Translate this page into:
Lactate enhanced-quick Sequential Organ Failure Assessment 2 (LqSOFA2): A new score for bedside prognostication of patients with sepsis
For correspondence: Dr Mradul Kumar Daga, Department of Medicine, Maulana Azad Medical College, New Delhi 110 002, India e-mail: drmraduldaga@gmail.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Early diagnosis and prompt treatment remain a challenge in sepsis. To study the role of quick Sequential Organ Failure Assessment (qSOFA), blood lactate levels and a new score Lactate - Enhanced-qSOFA 2 (LqSOFA2) in predicting outcome in patients with sepsis and their association with established severity scores.
Methods:
This was a prospective, observational study in patients admitted to ICU of a tertiary care hospital in north India. qSOFA, Acute Physiology and Chronic Health Evaluation II (APACHE II), SOFA score and LqSOFA2 were calculated in 150 patients with sepsis. Measurements of lactate and SOFA score was done on days one, three and seven.
Results:
The mean arterial pressure (MAP) was significantly higher in survivors (70.14±19.54 vs. 48.53±26.86). The mean qSOFA significantly predicted mortality (1.81 vs. 2.63; P<0.0001). The mean lactate on days one, three and seven in survivors were 2.27±0.91, 1.72±0.77 and 1.14±0.48, respectively, while it was 4.32±2.35, 3.57±2.28 and 2.13±1.22, respectively, in the non-survivor group (P<0.001). The new score LqSOFA2 also significantly predicted mortality between non survivors and survivors (3.52±0.71 vs. 2.37±0.91). There was a significant correlation of qSOFA with SOFA and APACHE II on day one. Lactate levels and SOFA correlated on all three days.
Interpretation & conclusions:
qSOFA, a novel score and lactate can independently predict mortality in patients with sepsis. They correlate with APACHE II and SOFA but fail to equilibrate with either. The combination score LqSOFA2 showed marginal (statistically insignificant) increase in predictive accuracy and specificity when compared to lactate or qSOFA alone. Early diagnosis by LqSOFA2 makes it a good standalone bedside prognostic marker.
Keywords
APACHE II
lactate
mortality
quick sequential organ failure assessment
sequential organ failure assessment
sepsis
Sepsis, a syndrome of pathological and biochemical abnormalities induced by infection, is a hidden public health disaster. It is associated with high morbidity and mortality and accounted for $23.7 billion in health care expenditures in 20131. The magnitude of the problem is depicted by worrisome incidence varying from 240 to 1031 per 100,000 general population in different studies234. Moreover, data from developing countries remain exceedingly scarce representing the submerged iceberg. The mortality rates are as high as up to 20-40 per cent, with a stark increase up to 80 per cent in patients presenting with septic shock5.
Sepsis III guidelines define sepsis as life-threatening organ dysfunction caused by a dysregulated host response to infection6. Organ dysfunction can be identified as an acute change in total Sequential Organ Failure Assessment (SOFA) score by two points consequent to the infection7. Septic shock is defined as hypotension requiring the use of vasopressors to maintain the mean blood pressure of 65 mmHg or greater and having a serum lactate level >2 mmol/l persisting after adequate fluid resuscitation6.
The diagnosis of sepsis and evaluation of its severity is complicated by the highly variable and non-specific nature of the signs and symptoms of sepsis. Therefore, the early diagnosis and stratification of the severity of sepsis are important which necessitates the search for prognostic scores and markers8.
A sepsis marker is useful only if it adds value to the physician’s clinical judgment. Ideally, it should shorten the time to as well as improve the diagnosis, differentiate between infectious and non-infectious causes of systemic inflammatory response syndrome (SIRS) and reflect the effectiveness of antimicrobial treatment. Innumerable biomarkers have been tried from non-specific acute phase reactants like C-reactive protein9 to non-feasible and expensive CD markers10.
Lactate is one such biomarker which has been studied as a marker of critical illness severity for decades11. Conventionally, lactic acidosis in sepsis is attributed to anaerobic glycolysis due to inadequate oxygen delivery. However, it has become clear that the mechanism of hyperlactataemia in sepsis is multifactorial. A higher level usually portends worse outcomes, and there is growing evidence of lactate clearance being a standalone prognostic marker12.
