Translate this page into:
High frequency of young age rectal cancer in a tertiary care centre of southern Assam, North East India
*For correspondence: drsankarghosh@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Colorectal cancer (CRC) is the third most common cancer in men and the second in women worldwide12, with significant geographical, racial and ethnic variation in its incidence rate and pattern34. Globally, cancer of rectum and anus constitutes more than 40 per cent of the CRC cases, and its incidence peaks between the age of 60 and 70 yr, while its occurrence in patients below 40 years is rare5.
The incidence of rectal cancer in India is lower than that in the western countries, and it is the tenth leading cancer in India6. Several individual studies on Indian and Bangladeshi patients have consistently documented a relatively high proportion of young age rectal cancer (RC), with a mean age of around 40-45 yr78910. Interestingly, many of the reports on young age RC or CRC in India came from West Bengal, a State in the eastern region of India89. Both Bangladesh and West Bengal are situated in the northeast region of the Indian Subcontinent, and share similar ethnic, linguistic, dietary, cultural and social characteristics.
We examined the frequency and clinicopathological characteristics of RC patients in Southern Assam (consisting of three districts: Cachar, Karimganj and Hailakandi) in a hospital based study. Our objective was to investigate if any discrepancy regarding rectal cancer in young patients occurs in this area and also to identify the associated clinicopathological features.
All patients diagnosed with rectal carcinoma at Cachar Cancer Hospital and Research Centre (CCHRC) from January 2008 to December 2011 were included in the study. This institute is a speciality oncology centre in Cachar district, which happens to be the only oncology centre serving the entire population of Southern Assam. Demographic as well as clinicopathological data of the RC patients were collected in two phases: retrospectively, for 106 cases from the hospital registry records from 2008-2010 and 38 newly diagnosed and histologically confirmed cases were included prospectively from January to December 2011. The study protocol was approved by the ethical committee of the hospital and written consent was taken from all the prospectively enrolled patients. The patients were divided into two groups; a younger group of below 40 years of age and an older group of 40 years and above. Patient data included age, sex, ethnicity, tumour morphology, tumour stage and differentiation, carcinoembryonic antigen (CEA) levels at presentation, etc.
Tumour involvements within 15 cm from the anal verge by rectal examination, colonoscopy or MRI were considered. Tumours 0.1 - 5 cm from the anal verge were classified as low rectal tumours and all resected tumours were staged according to Union for International Cancer Control (UICC) (Tumor, Node, Metastasis) TNM classification11. However, no patients had past history of colonic or rectal polyps or any other malignancy and most of the patients either did not have or did not disclose any family history of cancer.
Two tailed χ2 test or Fisher exact test was used to test the sgnificance of all categorical data and students t test for continuous data.
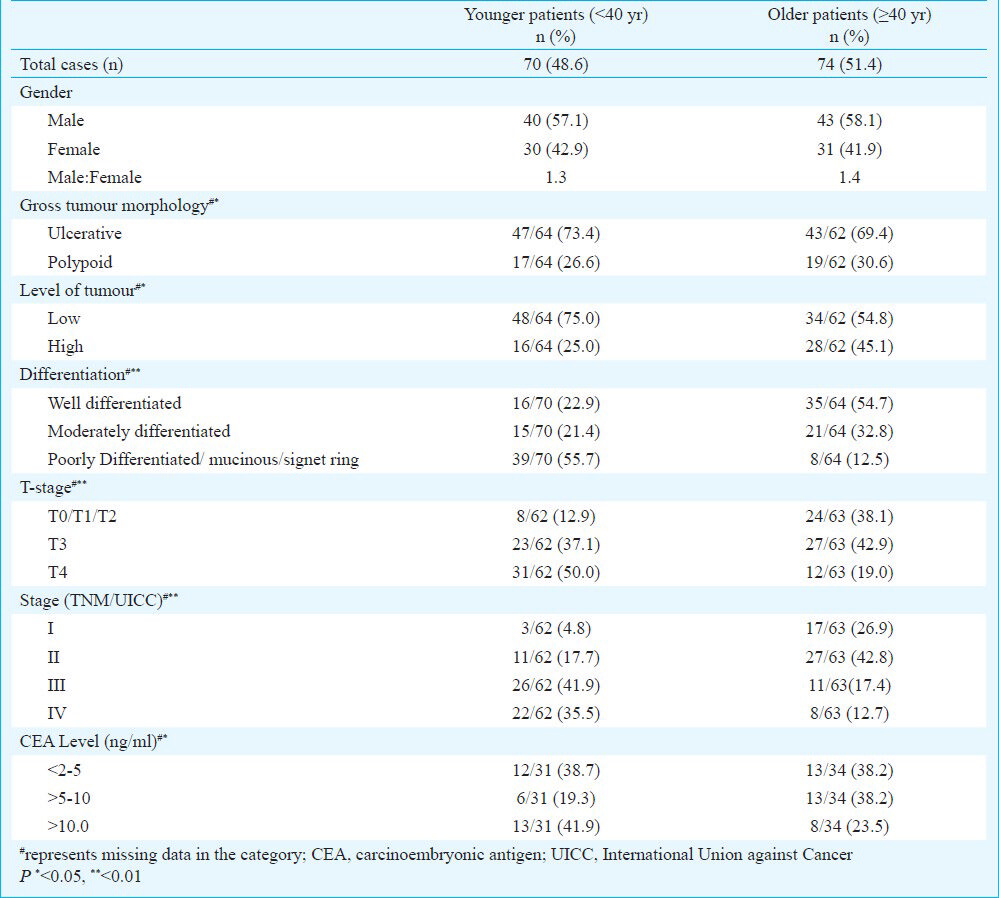
Among all the 144 patients under study, 70 (48.61%) were below 40 years and 74 (51.39%) were ≥40 yr of age. The mean age at presentation was 43. 4 ± 15.8 yr, the youngest patient was 14 years old. More than 80 per cent of the patients were Bengali, 7-10 per cent were Manipuri and the rest belonged to various other tribal and non-tribal groups. Of the 144 patients, 142 were diagnosed with rectal adenocarcinoma, while two patients in the ≥40 yr age group had squamous cell carcinoma. The major clinical presentations were bleeding per rectum, weight loss and anaemia, altered bowel habits, large gut obstruction and abdominal lump. The tumour characteristics of younger and older patients are summarized in Table I. The younger patients had predominance of low rectal tumours, advanced T-stage, poor differentiation with mucinous and signet ring and an advanced disease stage as compared to the older patients.
