Translate this page into:
Labour & delivery monitoring patterns in facility births across five districts of India: A cross-sectional observational study
For correspondence: Dr Shalini Singh, Division of Reproductive Biology, Maternal & Child Health, Indian Council of Medical Research, Ansari Nagar, New Delhi 110 029, India e-mail: shalinisingh.icmr@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
India has recorded a marked increase in facility births due to government's conditional cash benefit scheme initiated in 2005. However, concerns have been raised regarding the need for improvement in the quality of care at facilities. Here we report the monitoring patterns during labour and delivery documented by direct observation in reference to the government's evidence-based guidelines on skilled birth attendance in five districts of India.
Methods:
A cross-sectional study design with multistage sampling was used for observation of labour and delivery processes of low-risk women with singleton pregnancy in five districts of the country. Trained research staff recorded the findings on pre-tested case record sheets.
Results:
A total of 1479 women were observed during active first stage of labour and delivery in 55 facilities. The overall frequency of monitoring of temperature, pulse and blood pressure was low at all facilities. The frequency of monitoring uterine contractions and foetal heart sounds was less than the expected norm, while the frequency of vaginal examinations was high at all levels of facilities. Partograph plotting was done in only 15.8 per cent deliveries, and labour was augmented in about half of the cases.
Interpretation & conclusions:
The findings of our study point towards a need for improvement in monitoring of maternal and foetal parameters during labour and delivery in facility births and to improve adherence to government guidelines for skilled birth attendance.
Keywords
Guidelines
labour monitoring
partograph
quality of care
skilled birth attendance
The presence of skilled care during delivery and soon after childbirth is considered one of the most cost-effective interventions to attain the Sustainable Development Goal 3 of reducing maternal mortality ratio to <70 per 100,000 live births123. The Government of India (GOI) in 2005 initiated incentivizing facility births through the Janani Suraksha Yojana to increase the coverage of skilled attendance at birth4 and published Guidelines for Skilled Birth Attendance to assist the health personnel to effectively provide good quality maternity care4. The overall institutional delivery rate has doubled from 43 per cent in 2008 to 84 per cent in 20135, however, India lags behind in achieving the goal for reduction in maternal deaths678. The need of improving training and skills of healthcare providers as well as service delivery have been raised in the reports of the Joint Review Mission and the Common Review Mission which were commissioned for monitoring and evaluating the programme78. There is a paucity of data on implementation of the guidelines on skilled birth attendance at the facility level. Therefore, this cross-sectional direct observational study was conducted to evaluate the provider practices and processes during labour and early post-partum period vis-à-vis the government guidelines on skilled birth attendance in five districts of the country.
Material & Methods
Study area and design: The study was conceptualized and coordinated by the division of Reproductive Biology, Maternal & Child Health, Indian Council of Medical Research (ICMR), New Delhi, India. This direct observational study was carried out using a cross-sectional study design during June 2010-April 2011. Multistage sampling was followed; in the first stage, five States were selected, namely Rajasthan and Gujarat in the West, Uttar Pradesh in the North, Odisha from the East and Tamil Nadu from the Southern region of India. In the next stage, one district from each State was selected based on the convenience of the core research unit and the suggestions received from the Ministry of Health & Family Welfare, GOI. These were Jaipur (Rajasthan), Allahabad (Uttar Pradesh) and Cuttack (Odisha) from Empowered Action Group States with poor performance in maternal health, Vadodara (Gujarat) with medium performance and Thiruvallur (Tamil Nadu) with good performance in maternal health. In the third stage, all public health facilities in the selected districts were enumerated for random selection. In the urban areas, 11 public health facilities were selected which included five medical colleges (MCs), five district hospitals (DHs) and one sub-DH. In the rural areas, first referral units (FRUs)/community health centres (CHCs) with more than 500 deliveries and primary health centres (PHCs) with more than 200 deliveries in the past year and accessible by road from the MC within 2-3 hours were selected. These included 20 FRUs/CHCs and 24 PHCs.
Sample size calculation: Assuming the prevalence of the use of antepartum oxytocin to be around 50 per cent in the deliveries observed, the sample size was calculated at 95 per cent confidence level, with margin of error of 10 per cent and a design effect of 1.5; a sample of 144 women each, in urban and rural areas of the chosen study districts was required.