Scoring systems are extremely important for prognostication and management of the patients in critical care medicine. The Acute Physiology and Chronic Health Evaluation II (APACHE II) and the SOFA are the most commonly used scoring systems in patients of sepsis and septic shock713. Though highly accurate, a long list of 12 variables makes APACHE II calculation a tedious task. Similarly, SOFA score requires a mandatory laboratory investigation which obviates its use at the bedside. Sepsis III Task Force recommended qSOFA score (also known as quick SOFA) as a bedside prompt that may identify patients with suspected infection who are at a greater risk for a poor outcome outside the intensive care unit (ICU). It includes systolic blood pressure, respiratory rate and abnormal mentation.
In the present study, the role of lactate levels, qSOFA and a new score LQSOFA2 (a combination of lactate and qSOFA) were studied in predicting the outcomes in patients with sepsis.
Material & Methods
Study design: This study was a prospective observational study conducted in the department of Medicine, Maulana Azad Medical College and associated Lok Nayak Hospital, New Delhi, India, which included patients with sepsis admitted in the medical wards and ICU from May 2017 to January 2018. The study was conducted after being approved by the Ethical Committee of the Institute and obtaining informed consent from the patients. Based on previous literature, using adjusted odds ratio (OR) = 4.87 (predicting mortality in patients with normal and increased lactate levels) and keeping a level of significance at 95 per cent (α=0.05) and power of the study (1-β) at 80 per cent, with absolute error of 10 per cent as acceptable, the calculated sample size was 15014.
Patient selection: The patients with suspected sepsis as per standard criteria laid down in Sepsis guidelines 2016 (SEPSIS 3) were included in the study6. Patients with trauma, burns, anaphylaxis or those admitted for more than 24 h were excluded. This study enrolled 150 cases of sepsis, followed them through a period of seven days and categorized them into two categories. Group 1: survivors; and Group 2: non-survivors. All patients were assessed by history and physical examination and were subjected to a baseline laboratory workup. Standard treatment protocols were followed.
A new LqSOFA2 score i.e. a combination of qSOFA score and lactate level of more than or equal to 2 was devised in the present study. One additional point was added to patients with lactate levels of more than or equal to 2 (the weightage was determined as 1 point keeping in alignment with the variables of qSOFA also having 1 point). The aim was to find out whether the combination is able to match either APACHE II or SOFA.
qSOFA score, LqSOFA2 and APACHE II score were calculated at admission while blood lactate levels were done on the same days. SOFA score was also calculated on day one, three and seven. The study tried to evaluate the prediction of mortality by qSOFA, lactate and LqSOFA2 and compare its performance with APACHE II and SOFA scores.
Measurement of lactate levels: The blood lactate levels were measured using arterial blood gas analyzer. Heparinized blood samples were taken from the radial, brachial or femoral artery and were processed within 15 min of withdrawal.
Statistical analysis: The data were analyzed on the SPSS software version 25 (IBM Corp. IL, USA). The quantitative data were summarized using mean, standard deviation and were compared using independent t test while the qualitative data were summarized using proportions. The association between two quantitative variables was done using the Pearson’s correlation test. Based on the results of this univariate analysis, the factors which were found to be significant in association with mortality were taken as input variables in the logistic regression model. This model was used to find out independent predictors for mortality.
Results
The mean age of the study population was 48.46±15.28, with slight male predominance (58%). The respiratory system (47.3%) was the most common source of sepsis, closely followed by the genitourinary tract (31.3%). The day seven mortality was 48.67 per cent in our study.
The mean qSOFA was 2.63 in the non-survivor group and 1.81 in survivors, a significant difference of 0.82 (P<0.0001).
For the primary objective, lactate was measured on days one, three and seven. The mean lactate on day one was 4.32±2.35 in non-survivors and 2.27±0.91 in patients who survived. The mean lactate levels on day three and seven in non-survivor group were 3.57±2.28 and 2.13±1.22, respectively, while these were 1.72±0.77 and 1.14±0.48, respectively, in the survivor group. On independent t test, all three were highly significant (P<0.0001).
