Translate this page into:
Initial treatment dropout in patients with substance use disorders attending a tertiary care de-addiction centre in north India
Reprint requests: Dr Debasish Basu, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh 160 012, India e-mail: db_sm2002@yahoo.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Dropout from substance use disorders treatment is associated with poor outcomes. Although many factors have been associated with an early dropout of patients, the reasons for dropping out of treatment prematurely remain poorly understood particularly in the Indian context. This study was aimed to study socio-demographic and clinical variables predicting initial dropout of patients attending a tertiary care de-addiction treatment centre in north India.
Methods:
Information was extracted from the records of consecutive newly registered patients from January 2011 to December 2014. The patients who did not come for follow up within 30 days of the first contact were defined as initial dropouts.
Results:
Data of 7991 patients could be retrieved. Majority of the sample consisted of male, married and employed individuals. Of them, 4907 patients (61.3%) were considered initial dropouts. Multivariate analysis revealed that after controlling for other factors, greater age, being employed, lower educational status, lesser duration of substance use, use of alcohol, opiate, tobacco, cannabis or sedative-hypnotic use but the absence of multi-substance use predicted initial drop out.
Interpretation & conclusions:
This study identified some socio-demographic and clinical variables which might predict treatment attrition in substance use disorders. Clinician's awareness towards these factors and tailor-made intervention might improve initial treatment retention. Future research could be directed to find the validity of this assumption.
Keywords
Alcohol
de-addiction
dropout
opioids
retention
substance use disorder
Long-term retention of a patient in any treatment programme is known to be associated with a positive outcome. Moos and Moos1 have demonstrated that initial treatment entry and retention can predict long-term outcome in alcohol dependence, even at the end of 16 yr. Another naturalistic study on mixed substance use disorder population has demonstrated a dose-response relation between duration of treatment and outcome2. Treatment retention in substance use disorder programmes has also been effective in reducing criminal behaviour, improving the state of health, engaging in gainful employment and overall better outcome3. Hence, retaining the individual with substance use disorders in the treatment net constitutes an important goal of treatment. Yet, it is remarkable that high dropout rates are encountered in the substance use treatment settings45. It has been suggested that highest rates of dropouts occur in the initial stages of treatment and can be as high as 50 per cent in the first month of treatment678.
The predictors of attrition from de-addiction treatment setting vary across the studies. A positive association between immediate dropout and male gender, history of mental illness in the family and addiction to alcohol combined with other illicit substance has been shown6. Pre-treatment cocaine use, weak therapeutic alliance with counsellors, secure attachment style and better-coping strategies were associated with shorter retention9. Furthermore, younger age, greater cognitive dysfunction, maladaptive personality functioning, more drug use, lower severity of alcohol dependence and highly controlling treatment environment were found to be associated with dropout1011. A study examining the outpatient sample has found that early dropout was associated with less education, female gender, cocaine as the primary drug and being referred from outside the larger medical centre12. Early age of onset of substance abuse and polydrug abuse are associated with higher risk for early dropout from both in- and out-patient settings131415. Further, client-related factors, such as lower perception of treatment benefits16, depression and avoidance coping17 and lack of social support18 have been shown to relate to higher dropouts.
Although many factors have been shown to be related to early dropout, the reasons for clients dropping out of treatment prematurely remain poorly understood in view of inconsistent findings. The lack of uniform agreement in defining dropout/completion between the studies further adds to this inconsistency. Identifying clients at risk for early dropout may help in focused attempts to increase retention in treatment programme, thereby improving the outcome. The findings of two Indian studies on treatment non-completers in de-addiction setting1920 are limited by the fact that they included only opioid-dependent subjects and were carried within the inpatient setting specifically, hence curtailing the generalizability of results. Studies focusing on substance use disorders at the outpatient setting and including a wide variety of substance use disorders are lacking. Hence, this study was conducted to examine the socio-demographic and clinical variables that predict initial dropout of patients attending a de-addiction outpatient in north India.