Site preparation: One nodal officer from the State Health Department coordinated the study implementation in the chosen district. The research staff underwent centralized training at ICMR headquarters, New Delhi on study protocol, implementing strategies, data collection and data entry procedures and regular monitoring was done by site investigators and central coordinating unit from ICMR.
Study population: Women with singleton pregnancy of more than 34 wk gestation, in active first stage of labour (cervical dilation >4 cm), with no obvious obstetric or medical complications and willing to participate in the study were enrolled. Women were observed up to four hours after delivery or till discharge, whichever was earlier. Women who were shifted out of labour room due to referral to a higher centre or for caesarean section or for any other reason and whose observation could not be completed were excluded from the study. Institutional ethical clearance certificates were obtained from all the five district nodal centres and written informed consents were obtained from all the participants.
Variable measurement: A structured pre-tested case record form based on the GOI guidelines for skilled birth attendance was used to record the study data. The observers recorded the number of times the provider(s) carried out different examinations/procedures on each participant from the time of enrolment till delivery. The action of keeping the stethoscope or doptone on the woman's abdomen was considered as examination of foetal heart sound (FHS), keeping hand over uterus during contractions and during interval between two consecutive labour pains was considered as examination of uterine contractions (UCs), applying blood pressure cuff over the upper arm and using stethoscope was considered as measurement of blood pressure.
Statistical analysis: Data entry was done on case record forms and entered in excel sheets at site offices with appropriate coding and de-identification. Range checks and logical checks were run to minimize the errors. For descriptive statistics, quantitative variables were organized as mean (standard deviation) and continuous variables as median (mode), respectively, in analysis.
For each case, the total duration of observation from enrolment to delivery was calculated in minutes, and number of examinations of UCs, FHS and vaginal examination were recorded. Using one examination of UC and FHS in every 30 min and one vaginal examination in every four hours as the standard norm, the number of observations per unit time for each case was calculated.
Kruskal-Wallis test followed by Dunn's test was used for non-parametric pair-wise multiple comparisons in different independent facilities (MCs, DHs, FRUs/CHCs and PHCs) to compare median observation per unit time of UC, FHS examination and vaginal examination. Data were analyzed using STATA (version 13, StataCorp LP, College Station, TX, USA)9.
Results
A total of 1922 women were screened of whom 332 women were excluded as they did not meet the inclusion criteria. Of the remaining 1590 women, 111 whose observations could not be completed due to transfer for Caesarean section, referral and other reasons were further excluded. Thus, a total of 1479 women from 55 facilities completed the study (Fig. 1).
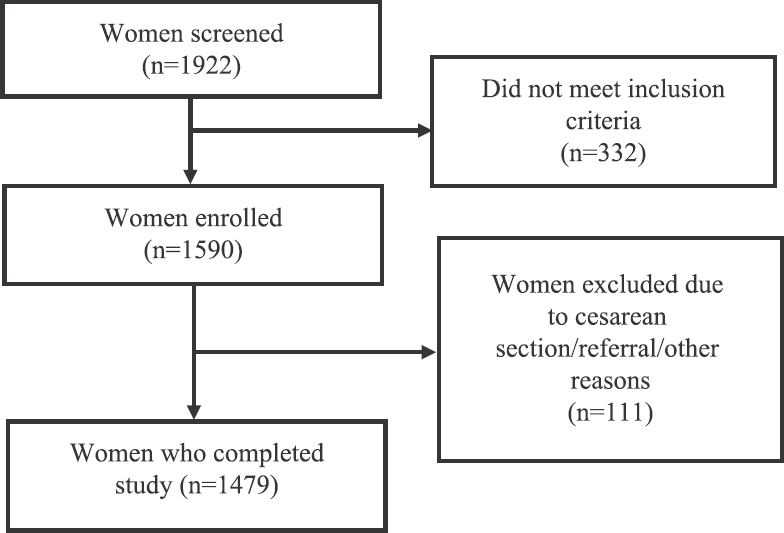
- Flow diagram showing enrolment of study participants.