On analyzing our newly devised LqSOFA2 score i.e. a combination of qSOFA score and lactate level of more than or equal to 2, we observed the mean difference (2.37±0.91 vs. 3.52±0.71) between survivor and non-survivors was significant using independent t test (Table I).
| Parameters | Outcome | Mean±SD | Mean difference |
|---|---|---|---|
| qSOFA | Non-survivors | 2.63±0.57 | 0.82*** |
| Survivors | 1.81±0.67 | ||
| Lactate day one | Non-survivors | 4.32±2.35 | 2.04*** |
| Survivors | 2.27±0.92 | ||
| Lactate day three | Non-survivors | 3.57±2.28 | 1.87*** |
| Survivors | 1.71±0.78 | ||
| Lactate day seven | Non-survivors | 2.13±1.23 | 0.99*** |
| Survivors | 1.14±0.48 | ||
| LqSOFA2 | Non-survivors | 3.52±0.71 | 1.15*** |
| Survivors | 2.37±0.91 |
P***<0.001. SD. Standard deviation; LqSOFA, lactate-enhanced-qSOFA
Initially the lactate levels were more than 2, the OR was 5.789 [95% confidence interval (CI) 2.697-12.427, P<0.001]. The OR progressively increased to 13.679 (95% CI 5.997-31.201, P<0.001) and 14.011 (95% CI 5.073-38.698, P<0.001) for lactate levels more than 3 and 4, respectively.
APACHE II was calculated in all patients at admission. The scores ranged from 5 to 52, with a mean APACHE II score of 23.51±10.06. The mortality increased dramatically when the APACHE II score was >30. In our study, mortality was 100 per cent if the score was more than 34. The mean of the APACHE II score in the survivor group was 16.23±6.10 which was significantly lower than that in the non-survivor group 31.19±7.23.
