management of aortic dissection. Beta-blockers appear to improve survival in patients with type A aortic dissection undergoing surgery [odds ratio (OR)=0.47]3. Calcium channel blockers may improve survival selectively for patients with type B aortic dissection treated medically (OR=0.55)3. Antihypertensives are felt to reduce aortic wall stress, which may decrease further expansion of the false lumen and/or prevent dissection extension and/or aortic rupture.
As with all medications used to treat chronic conditions, medication adherence remains an issue. Evidence suggests that medication non-adherence is associated with adverse outcomes4. No studies exist assessing the medication adherence rate in aortic dissection survivors. For other chronic illnesses, such as hypertension, only 31 per cent of patients have adequately controlled blood pressure5, with a major reason being non-adherence to antihypertensives67. The medication non-adherence rate for patients with hypertension has been estimated to be as high as 50 per cent8. A better understanding of medication adherence and reasons for non-adherence provide the potential opportunity to improve clinical outcomes9101112. Thus, the purpose of this study was to assess medication adherence patterns in aortic dissection survivors.
Material & Methods
This was an observational study consisting of a cross-sectional survey of individuals who received care at the University of Michigan hospital in Ann Arbor, Michigan, USA, which is a part of the International Registry of Acute Aortic Dissection (IRAD) registry, from 1996 to 2011.
The sample of patients used for this study was derived from the IRAD, a multinational registry consisting of 34 referral centres in 12 countries. It contains 4430 patients enrolled in the registry since it began in 1996. Full details regarding IRAD have been previously published1314.
Patients for this study were from a single academic medical centre which is a part of the IRAD registry. The patients in our study included those who have survived a type A or type B acute aortic dissection (AAD). Type A AAD is defined as any non-traumatic dissection involving the ascending aorta and presenting within 14 days of symptom onset. Type B AAD is defined as any non-traumatic dissection involving the descending aorta and presenting within 14 days of symptom onset1314. All patients received medical treatment, and when indicated, surgery and/or endovascular treatments.
All individuals who survived to discharge were considered for the study (n=439). Patients were excluded if their mailing address on file was incorrect or if they were deceased based on an online search of the Social Security Death Index (n=125, mean age 71.40±12.88 yr).
Data for this study were obtained from both a survey and analyses of data contained in the IRAD registry after Institutional Review Board approval. A survey was mailed to 197 patients (as the address for only these 197 patients was available). Informed written consent was obtained from all participants. While this survey was part of a larger study to better understand physical and emotional well-being in AAD survivors, one section was dedicated to medication adherence. If there was no response from the patient two weeks after initial mailing of the survey, a second survey packet was sent. Eighty two surveys were returned as completed. Of these 82 responders, 74 completed the portion of the survey pertaining to medication adherence. Thus, the overall response rate was 38 per cent. The time (median) between discharge and completion of survey was 7.1 yr.
Data regarding the initial presentation, including dissection-related presenting symptoms (i.e. chest pain, back pain, dizziness), physical examination findings, demographics, management (medical, surgical, and/or endovascular), imaging modality and findings (i.e. extent of dissection, aortic diameters) and in-hospital complications, had already been entered into the local IRAD database through medical record abstraction. Follow up data after one and six months after discharge, and annually until five years after discharge, consisting of the blood pressure at clinic visits, presence of dissection-related symptoms (yes/no response for each specific symptom), physical examination findings at the visit, cardiac medications, imaging findings and any pre-operative, post-operative and interval complications (cardiovascular accident, coma, malperfusion, limb ischaemia, myocardial ischaemia/infarction, mesenteric ischaemia, hypotension, shock, tamponade and intramural haematoma), had also been previously entered into the local IRAD database by medical record abstraction. The forms used for entering this initial presentation and follow up data were reviewed for internal and external validity.
Our survey utilized a 4-item self-reported scale developed by Morisky to assess medication adherence1516. The Morisky scale is a validated, self-reporting tool commonly used for medication adherence screening. It consists of four items (forgetfulness, carelessness, side effects and feeling better) to assess adherence using a yes/no response format. The scale score is derived from the sum of responses, with ‘yes’ equalling 1 point and ‘no’ equalling 0 points; a score of 0 indicates higher adherence. Individuals were asked to think about their blood pressure lowering medications as a whole over the past 12 wk when answering these questions.
Statistical analysis: SPSS statistical software (SPSS Inc., Chicago, IL, USA) was used for data analysis. Descriptive data are presented as means for continuous variables and frequencies for categorical variables. Frequencies were determined for each item of the Morisky scale. Pearson's Chi-square and Fisher's exact test were used to determine the association between demographic variables (i.e. gender, race, type of dissection, etc.) and medication non-adherence. A Kaplan–Meier analysis was performed to examine the association between recurrent follow up dissection-related symptoms and/or pain and medication non-adherence.