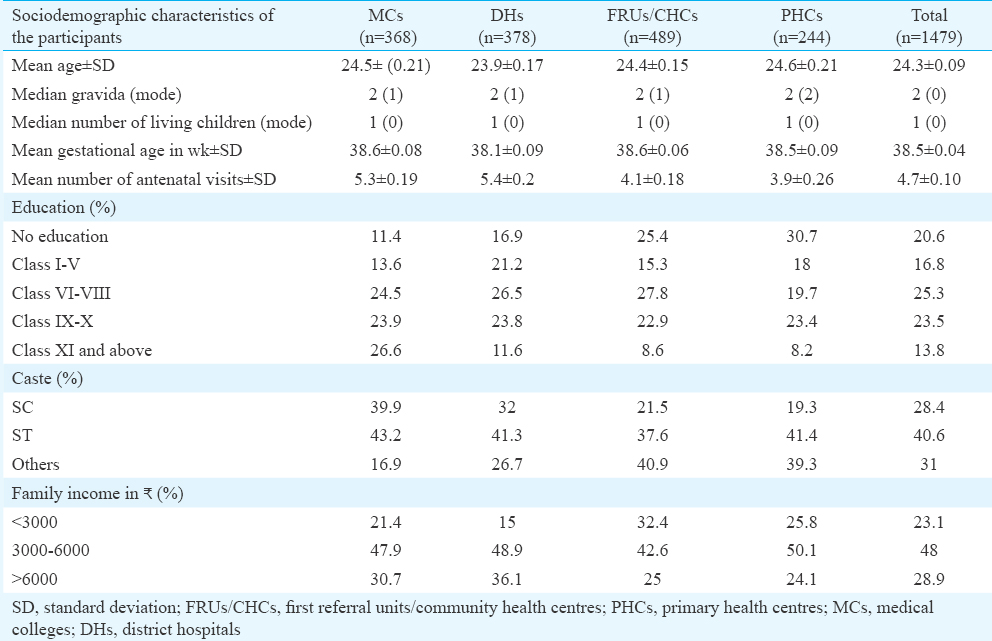
The sociodemographic characteristics of participants are described in Table I. The mean age of the participants was 24.3±0.09 yr. The average number of antenatal visits was 4.7 for all women enrolled. Nearly 30.7 per cent women in the PHCs were uneducated which was three times higher than those enrolled in the MCs.
General & obstetric examination during observation period: The overall frequency of examinations carried out during the observation period is shown in Table II. Uterine contractions was the least measured parameter in obstetric examination at enrolment, and vaginal examinations were done the maximum number of times both at enrolment and during the 1st stage of labour. Plotting of partograph was very low (15.8%), the highest being 21.7 per cent in FRUs/CHCs and the lowest in district/sub DH (1.6%).
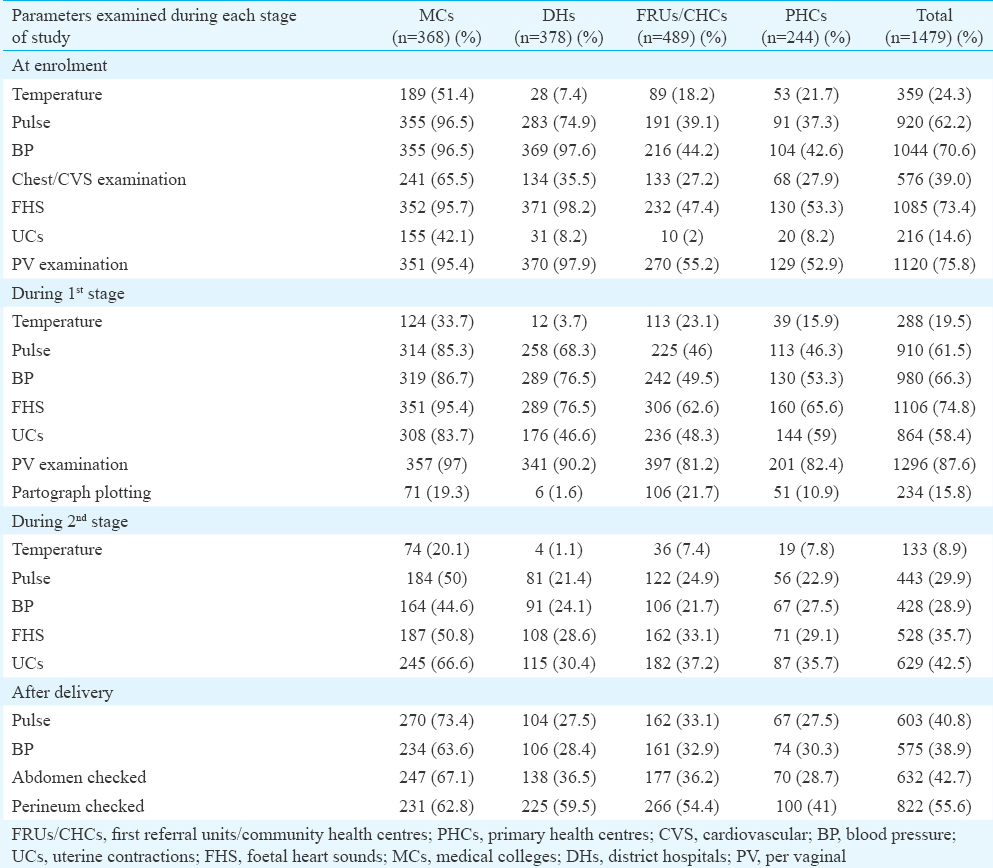
Fig. 2 depicts the proportion of participants in whom four parameters, namley blood pressure, UC, FHSs and vaginal examination were not performed even once during the entire observation period. Monitoring of UCs was poorest in DHs followed by PHCs and FRUs/CHCs. Monitoring of blood pressure and FHS of participants was poor in FRUs/CHCs and PHCs.