For determining the use of SOFA score as a prognostic marker in patients with sepsis, SOFA score was calculated on days one, three and seven and SOFA (mean) was also used. The SOFA score on day one ranged from 0 to 19, with a mean of 8.84±4.49. The mortality percentage increased with increasing SOFA day one scores with 100 per cent mortality when the score was more than 16. The mean SOFA in the non-survivors was 12.25±3.65 which was significantly higher than in survivors 3.64±2.28. The mean SOFA score on day one and three were 12±3.45 vs. 5.84±3.08 and 11.54±4.24 vs. 3.69±2.71 between two groups which were also significant, (P<0.0001). The SOFA score on day seven also showed significant difference between the two means, 10.00±6.02 vs. 1.29±1.54 (P<0.0001).
Correlation of the qSOFA score with other prognostic markers was calculated. There was a significant correlation (P=0.001) of qSOFA with serum lactate Day one and APACHE II, Pearson correlation coefficient values of 0.474 and 0.735, respectively (Fig. 1).
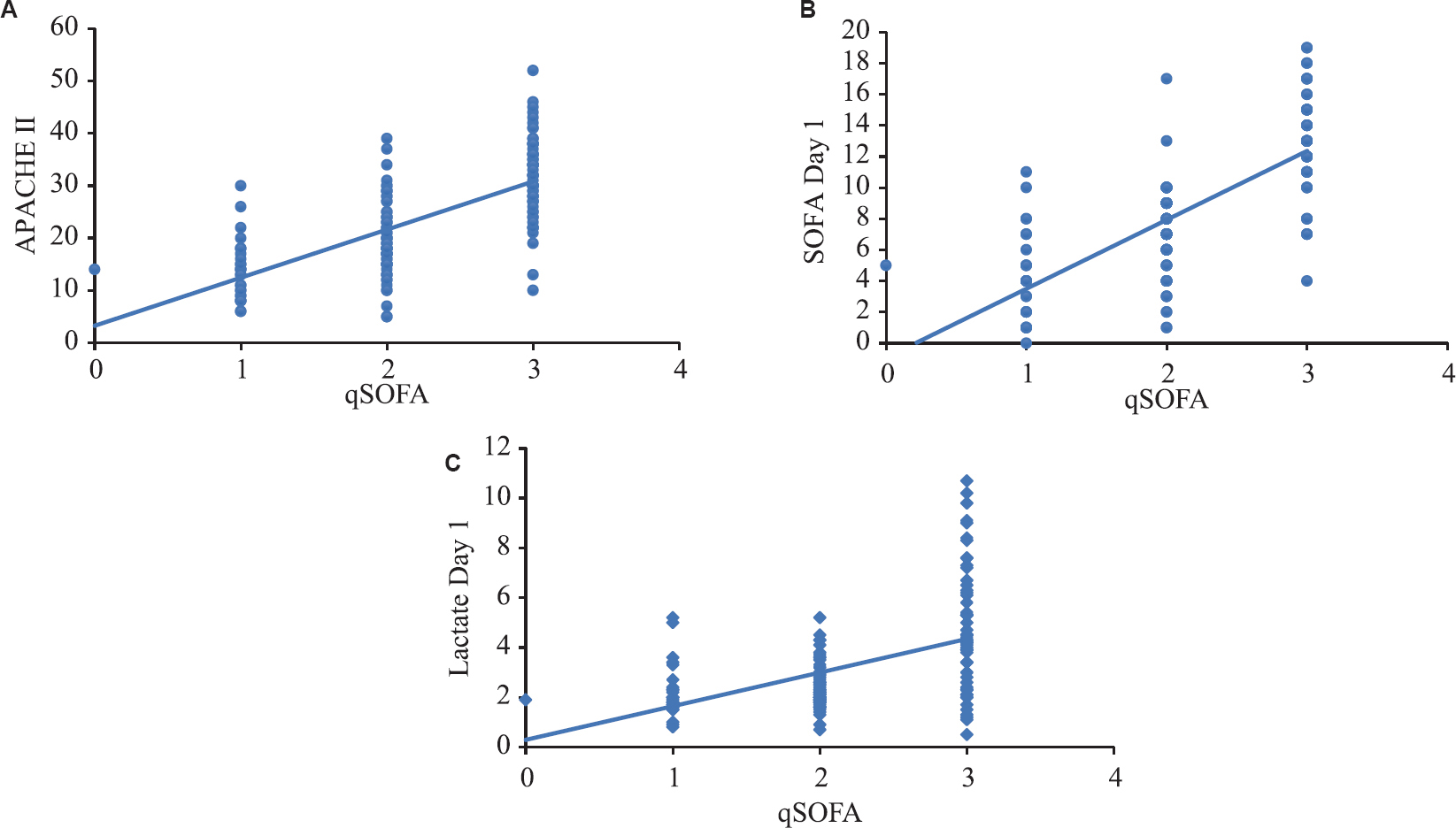
- Correlation of qSOFA (quick Sequential Organ Failure Assessment) with (A) APACHE II (Acute Physiology and Chronic Health Evaluation II) and (B) lactate 1.
Similarly, a significant correlation (P<0.001) of lactate with APACHE II was observed with Pearson’s correlation coefficient values of 0.651. Lactate levels also correlated with SOFA score on day one, three and seven, respectively (Fig. 2).