Material & Methods
The present study was conducted at the Drug De-addiction and Treatment Centre (DDTC) at Postgraduate Institute of Medical Education and Research (PGIMER), a tertiary care government hospital in Chandigarh, India. Initial treatment of outpatients mainly consists of pharmacotherapy for the withdrawal symptoms and other supportive treatment (e.g. referral to other OPDs in case of medical complications; unstructured brief motivational counselling). For treatment of opioid withdrawal, clonidine is prescribed in the majority along with symptomatic treatment, and alcohol withdrawal is mostly managed with long-acting benzodiazepines (except in cases of liver dysfunction where lorazepam or oxazepam is preferred). Since October 2013 buprenorphine-naloxone (BNX)-based outpatient, detoxification has been made available. However, the prescription of BNX is relatively limited exclusively for detoxification but rather considered in selected cases for long-term opioid substitution therapy. Involvement of the family members is encouraged in all situations. The study was approved by the ethics committee of the Institute and written informed consent was obtained from each participant.
The present study was aimed to assess the dropouts from the Centre who registered themselves at the DDTC outpatient and not admitted during the first one month. The sample comprised all the consecutive patients registered at the DDTC from January 2011 to December 2014 over a span of four years. Computerized databases were used for analyses. The records of the patients contained the demographic details, date of registration, substance use characteristics and follow up notes. The demographic characteristics included variable such as age, gender, marital status, employment status, educational level, religion, residence locality, the type of family and income. The substance use characteristics that were documented included the various substance use disorders and the overall duration of substance use and dependence.
Data extraction from the computerized records were done. The data were analyzed using SPSS version 19 (IBM Corp., NY, USA). For the purposes of the study, ‘initial dropouts’ were defined as those patients who did not follow up at DDTC within 30 days of the initial contact. The period of 30 days was selected for the purposes of the study as all patients were called for follow up in this time frame, most of them within one week of the initial contact. The initial dropout patients were compared with the non-dropout across a range of demographic and clinical variables available from the computerized records. Comparisons were made between the dropout groups with respect to five commonly used substance use disorders encountered at the Centre (alcohol, opioids, tobacco, cannabis and sedative hypnotics). Users of two or more substances except tobacco were classified as having multi-substance use. The diagnosis of substance use disorders (dependence or harmful use) was made by qualified psychiatrists following a clinical interview. Patients who had fulfilled criteria for substance use disorders for two or more substances independently were labelled as multi-substance use. Thus, each of these substance use disorders would need independent attention in their own merit. This group is distinct from the polysubstance dependence as mentioned in the Fourth Edition of the Diagnostic and Statistical Manual of Mental Disorders21, in which in addition to the number of substance to be >2, patient must not fulfil dependence criteria for individual substance. This concept of polysubstance dependence was not considered in the analysis.
Statistical analysis: Appropriate descriptive statistics in the form of mean, standard deviation, frequency and percentage were used to represent the data. Inferential statistics were used to find differences between the initial dropout and the non-dropout groups using parametric tests (Student's t test) and non-parametric tests (Chi-square test). Since the present analysis was based on large data, the possibility of type I error was high. Hence, Cramer V and η2 were used to estimate the clinical effect of the observed differences. A higher value of Cramer V or η2 reflects greater clinically relevant effects. Logistic regression analysis was carried out to find independent predictors of initial dropout. The forwards Wald method22 was used for the logistic regression analysis, utilizing those variables which showed at least a trend level significant difference between initial dropouts and those who were retained (P<0.2). Nagelkerke R2 was used to estimate the variance explained by the model. Missing value imputation was not done as a part of the study. A P<0.003 was considered significant to control for multiple comparisons using the Šidák correction.