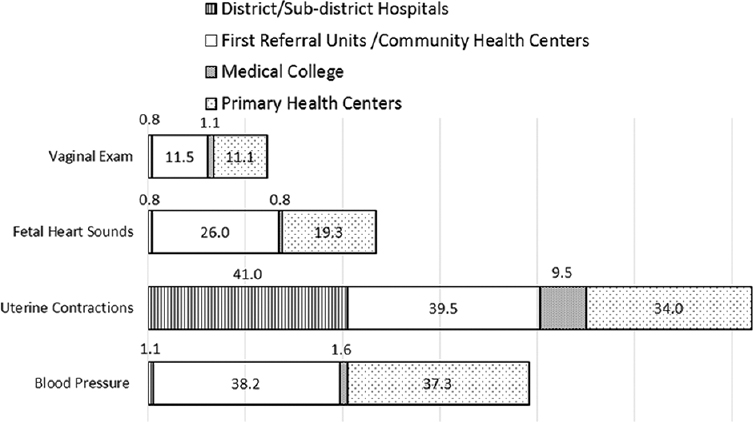
- Facility wise distribution of percentage of women in whom four parameters, namely blood pressure, uterine contraction, foetal heart sounds and vaginal examination were never performed even once during observation period.
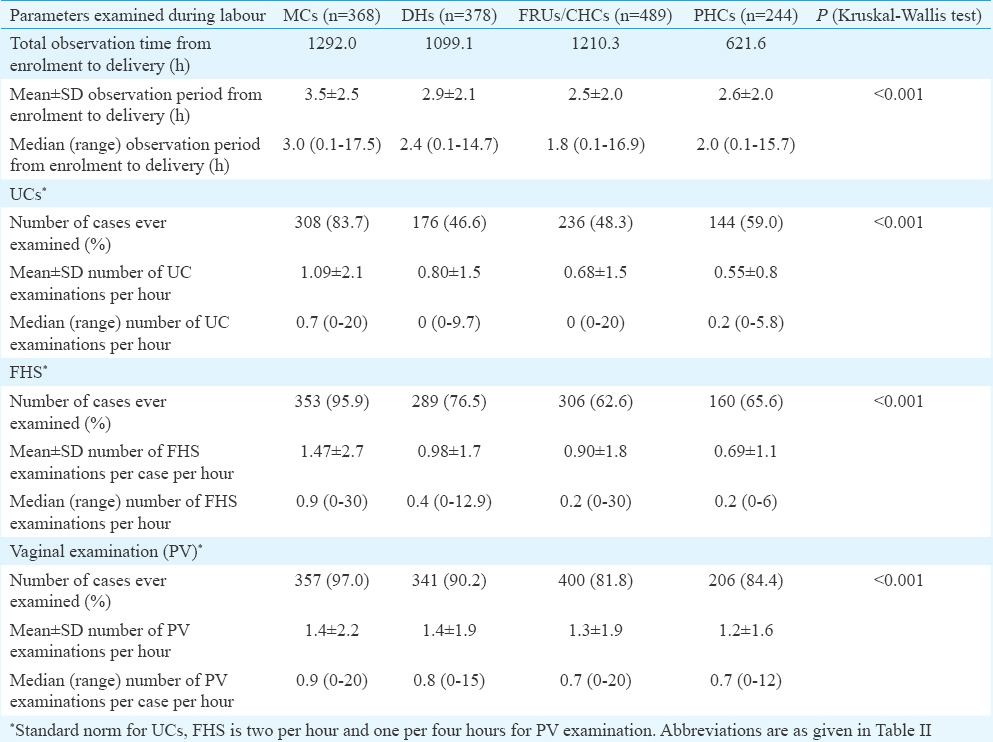
Monitoring during labour: Table III depicts the facility-wise distribution of labour monitoring pattern and its comparison to the expected norm. The median value of the observation time in MCs was significantly higher than all other facilities. The difference in the median observation time between FRUs and PHCs was not significant. The median number of UCs examinations per hour was low in all the facilities when compared to the standard norm (2/h). MCs had significantly higher median values for UCs and FHS examination as compared to all other facilities. The difference in the median number of UC examination between FRUs and PHCs was not significant. The difference in the median number of FHS examination between FRUs and PHCs and DHs and PHCs was also not significant. In contrast to the examination pattern of UCs and FHS, the mean number of vaginal examination per woman was nearly three to four times higher than