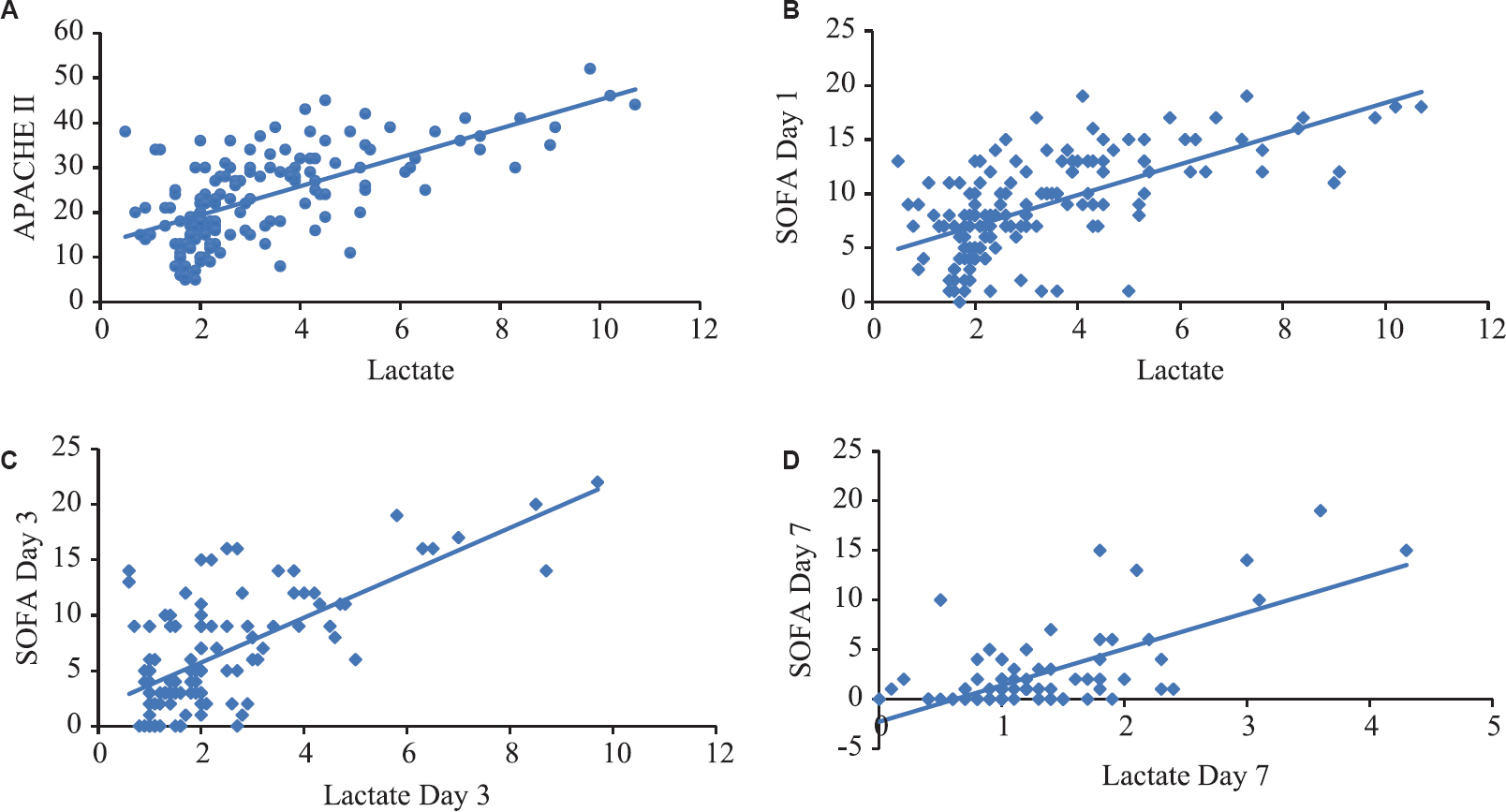
- Correlation of lactate with (A) APACHE II; (B) SOFA score on day one, (C) three and (D) seven.
The new score LqSOFA2 also significantly correlated with APACHE II (r=0.752) and SOFA score (r=0.707).
Based on the results of our study, all four scores or markers were found to be significant in association with mortality. Taking them as input variables in the logistic regression model, we tried to find the independent predictor(s) of mortality. Using qSOFA, lactate day one, SOFA day one and APACHE II as the variables, APACHE II emerged as an independent predictor for mortality with OR 16.724 (P=0.001).
Receiving operator characteristic (ROC) curves (Table II and Fig. 3) were constructed for qSOFA, lactate, LqSOFA2, APACHE II and SOFA scores to identify cut-offs that can predict mortality with optimum sensitivity and specificity. More the area under ROC (AUROC), better the prognostic marker15.