Results
The majority of patients were <70 yr of age, male, and Caucasian. A large proportion of patients had a history of hypertension as well as smoking (Table). There was an equal distribution of type A and type B aortic dissections. The Morisky score was ≥1.0 for the overall antihypertensive regimen for 27 (36%) patients, indicating a level of non-adherence. Forty eight (64%) patients reported a Morisky score of 0 suggesting medication adherence. Medication adherence for patients who have survived an aortic dissection was 64 per cent at a median (Q1, Q3) of 7.1 yr (5.6, 11.5) after discharge. The Figure presents an analysis of the scores for each Morisky item for all four antihypertensive classes (beta blockers, angiotensin receptor inhibitors, Angiotensin converting enzyme inhibitors, calcium channel blockers) combined. The Morisky item with the highest number of patients responding with a yes, indicating poor adherence, was forgetfulness followed by carelessness.
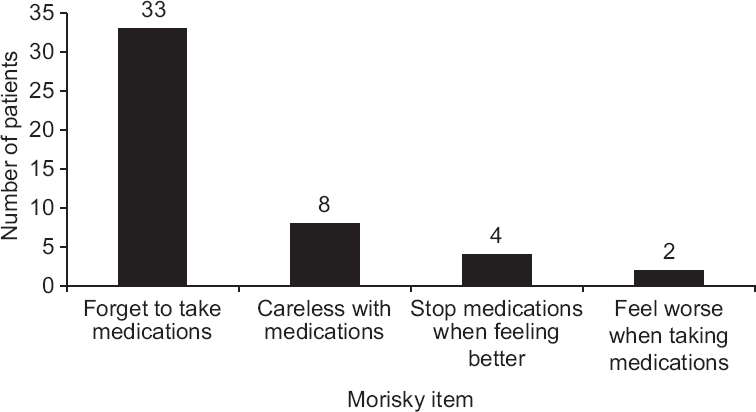
- Number of patients responding ‘yes’ to each item on the Morisky scale.
Sixteen patients responded ‘yes’ to having an anti-hypertensive discontinued (six for beta-blocker, and five for calcium channel blocker). Of these 16 patients, 14 reported that the medication was discontinued by their physician as it was no longer needed, while two patients discontinued the medication on their own and did not give a particular reason for doing so.
Forty five per cent of patients (n=33) who reported non-adherence as per the Morisky scale had chest pain (similar pain as initial presentation but milder without recurrence of aortic dissection) within one year of follow up, while patients who reported adherence did not have chest pain within one year of follow up (P=0.007).
Discussion
The goal of treatment after an AAD is to prevent further propagation of the false lumen, aortic expansion, dissection extension, and aortic rupture. Antihypertensives, particularly beta-blockers, by reducing aortic wall stress, are thought to decrease the risk of these complications313.
The medication adherence rate for patients who have survived an AAD was 64 per cent at a median (Q1, Q3) of 7.1 yr (5.6, 11.5) after discharge, as per the Morisky scale. This adherence rate was similar to the reported medication adherence rate for patients with heart failure (65%)17, and was higher than the medication adherence rate for patients with hypertension (40-50%)18 and patients with a history of acute coronary syndromes (46.2%)19. Only two patients discontinued an antihypertensive on their own, with others having the medication discontinued by their physician as it was no longer indicated.
Items on the Morisky scale which were most frequently answered as ‘yes’ were intentional forgetfulness and carelessness. While the Morisky scale is a measure for adherence and not for a reason for non-adherence, forgetfulness and carelessness have been shown to be the two main reasons for non-adherence in patients with a history of acute coronary syndromes and in patients with hypertension1920. Non-adherent patients were more likely to have chest pain at one year of follow up. This suggests the importance of medication adherence in decreasing long-term adverse events and improving clinical outcomes, which has been previously shown101112. While these findings were striking, these were limited in their interpretation given this survey was sent to patients at an average of seven years after discharge. It is possible that symptoms within one year of discharge were due to poor compliance with medical therapy and clinic follow up, which has translated to lower medication adherence at this time of survey completion. Further study is needed to better understand this association.
This study suggests relatively high medication adherence rates for aortic dissection patients, higher than several other chronic cardiac conditions171819. However, there still remains substantial room for improvement. Clinicians, pharmacists, and other health professionals must continue to educate patients about the importance of antihypertensives in likely reducing aortic wall stress, thus decreasing the risk of future aortic complications. Patient education has been shown to improve outcomes by allowing patients to take part in the management of their chronic illness21. Other possible methods to improve adherence include an understanding of patients’ beliefs about drug therapy by clinicians, which has also been shown to improve adherence22. Modern technology such as websites and mobile applications may be promising for educating patients and improving adherence. Consistent phone calls to patients between follow up clinic visits may also be beneficial. Reasons for non-adherence and interventions for adherence improvement are topics for future study.