Results
From January 2011 to December 2014, 8345 patients were newly registered at the Centre, of which records of 7991 patients could be retrieved (95.6% of the sample). Mean age of the sample was 35.0±11.4 yr, with a median of 33 yr and interquartile range from 26 to 42 yr. The sample comprised an overwhelming majority of males (99.3%). Majority of the sample comprised married and employed individuals. The substances of abuse encountered in the descending order of frequency included tobacco (n=5264), opiates (n=3934), alcohol (n=3554), cannabis (n=698), sedative-hypnotics (n=463), volatile solvents (n=67), stimulants (n=33), hallucinogens (n=32) and cocaine (n=29). The number of multisubstance users (>2 substance use except tobacco) was 1391.
Of the total 7991 patients, 3084 (38.6%) were followed up at least once within the initial 30 days, and 4907 patients (61.4%) did not follow up even once during the initial 30-day period (initial dropout). The differences in demographic and clinical characteristics of those with initial dropout and those retained are shown in Table I. On bivariate comparisons, initial drop-out was associated with greater age, marital status, lower educational status, being employed, rural background, lower incomes, shorter duration of substance use and dependence and use of opiates. Use of alcohol, tobacco, cannabis, sedative-hypnotic and polysubstance abuse was associated with retention into treatment.
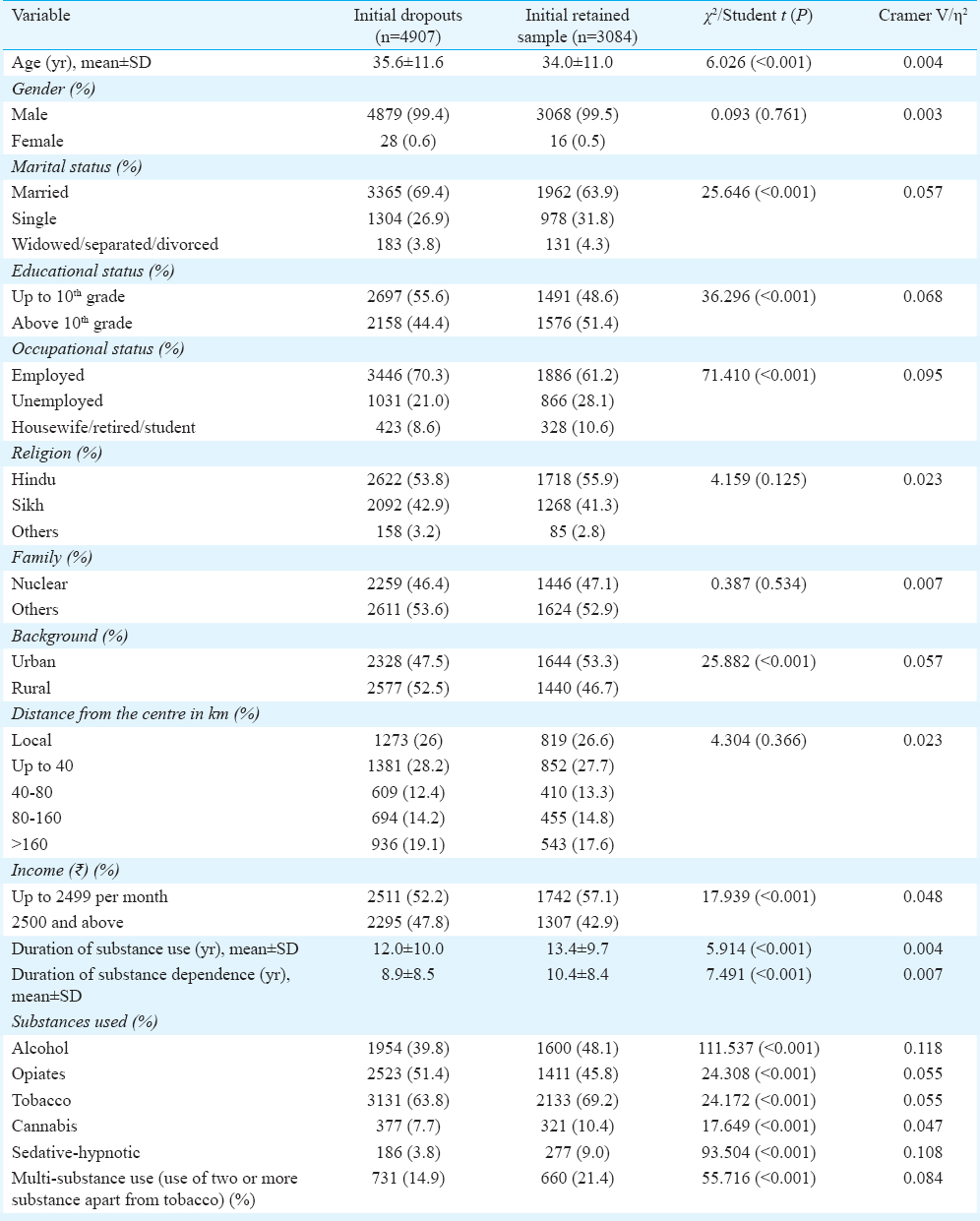
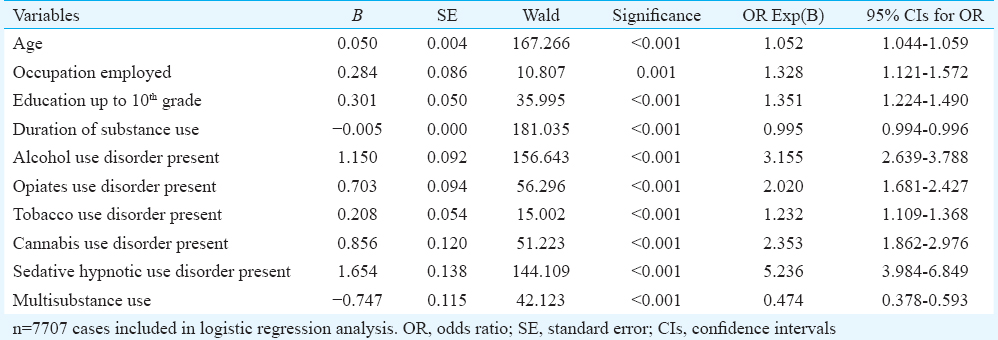
A multivariate logistic analysis with forwards Wald method was conducted to ascertain the independent predictors of initial dropout status. All those variables which showed at least a trend level significance (P<0.2) in the bivariate sample were used for the logistic regression analysis. Since the duration of substance use and duration of dependence showed high degree of collinearity (r=0.858, P<0.001), only the duration of substance use was entered into the regression equation. The variables