| Parameters | AUROC | SE |
|---|---|---|
| qSOFA | 0.804*** | 0.036 |
| Lactate 1 | 0.802*** | 0.038 |
| LqSOFA 2 | 0.829*** | 0.034 |
| SOFA (mean) | 0.971*** | 0.013 |
| APACHE II | 0.943*** | 0.017 |
P ***<0.001. SE, standard error; SOFA, sequential organ failure assessment; qSOFA, quick-SOFA; SE, standard error; APACHE II, AUROC, area under the receiver operating characteristics
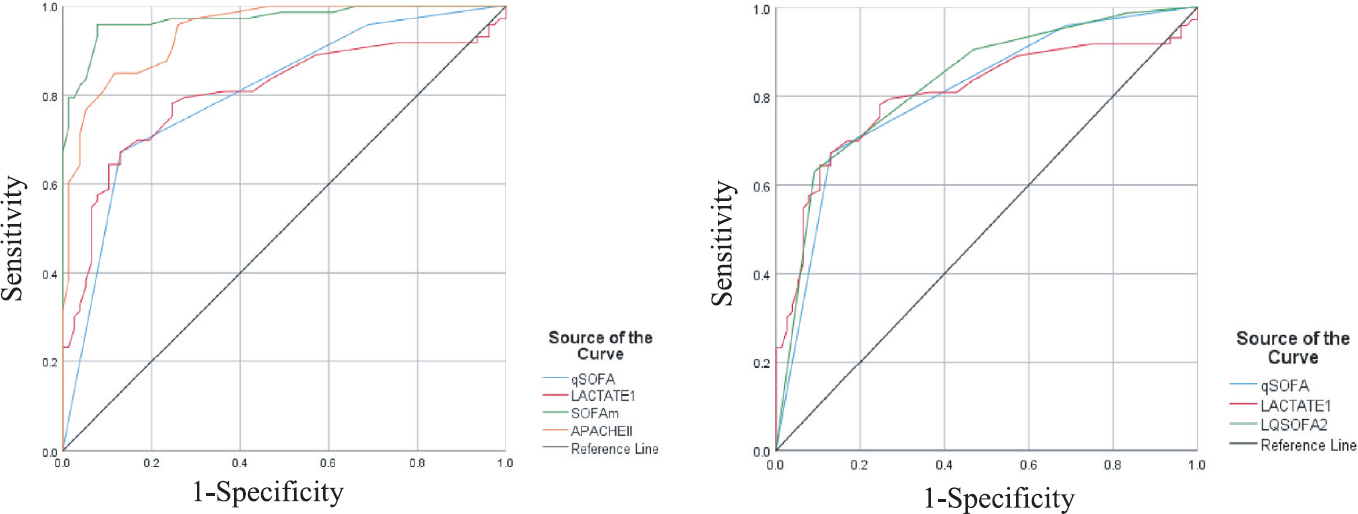
- Comparative receiving operator characteristic curves (ROC) of various qSOFA, lactate 1, APACHE II and LqSOFA.
The mean SOFA was the best among the five parameters to predict mortality (AUROC=0.971, 95 per cent CI 0.946-0.996, P<0.0001). A SOFA score of more than 8.5 predicted mortality sensitivity and specificity of 83.6 and 83.1 per cent, respectively. The AUROC for the new score LqSOFA2 was not insignificant but better (0.829) than qSOFA (0.804) or lactate (0.802) alone.
Discussion
The mean APACHE II was significantly higher in non-survivors in the present study. Higher the score more was the mortality. APACHE II of more than 22.5 was found to predict mortality with a sensitivity of 84.9 per cent and specificity of 83.1 per cent. APACHE II also emerged as an independent predictor of mortality among the four variables; however, it is time-consuming, complex and needs a battery of investigations.
The arithmetic mean SOFA was significantly higher in the non-survivor group. Similarly, the mean SOFA score on days one, three and seven showed a significant difference between the two groups. Similar findings were also observed by Vosylius et al16 and since the SOFA scores show high accuracy in describing the course of organ dysfunction, which in turn strongly affects the outcome, it was concluded that successive SOFA scores were better in predicting outcome compared to one-time scoring. The mean SOFA had an AUROC of 0.971 (95% CI 0.946-0.996, P<0.0001) which was comparable to the observations in previous studies by Rivera-Fernández et al (0.91-0.95)17 and Ferreira et al (0.88)18. Thus, it is suggestive of the good predictive value of SOFA score, be it mean or at admission, for the outcome.