the standard norm of one examination per four hours across different levels of facilities. Median number of vaginal examinations per hour was higher in MCs as compared to other health facilities. There was no significant difference in the frequency of vaginal examination between FRUs/CHCs and PHCs.
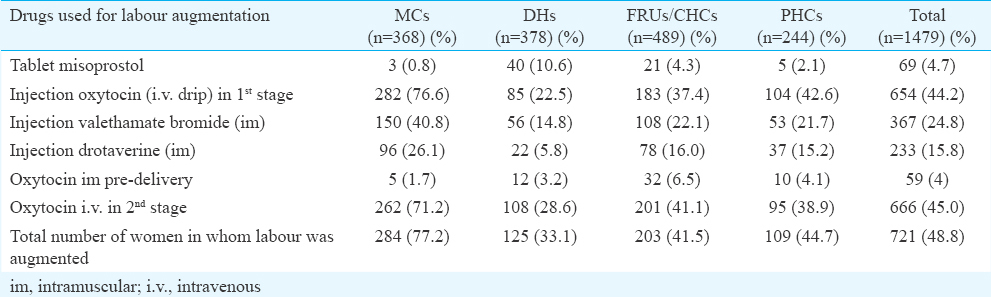
Drugs used during labour: Labour was augmented in nearly half (48.8%) of the total cases observed (Table IV). Nearly 44.7 per cent women observed in PHCs were given drugs to augment labour. In nearly 4.0 per cent women, intramuscular oxytocin was administered during labour before delivery. Intravenous oxytocin was administered in the first stage of labour to 76.6 per cent of women at MCs and only 22.5 per cent of women at DHs. Providers other than doctors (SNs/LHVs/ANMs) were also seen administering oxytocic drugs before delivery (Data not shown).
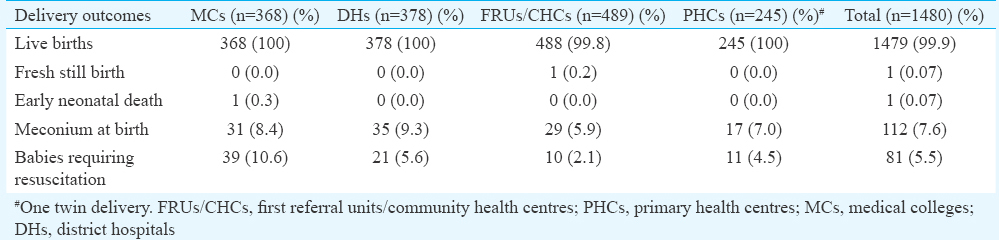
Outcome of delivery: A total of 1480 newborns were delivered including a set of twins (Table V). There were one fresh stillbirth and one early neonatal death during the observation period. Overall, meconium was present in 7.6 per cent deliveries and 5.5 per cent babies required resuscitation.
