Translate this page into:
Hughes syndrome with cerebral, skeletal infarction & retinal vein thrombosis
*For correspondence: ssundaram@aims.amrita.edu
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 23-year old female patient presented to the General Medicine and Nuclear Medicine departments of Amrita Institute of Medical Sciences, Cochin, Kerala, India in March 2013 with fever, joint pains for six months duration with thrombocytopenia. Immunologically she was tested positive for systemic lupus erythematosis (SLE). A Technetium 99m (Tc 99m)-methylene diphosphonate (MDP) bone scan was advised. Images revealed unsuspected cold defects in D6 and L4 vertebral bodies raising the suspicion of bone infarcts versus marrow metastatic infiltration. The patient showed no evidence of polyarthritis. However, there was evidence for left frontal lobe acute infarction on the MRI (magnetic resonance imaging) (Fig. 1). Whole body (methoxy-iso butyl-isonitrile) MIBI oncoscintigraphy (Figs 2 and 3) was suggested to re-assess the above bone scan findings. The patient developed sudden onset painless diminution of vision two weeks later. Ophthalmological examination revealed retinal vein thrombosis on right side.

- MRI of brain shows features of acute infarct in left frontal lobe (arrow).

- Whole body MIBI oncoscintigraphy and 99mTc MDP whole body skeletal scintigraphy showed cold defects in D6 and L4 vertebral bodies confirming scintigraphic diagnosis of bone infarcts.
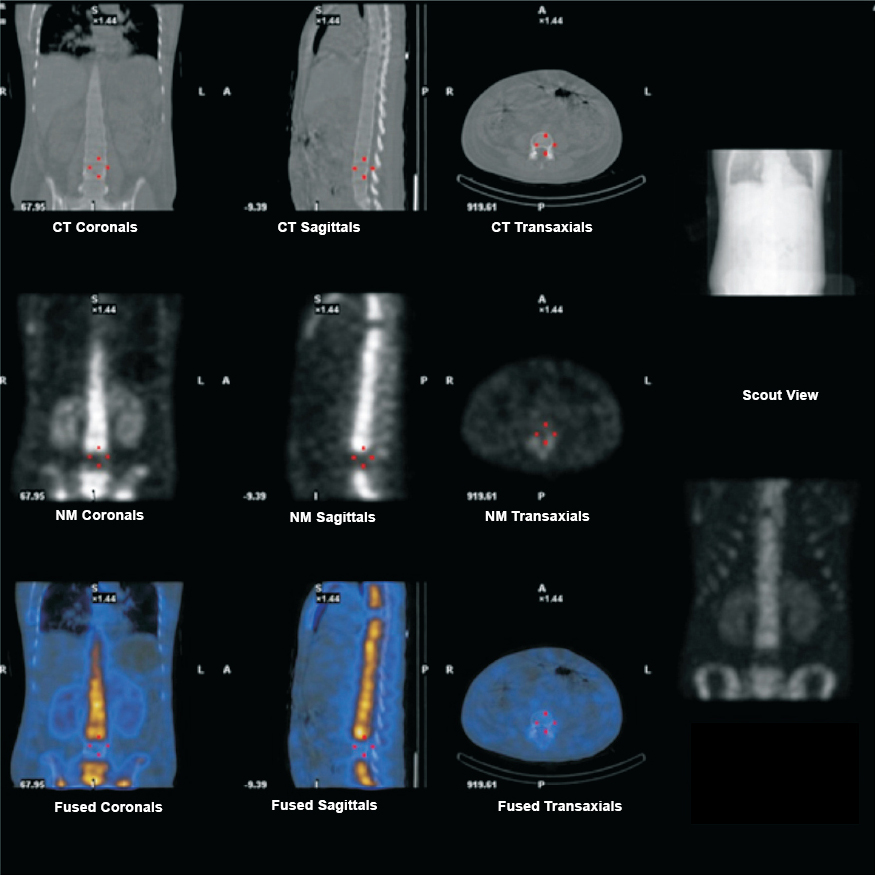
- 99mTC MDP bone SPECT CT (single photon emission computed tomography - computed tomography) images of dorsolumbar vertebrae showing cold defects in D6 and L4 vertebral bodies.
The patient had persistent severe thrombocytopenia to the tune of 15,000 per microliter and elevated serum creatinine of 1.3 mg/dl. The possibilities considered were severe lupus activity with relapse, thrombotic thrombocytopenic purpura (TTP) or severe antiphospholipid antibody syndrome. To rule out TTP, lactate dehydrogenase level was measured which was elevated, but peripheral smear was non contributory ruling out the diagnosis of TTP. She was given three pulses of high-dose steroid despite further deterioration in her platelet counts. Her anticardiolipin antibody titres were positive on two occasions 12 wk apart to the titre of 25-30 MPL units confirming the diagnosis of Hughes syndrome rather than SLE induced bone infarction. The patient was started on intravenous (iv) Heparin (1000 units per hour), titrated based on activated partial thromboplastin time (APTT) values with which she started responding. Platelet counts also stabilized. The patient was doing well at two months follow up.