The mean qSOFA in the non-survivor group was 2.63, which was higher than 1.181 in survivor group. This suggested that qSOFA can predict prognosis in patients with sepsis which was a consistent finding in studies by Seymour et al19 and Finkelsztein et al20 as well. In our study, AUROC being 0.804 (95% CI, 0.73-0.87; P<0.001) was comparable to studies by Finkelsztein et al20 (AUROC 0.74) and Raith et al21 (AUROC 0.762). Taking previous studies into consideration, qSOFA scores over SIRS criteria in the prediction of mortality but lags behind SOFA score, finding which was observed in our study as well. There was a significant correlation (P=0.001) of qSOFA with mortality as the outcome and APACHE II (r values of 0.556 and 0.735, respectively). Lembke et al22 conducted a retrospective cohort study in 15,078 patients challenging the notion that SIRS can be replaced by qSOFA as a screening test for sepsis. They concluded that SIRS is the most sensitive predictor of mortality, but lacks specificity, whereas qSOFA is more specific but with the lower sensitivity, a finding which was corroborated by Fernando et al23 in a study of 1708 patients (qSOFA: sensitivity - 64.9%; specificity - 92.2%; SIRS: sensitivity - 91.6%; specificity - 23.6%). Using three out of six parameters from the SOFA score, qSOFA performed reasonably in prognostication of patients outscoring SIRS criteria but the SOFA score remained a touchstone. The use of binary scoring by qSOFA as compared to grading used by SOFA score explains the discrepancy in predictive accuracy. However, being a score requiring no investigations, qSOFA can be a useful bedside tool in diagnosis and prognostication.
The mean lactate levels on day one was significantly lower in survivors as compared to the non-survivors group, a finding which suggests that initial lactate levels can be a prognostic marker in patients with sepsis24. However, Bakker et al25 have previously reported no significant reduction in the initial lactate levels among the survivors in their study. It elucidated that lactate clearance was a more important survival influencing factor than initial lactate level. The mean lactate on day three and seven was significantly higher among non-survivors. The AUROC for prediction of mortality at day seven was 0.802 (95% CI 0.728-0.877, P<0.0001) which was consistent with the results in a study by Lee et al26 (AUROC 0.749). There was a significant correlation (P<0.0001) of lactate levels with mortality as the outcome and APACHE II [r values of 0.506 and 0.651, respectively; (P<0.001)]. An important finding in this study was the significant correlation between lactate levels with SOFA score on day one, three and seven. With availability of blood gas analyzers in wards and ICU, blood lactate levels will obviate the need for whole battery of investigations (required for SOFA scoring) to be repeated every time for prognostication during the course of the hospital stay. Thus, serial lactate levels can be an easier and effective tool for prognosis of patients with sepsis.
The newly devised LqSOFA2 score was significantly higher among non survivors. It correlated with the established scores as well. It marginally improves the predictive accuracy (0.829) and increases the specificity (from 87% to 90.9%) for detecting patients with sepsis, when compared to either qSOFA or lactate alone (difference not significant). In a previously published Indonesian study, they found that qSOFA (AUROC=0.70) lags behind SOFA (AUROC=0.75) significantly suggesting plausible outcomes for resource-limited countries like ours. However, the addition of lactate levels (cut-off >2 mmol/l) to qSOFA significantly improved its performance (AUROC=0.74) vis-à-vis SOFA27. In our study, however, it fell short of the SOFA score. In a subset of the population that involves people with suspected sepsis, this higher specificity would be beneficial in identifying such patients. Given the need for only a single easy and widely available bedside investigation in scoring, this score has the potential to shift the process of prognostication from laboratories to patients’ bedsides. Moreover, earlier availability will save valuable time in the management of sepsis, especially in resource-limited countries like ours. Large-scale longitudinal studies are required to further elaborate the results.
Overall qSOFA, a novel score and lactate levels are reliable and are good prognostic markers of sepsis. These are good bedside diagnostic tools which are easier and quicker to use. The new score LqSOFA2 increases the specificity and prognostic accuracy (although not statistically) as compared to qSOFA or lactate alone. The instant availability of qSOFA and lactate along with comparable sensitivity and specificity makes them suitable predictors of mortality in patients with sepsis; however SOFA score remains a touchstone. A study on a large population would provide further validation to this new score.