Discussion
In general, between 70 and 80 per cent of all pregnant women may be considered as low-risk at the start of labour10. While most women go through labour without any need for intervention, some develop complications rapidly. Therefore, regular monitoring of woman and the foetus are crucial to identify any departure from safe delivery and to manage these complications early. Several countries, including Malaysia and Sri Lanka, have demonstrated reduction in maternal and perinatal mortality using the services of skilled birth attendants in facilities supported by adequate equipment, supplies and transport11. Detailed clinical guidelines for intrapartum care published by National Institute for Health and Care Excellence (NICE) provide a framework to the caregivers for monitoring of mother and the foetus12. The Indian guideline on skilled birth attendance incorporates evidence-based best practices as norms for optimal care during normal labour4. Accordingly, after initial assessment of the woman, it is important to monitor maternal pulse, FHS and UCs every 30 min during active first stage of labour and vaginal examination, and blood pressure is recommended at four hourly intervals4.
This study indicates a deficiency of monitoring the general physical well-being of the woman during labour at all levels of healthcare facilities; and the deficiency was higher in the primary and secondary healthcare facilities. Parameters, such as temperature, blood pressure and pulse, were never examined in 19.3 per cent of women enrolled in the study. A study carried out in a teaching hospital in Egypt indicated the omission of assessing temperature (88%), pulse (60%) and blood pressure (19%) among women13 which was similar to observations in our study. Indicators, such as measuring temperature, pulse and blood pressure, are well established, easy to measure and do not require expensive equipment. It is also known that adverse changes in these indicators can affect labour management and pregnancy outcome10. A qualitative study featuring observations of women in labour in rural Rajasthan revealed inadequate monitoring of the maternal and foetal condition (by way of blood pressure and FHSs)14. Nearly one-third of the maternal deaths in India occur during intrapartum period15 and the absence of or infrequent monitoring of these parameters during labour deprives the women of a chance for early diagnosis and management or timely referral to a higher facility when the need arises. The omission of monitoring temperature, pulse and blood pressure may delay the diagnosis of sepsis and preeclampsia which contribute to 11 and 5 per cent of maternal mortality, respectively in India16.
The plotting of partograph is an effective tool for monitoring progress of labour, prevents prolonged and obstructed labour and helps to undertake decision for augmentation, Caesarean section and transfer of women to higher facility for comprehensive emergency obstetric care. These benefits may be more in low-resource settings where the use of standard labour management protocol is inconsistent17. Low use of partograph by providers in peripheral centres of Nigeria18 was similar to the findings of this study. In the MCs, the UCs and FHS examinations were close to the standard norm, but vaginal examinations were nearly six times higher. Preference of monitoring labour progress by frequent vaginal examinations seen in this study has also been reported from other studies in India1920.
The use of oxytocics for augmentation of labour coupled with less than desirable frequency of maternal and foetal monitoring has been reported from a teaching hospital of Egypt21. This study also indicated the inappropriate use of oxytocics such as use of unapproved vaginal misoprostol for labour augmentation, administration of intramuscular oxytocin before delivery, giving unlabelled intravenous oxytocin infusion without proper regulation of dose, administering oxytocin prior to delivery in clinical settings without facilities for Caesarean section such as PHCs and without plotting partograph for monitoring labour. Misuse of intrapartum oxytocin has been reported on the pretext of providing warmth for labour pains and was found to be culturally acceptable and demanded by women and her relatives who want to shorten the process of labour14.
Nearly two-thirds of maternal deaths arise from complications during labour and early postpartum period22. Routine care and early identification of complications play an important role in preventing maternal death and morbidity20.
The strength of the study included reporting on directly observed patterns of labour monitoring covering different geographical regions of the country including from the good, medium and poor performing States with respect to maternal health indicators. The practices in the teaching hospitals were compared with district health system. Limitations of the study included the presence of external observers to document provider practices which might have resulted in modified or better practices (Hawthorne effect). Our study was not designed to evaluate the effect of provider practices on maternal and foetal outcome.
In conclusion, our results indicated an urgent need for strong reforms in the healthcare system, in-service training and monitoring of service delivery at all levels including teaching hospitals and district health system. With an increase in the proportion of institutional deliveries in India, the outcomes for mothers and newborns can be improved by optimizing the use of interventions during birth and improving standards of care through adhering to practice guidelines.
Acknowledgment
Authors acknowledge the technical inputs provided by Dr N.K. Arora, INCLEN India and Dr Dinesh Agarwal, UNFPA India, contributions of Dr (Late) Panna Choudhury, Project Manager, the State Directorates of Health Services and the Chief District Medical Officers of the five selected Districts for their support.
Financial support & sponsorship: The funding support for this study was provided by UNFPA vide Ref No: ICMR-AWP (IND7R21W) and Indian Council of Medical Research, New Delhi (vide project No: 5/7/340/09-RHN).