The major limitation of this study was recall bias. Due to this, the adherence rate may be lower than that reported in our study. It was possible that non-responders were either doing so well as to not respond, careless or forgetful with their medications as well as in completing this survey and returning it to us or are extremely debilitated and not able to respond or deceased since the time of mailing the survey. It could be that only healthy controls responded to our survey. Finally, adherence was assessed using a self-reported scale rather than a more objective measure, raising the possibility of over-reporting of adherence. Also, patients who were not involved in their own medication management might have erroneously filled out our survey, which would also lower our adherence rate. Future studies may consider utilizing a more objective measure of medication compliance, such as blood pressure. It was also not known what percentage of patients who were ‘non-adherent’ as per the Morisky scale were non-adherent with multiple prescribed antihypertensives as compared to only one prescribed antihypertensive. It was also not known what percentage of patients was overusing their medications, which is also a form of non-adherence.
In conclusion, the medication adherence rate for patients who survived an AAD was 64 per cent at a median (Q1, Q3) of 7.1 yr (5.6, 11.5) after discharge, as per the Morisky scale. This rate was comparable to that of patients with other chronic cardiovascular conditions such as acute coronary syndromes, hypertension and heart failure. Clinicians should continue to educate patients on the importance of antihypertensive therapy and assess for forgetfulness and carelessness at each visit, as well as understand patients’ beliefs about drug therapy, all of which have been shown to increase medication adherence.
Financial support & sponsorship: None
Conflicts of Interest: None.
References
- Long-term survival in patients presenting with type A acute aortic dissection: Insights from the International Registry of Acute Aortic Dissection (IRAD) Circulation. 2006;114(1 Suppl):I350-6.
- [Google Scholar]
- Long-term survival in patients presenting with type B acute aortic dissection: Insights from the International Registry of Acute Aortic Dissection. Circulation. 2006;114:2226-31.
- [Google Scholar]
- Type-selective benefits of medications in treatment of acute aortic dissection (from the International Registry of Acute Aortic Dissection [IRAD]) Am J Cardiol. 2012;109:122-7.
- [Google Scholar]
- Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA. 2003;290:199-206.
- [Google Scholar]
- Adherence with statin therapy in elderly patients with and without acute coronary syndromes. JAMA. 2002;288:462-7.
- [Google Scholar]
- Non-compliance and knowledge of prescribed medication in elderly patients with heart failure. Eur J Heart Fail. 1999;1:145-9.
- [Google Scholar]
- Helping patients follow prescribed treatment: Clinical applications. JAMA. 2002;288:2880-3.
- [Google Scholar]
- Patient adherence: The next frontier in quality improvement. Am J Med. 2004;117:130-2.
- [Google Scholar]
- Chronic beta-blocker therapy improves outcome and reduces treatment costs in chronic type B aortic dissection. Eur J Cardiothorac Surg. 2001;19:606-10.
- [Google Scholar]
- Tight heart rate control reduces secondary adverse events in patients with type B acute aortic dissection. Circulation. 2008;118(14 Suppl):S167-70.
- [Google Scholar]
- Aortic dissection: New frontiers in diagnosis and management: Part II: Therapeutic management and follow-up. Circulation. 2003;108:772-8.
- [Google Scholar]
- Acute type A aortic dissection in the elderly: Clinical characteristics, management, and outcomes in the current era. J Am Coll Cardiol. 2002;40:685-92.
- [Google Scholar]
- The International Registry of Acute Aortic Dissection (IRAD): New insights into an old disease. JAMA. 2000;283:897-903.
- [Google Scholar]
- Self-reported morisky score for identifying nonadherence with cardiovascular medications. Ann Pharmacother. 2004;38:1363-8.
- [Google Scholar]
- Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67-74.
- [Google Scholar]
- Compliance with and dosing of angiotensin-converting-enzyme inhibitors before and after hospitalization. Am J Health Syst Pharm. 2000;57:139-45.
- [Google Scholar]
- Discontinuation of and changes in treatment after start of new courses of antihypertensive drugs: A study of a United Kingdom population. BMJ. 1995;311:293-5.
- [Google Scholar]
- Adherence to medications by patients after acute coronary syndromes. Ann Pharmacother. 2005;39:1792-7.
- [Google Scholar]
- Validation of patient reports, automated pharmacy records, and pill counts with electronic monitoring of adherence to antihypertensive therapy. Med Care. 1999;37:846-57.
- [Google Scholar]
- Randomized trial of an education and support intervention to prevent readmission of patients with heart failure. J Am Coll Cardiol. 2002;39:83-9.
- [Google Scholar]
- Patient adherence to treatment: Three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26:331-42.
- [Google Scholar]