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- Vital signs:Epidemiology of sepsis:Prevalence of health care factors and opportunities for prevention. MMWR Morb Mortal Wkly Rep. 2016;65:864-9.
- [Google Scholar]
- The burden of sepsis-associated mortality in the United States from 1999 |mto |d2005:An analysis of multiple-cause-of-death data. Crit Care. 2009;13:R28.
- [Google Scholar]
- Benchmarking the incidence and mortality of severe sepsis in the United States. Crit Care Med. 2013;41:1167-74.
- [Google Scholar]
- National estimates of severe sepsis in United States emergency departments. Crit Care Med. 2007;35:1928-36.
- [Google Scholar]
- Sepsis in European Intensive Care Units:Results of the SOAP study. Crit Care Med. 2006;34:344-53.
- [Google Scholar]
- The third international consensus definitions for sepsis and septic shock (sepsis-3) JAMA. 2016;315:801-10.
- [Google Scholar]
- The Sequential Organ Failure Assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation. Crit Care Med. 2009;37:1649-54.
- [Google Scholar]
- The lingering consequences of sepsis:A hidden public health disaster. JAMA. 2010;304:1833-4.
- [Google Scholar]
- Comparison of procalcitonin and C-reactive protein as markers of sepsis. Crit Care Med. 2003;31:1737-41.
- [Google Scholar]
- Experimental and clinical studies on lactate and pyruvate as indicators of the severity of acute circulatory failure (shock) Circulation. 1970;41:989-1001.
- [Google Scholar]
- Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med. 2004;32:1637-42.
- [Google Scholar]
- APACHE II:A severity of disease classification system. Crit Care Med. 1985;13:818-29.
- [Google Scholar]
- Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med. 2009;37:1670-7.
- [Google Scholar]
- Sensitivity, specificity, receiver-operating characteristic (ROC) curves and likelihood ratios:communicating the performance of diagnostic tests. The Clin Biochem Rev. 2008;29(Suppl 1):S83.
- [Google Scholar]
- Sequential organ failure assessment score as the determinant of outcome for patients with severe sepsis. Croat Med J. 2004;45:715-20.
- [Google Scholar]
- Analysis of physiologic alterations in Intensive Care Unit patients and their relationship with mortality. J Crit Care. 2007;22:120-8.
- [Google Scholar]
- Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286:1754-8.
- [Google Scholar]
- Assessment of clinical criteria for sepsis:For the third international consensus definitions for sepsis and septic shock (Sepsis-3) JAMA. 2016;315:762-74.
- [Google Scholar]
- Comparison of qSOFA and SIRS for predicting adverse outcomes of patients with suspicion of sepsis outside the Intensive Care Unit. Crit Care. 2017;21:73.
- [Google Scholar]
- Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the Intensive Care Unit. JAMA. 2017;317:290-300.
- [Google Scholar]
- Sensitivity and specificity of SIRS, qSOFA and severe sepsis for mortality of patients presenting to the emergency department with suspected infection. Chest. 2017;152:A401.
- [Google Scholar]
- Sepsis-3 septic shock criteria and associated mortality among infected hospitalized patients assessed by a rapid response team. Chest. 2018;154:309-16.
- [Google Scholar]
- Prognostic value of lactate and central venous oxygen saturation after early resuscitation in sepsis patients. PLoS One. 2016;11:e0153305.
- [Google Scholar]
- Serial blood lactate levels can predict the development of multiple organ failure following septic shock. Am J Surg. 1996;171:221-6.
- [Google Scholar]
- Lactate clearance and vasopressor seem to be predictors for mortality in severe sepsis patients with lactic acidosis supplementing sodium bicarbonate:A retrospective analysis. PLoS One. 2015;10:e0145181.
- [Google Scholar]
- Prognostic accuracy of the quick Sequential Organ Failure Assessment (qSOFA)-lactate criteria for mortality in adults with suspected bacterial infection in the emergency department of a hospital with limited resources. Emerg Med J. 2020;37:363-9.
- [Google Scholar]