found to significantly predict the initial dropout status are summarized in Table II. The model could correctly explain 64.3 per cent of the cases, and the Nagelkerke R2 value was 0.110. Multivariable analysis revealed that after controlling for other factors, greater age, being employed, lower educational status, lesser duration of substance use, use of alcohol, opiate, tobacco, cannabis or sedative-hypnotic use but the absence of multi-substance use predicted initial dropout.
Discussion
The present study suggests that 61 per cent of the patients registering to an outpatient substance use disorder programme drop out within the first month. The figure is marginally higher than that of a similarly conducted study (57%)6, which included 480 randomly selected patients over a period of eight years. The previous study6 predominantly consisted of patients with cocaine dependence and had excluded mental retardation, psychosis or organic mental disorder, the present study had a maximum proportion of opioid dependence and included all consecutive patients into the analysis. Another study23 conducted in the US in an addiction treatment centre, which was retrospective chart review showed an attrition rate as high as 80 per cent. However, this rate includes attrition between treatment request and assessment and assessment and treatment enrollment23. Although there is no definitive cut-off for determining treatment retention status, in our study one month was taken as the criterion to define dropout as treatment non-retention has been reported to be high during this period78. The first month of treatment has been suggested to be the critical period for establishing treatment engagement, therapeutic alliance and motivation enhancement24. We attempted to strike a balance between choosing too short duration and thus increasing the possibility of ‘false positive’ labelling of dropout and considering too long duration thus increasing the probability of not including patients who actually had dropped out initially.