Conflicts of Interest: None.
References
- 2015. United Nations. Transforming our world: The 2030 agenda for sustainable development. New York: United Nations; Available from: http://www.un.org/en/development/desa/population/migration/generalassembly/docs/globalcompact/A_RES_70_1_E.pdf
- 2015. World Health Organization. Maternal Mortality. Geneva: WHO; Available from: http://www.who.int/news-room/fact-sheets/detail/maternal-mortality/
- Tapping into the resources of skilled birth attendants in reducing the maternal mortality rates in developing nations. Iran J Nurs Midwifery Res. 2017;22:81-2.
- [Google Scholar]
- 2010. Guidelines for Antenatal Care and Skilled Attendance at Birth by ANMs/LHVs/SNs. India. Government of India, Maternal Health Division, Ministry of Health & Family Welfare. Available from: https://www.nhp.gov.in/sites/default/files/anm_guidelines.pdf
- Government of India. National Health Mission - Five Years (2009 – 2014) Achievements & New Initiatives. 2015. New Delhi: Government of India, Ministry of Health and Family Welfare; Available from: http://www.nhm.gov.in/images/pdf/media/publication/fiveyears-of-nhm-2009-2014/5_years_nhm_final.pdf
- [Google Scholar]
- Global, regional, and national levels of maternal mortality, 1990-2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1775-812.
- [Google Scholar]
- 2011. Government of India. National rural health mission reproductive & child health programme phase II 8th Joint Review Mission July - September. New Delhi: Government of India, Ministry of Health and Family Welfare. Available from: http://www.nhm.gov.in/images/pdf/monitoring/jointreview-mission/jrm-8-aide-memoire.pdf
- 2011. Ministry of Health & Family Welfare. 5th common review mission report 2011. New Delhi: Nirman Bhawan, Government of India, Ministry of Health & Family Welfare; Available from: http://www.nhm.gov.in/images/pdf/monitoring/crm/5th-crm/report/main-report-5th-crm.pdf
- StataCorp. Stata statistical software: Release 13. College Station, TX: StataCorp LP; 2013.
- 1997. World Health Organization. Care in normal birth: A practical guide. Geneva: World Health Organization; 24:121-3. Available from: http://apps.who.int/iris/bitstream/10665/63167/1/WHO_FRH_MSM_96.24.pdf
- Organizing delivery care: What works for safe motherhood? Bull World Health Organ. 1999;77:399-406.
- [Google Scholar]
- 2014. Intrapartum care for healthy women and babies | Guidance and guidelines | NICE. Available from: https://www.nice.org.uk/guidance/cg190
- Hospital practice versus evidence-based obstetrics: Categorizing practices for normal birth in an Egyptian teaching hospital. Birth. 2005;32:283-90.
- [Google Scholar]
- Comparison of domiciliary and institutional delivery-care practices in rural Rajasthan, India. J Health Popul Nutr. 2009;27:303-12.
- [Google Scholar]
- Maternal mortality in India: Causes and healthcare service use based on a nationally representative survey. PLoS One. 2014;9:e83331.
- [Google Scholar]
- Registrar General (India). Centre for Global Health Research (Canada). Maternal mortality in India 1997-2003: Trends, causes and risk factors (Sample Registration System). New Delhi: Registrar General India; 2006.
- World Health Organization. WHO recommendations for augmentation of labour. Geneva: World Health Organization; 2014. p. :5.
- Knowledge and use of the partograph among healthcare personnel at the peripheral maternity centres in Nigeria. J Obstet Gynaecol. 2006;26:538-41.
- [Google Scholar]
- Assessment of care in labour in a delivery ward in Gulbarga, India. University of Gothenburg. 2011. Available from: https://gupea.ub.gu.se/bitstream/2077/24531/1/gupea_2077_24531_1.pdf
- [Google Scholar]
- Adherence to evidence based care practices for childbirth before and after a quality improvement intervention in health facilities of Rajasthan, India. BMC Pregnancy Childbirth. 2014;14:270.
- [Google Scholar]
- Labor augmentation in an Egyptian teaching hospital. Int J Gynaecol Obstet. 2004;85:74-80.
- [Google Scholar]
- Strategies for reducing maternal mortality: Getting on with what works. Lancet. 2006;368:1284-99.
- [Google Scholar]