The socio-demographic variables associated with treatment dropout vary across the studies. As per finding of this study, age, employment status and levels of education were significant factors affecting the treatment outcome. Younger mean age at treatment seeking was found to be associated with better treatment retention. Explaining this association in isolation would be difficult and speculative. It is likely to be mediated by other factors which have not been investigated in the present study like severity of the substance use and better therapeutic relationship25. Results of previous studies regarding age and treatment retention are mixed. Studies conducted in the residential settings found the older age to be associated with better treatment retention911. However, other studies conducted in outpatient facilities did not find differences in retention with respect to age111326. Higher employment status and lower education predicted poor treatment retention in our study. The association remained significant even after the logistic regression, implying that these two socio-demographic parameters were independently related to treatment retention. While one study revealed that Caucasian race, male gender and higher employment status together predicted higher treatment retention, another study showed that higher employment score was associated with lower rate of treatment completion2728. The higher levels of education being a predictor of treatment retention is congruent to the existing literature101329. One study has demonstrated positive effect of familism (a social construct where family's needs take precedence over an individual member of the family) on treatment retention and engagement. The current study did not look into the particular construct, future research should focus on that because of its relevance in the current changing social scenario of India30. Studies examining gender differences in substance abuse treatment retention found inconsistent results with some showing no gender differences in treatment retention112628 while others show women to more commonly drop out1328 and still others show men to drop out more frequently73031. The low number of women in our study made the interpretations difficult. The lower percentage of females presenting for drug de-addiction treatment has also been reported in the literature323334. The present study also showed a trend towards lower retention rate with increasing distance of patient's place of residence from the Centre. However, distance did not come up as one of the important predictors for treatment dropout in the multivariate analysis. This finding was in contrast with the previous literature demonstrating a significant association between the distance travelled for outpatient treatment and client retention35, higher retention with lower distance to be travelled. This variation might be explained by the difference in cut-off used for the distance travelled. As the cut-off was arbitrary, continuous variable instead of an ordinal one regarding the distance could have been more useful.
Among the clinical variables, there were significant differences in the presence of alcohol use, opioid use, cannabis use, sedative-hypnotic use and multiple substance use disorders (>1 substance excluding tobacco) between the two groups. Multivariate logistic analysis also showed that presence of alcohol, opiates, cannabis and sedative-hypnotic use disorders was independent predictors of treatment retention i.e. single substance use disorder diagnosis was related to poor treatment retention. This could be due to the high attrition rate in the present sample. Beynon et al36 found that the odds of dropout were significantly lower among opiate and alcohol users. Veach et al37 also found that alcohol use disorder was indicated in treatment retention. However, the role of alcohol consumption in treatment dropout was also documented by one study conducted on a sample of 102 cocaine-addicted patients38. However, another outpatient based study did not find any association between treatment retention and type of substance use disorder26. Moreover, not only for alcohol and opioids but benzodiazepine use was also associated with a complex clinical picture. One study showed that it might negatively influence treatment outcomes and had no association with retention39, other showed that baseline benzodiazepine use correlated with lower retention rates but not with poorer outcome40. A study on benzodiazepine use (prescription use/misuse) did not find any association with treatment retention rate41. An interesting finding of the current study was the inverse association of polysubstance use and treatment attrition. The speculative reason could be higher clinician's involvement and attention in those with more than two substance use disorders. Many of earlier studies were on patients who were on agonist maintenance programme for opioid dependence, while the patients in our study represented a heterogeneous mix of substance users.
Limitations of the study included the computation being based on available medical records. A restricted number of relevant variables could be analyzed. Some of the factors which could be related to dropouts, for example, motivation at the intake point, additional psychiatric disorders and medical illnesses were not assessed as a part of the study due to nature of records and coding procedures. The treatment details provided to the patients were not included in the coding. Hence, it would not be possible to make any comments regarding whether and how initial treatment might predict retention. One example of this was the unavailability of BNX detoxification during about half of the study period when opioid detoxification was exclusively done by clonidine. This might have affected the treatment retention in opioid-dependent subjects. Duration of use of each of the individual substances was not available. Many of the variables included in the current study might be correlated with those not included and hence could lead to erroneously significant association with the retention. This could have been picked up on analysis while exploring co-linearity. However, these variables were not assessed in the present study. Only a limited number of women could be registered during the study period (<1% of the total sample). This however, reflects the characteristics of the patients attending the de-addiction services in the region32. Social stigma, dependence on others in the family for treatment seeking, and lack of gender-sensitive treatment programme could be postulated as causes of very low treatment seeking of women with addiction in our study. For initial dropout the cut-off was fixed at 30 days. Although this threshold was based on rationale and existing evidence, one might question whether this represented the actual treatment attrition. This study did not attempt to find out the reasons of dropout from the patients who did not follow up within 30 days. However, such an enquiry subsequently would help in ascertaining the patient's perspectives of the reasons of dropping out of treatment.
In conclusion, certain demographic and clinical variables measured at the intake point were found to be associated with an increased risk for dropout. Rates of retention can be improved by better understanding of factors associated with premature dropout. One important advantage to identifying individuals at risk for early dropout may be to effectively triage and target the high risk individuals. In our study, patients with single substance use disorder, older age, employed, with lower education and using substance for lesser duration of time were observed to be high risk for treatment attrition. It has been suggested that rather than attempting to prevent dropout, service providers could instead offer shorter-term interventions better suited to a dropout population. This approach named as ‘treatment-fit’ would ensure that the patient receives an intervention optimally suited to their attendance duration38. This could reduce resource-related costs in the treatment process in a resource constraint country like India.
Conflicts of Interest: None.
References
- Participation in treatment and Alcoholics Anonymous: A 16-year follow-up of initially untreated individuals. J Clin Psychol. 2006;62:735-50.
- [Google Scholar]
- Specialty mental health care improves patients’ outcomes: Findings from a nationwide program to monitor the quality of care for patients with substance use disorders. J Stud Alcohol. 2000;61:704-13.
- [Google Scholar]
- Retention in psychosocial treatment of cocaine dependence: Predictors and impact on outcome. Am J Addict. 2002;11:24-40.
- [Google Scholar]
- Responding to treatment dropout: A review of controlled trials and suggested future directions. Addict Res Theory. 2010;18:298-315.
- [Google Scholar]
- Predictors of being expelled from and dropping out of alcohol treatment. Psychiatr Serv. 1998;49:187-9.
- [Google Scholar]
- Factors associated with immediate dropout of outpatient treatment for drug abuse in Rio de Janeiro. Soc Psychiatry Psychiatr Epidemiol. 2000;35:513-7.
- [Google Scholar]
- Dropping out of substance abuse treatment: A clinically oriented review. Clin Psychol Rev. 1992;12:93-116.
- [Google Scholar]
- The role of the early therapeutic alliance in predicting drug treatment dropout. Drug Alcohol Depend. 2006;83:57-64.
- [Google Scholar]
- Addiction treatment dropout: Exploring patients’ characteristics. Am J Addict. 2012;21:78-85.
- [Google Scholar]
- Pretreatment and during treatment risk factors for dropout among patients with substance use disorders. Addict Behav. 2006;31:450-60.
- [Google Scholar]
- Client-related predictors of early treatment drop-out in a substance abuse clinic exclusively employing individual therapy. J Subst Abuse Treat. 2004;26:189-95.
- [Google Scholar]
- Patient factors related to early attrition from an outpatient cocaine research clinic. Am J Drug Alcohol Abuse. 1996;22:29-39.
- [Google Scholar]
- Correlates of outpatient drug treatment drop-out among methamphetamine users. J Psychoactive Drugs. 2000;32:221-8.
- [Google Scholar]
- Unplanned versus planned discharges from in-patient alcohol detoxification: Retrospective analysis of 470 first-episode admissions. Alcohol Alcohol. 2002;37:277-81.
- [Google Scholar]
- Coping among individuals seeking private chemical dependence treatment: Gender differences and impact on length of stay in treatment. Alcohol Clin Exp Res. 2002;26:1228-33.
- [Google Scholar]
- A comparative study of cocaine-treatment completers and dropouts. J Subst Abuse Treat. 1999;16:17-22.
- [Google Scholar]
- Predictors of inpatient treatment completion of subjects with heroin dependence. Indian J Psychiatry. 1997;39:282-7.
- [Google Scholar]
- Non completers of opiate detoxification program. Indian J Psychiatry. 1992;34:376-9.
- [Google Scholar]
- American Psychiatric Association. DSM-IV-TR: Diagnostic and statistical manual of mental disorders, text revision. Washington, DC: American Psychiatric Association; 2000.
- [Google Scholar]
- Examining attrition rates at one specialty addiction treatment provider in the United States: A case study using a retrospective chart review. Subst Abuse Treat Prev Policy. 2014;9:41.
- [Google Scholar]
- Therapeutic alliance as a predictor of outcome and retention in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. J Consult Clin Psychol. 2001;69:119-24.
- [Google Scholar]
- Drug abuse treatment process components that improve retention. J Subst Abuse Treat. 1997;14:565-72.
- [Google Scholar]
- Reasons for dropout from drug abuse treatment: Symptoms, personality, and motivation. Addict Behav. 2006;31:320-30.
- [Google Scholar]
- Predictors of outpatient treatment retention: Patient versus substance use characteristics. Drug Alcohol Depend. 2001;62:9-17.
- [Google Scholar]
- Gender differences in predictors of initiation, retention, and completion in an HMO-based substance abuse treatment program. J Subst Abuse Treat. 2002;23:285-95.
- [Google Scholar]
- Predictors of attrition in a longitudinal study of substance abusers. J Psychoactive Drugs. 2002;34:69-74.
- [Google Scholar]
- The influence of cultural variables on treatment retention and engagement in a sample of Mexican American adolescent males with substance use disorders. Psychol Addict Behav. 2015;29:969-77.
- [Google Scholar]
- Determining predictors of attrition in an outpatient substance abuse program. Am J Drug Alcohol Abuse. 2002;28:55-72.
- [Google Scholar]
- Gender differences in treatment outcomes over a three-year period: A PATH model analysis. J Drug Issues. 2004;34:419-39.
- [Google Scholar]
- Changing pattern of substance abuse in patients attending a de-addiction centre in North India (1978-2008) Indian J Med Res. 2012;135:830-6.
- [Google Scholar]
- Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug Alcohol Depend. 2007;86:1-21.
- [Google Scholar]
- Distance traveled to outpatient drug treatment and client retention. J Subst Abuse Treat. 2003;25:279-85.
- [Google Scholar]
- Factors predicting drop out from, and retention in, specialist drug treatment services: A case control study in the North West of England. BMC Public Health. 2008;8:149.
- [Google Scholar]
- Retention predictors related to intensive outpatient programs for substance use disorders. Am J Drug Alcohol Abuse. 2000;26:417-28.
- [Google Scholar]
- Comparison of completers and dropouts in psychological treatment for cocaine addiction. Addict Res Theory. 2010;18:433-41.
- [Google Scholar]
- The impact of benzodiazepine use on methadone maintenance treatment outcomes. J Addict Dis. 2008;27:37-48.
- [Google Scholar]
- Benzodiazepine use among patients in heroin-assisted vs.methadone maintenance treatment: Findings of the German randomized controlled trial. Drug Alcohol Depend. 2010;112:226-33.
- [Google Scholar]
- Benzodiazepine use during buprenorphine treatment for opioid dependence: Clinical and safety outcomes. Drug Alcohol Depend. 2013;132:580-6.
- [Google Scholar]