In this study, about 48 per cent of young age (below 40 yr) rectal cancer was observed, with distinct clinical and pathological characteristics. Highest proportion of RC patients was observed in the age group of 30-39 (28.4%), followed by the 50-59 age group (19.4%). As such, along the age groups of 10 yr interval from 0-70+ yr, two distinct peaks in percentage were observed and the proportion of patients decreased in the subsequent age groups (Table II). Corresponding figures of rectal cancers, along with mean age and standard deviation from the major hospital based cancer registries (HBCRs) of India (2004-2006) viz. Mumbai, Chennai, Banglore, Dibrugarh and Thiruvanathapuram and also the population base cancer registries (PBCRs) in India (2006-2008) viz, Bangalore Mumbai, Delhi, Chennai, Kolkata and the major PBCRs of North-east India viz, Kamrup, Dibrugarh, Mizoram and Manipur are shown in Table II612. The mean age of the patients reporting to our hospital was significantly lower (P<0.001) as compared to the overall mean age of patients reported in all the HBCRs (mean age 50.4 ± 15.1 yr) and PBCRs (mean age 54.65 ± 15.5 yr). The peak observed in the age group of 30-39 in our hospital was also significantly higher (P<0.001) than all the compared registries and was consistent for all the age group between 10-39 yr (P<0.001 for 10-19 yr, P=0.02 for 20-29 yr as compared to HBCRs and P=0.001 for both groups as compared to PBCRs). The overall percentage of patients below 40 yr was significantly higher (P<0.001) in our hospital as compared to the HBCRs and PBCRs including the North-east ones. However, there was no difference in any age group above 40 yr between our hospital, HBCRs and PBCRs, except for a comparatively lesser proportion of patients in above 70 yr group in our hospital.
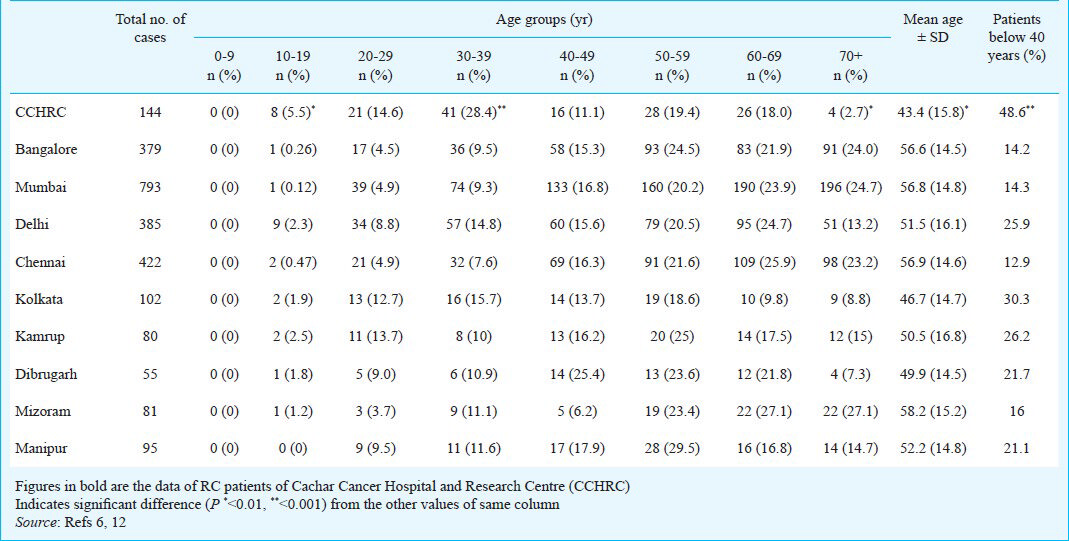
Prior studies conducted in various oncology centres and hospitals have documented a relatively higher proportion (42 to ~48%) of young age RC or CRC in West Bengal compared to the rest of India89. In one study from a tertiary oncology centre in India, a high occurrence of below 40 yr RC was reported (~35%) and 39% of the study group comprised patients from West Bengal7. As West Bengal, Bangladesh and the population of Southern Assam share similar geographic, dietary and ethnic characteristics, comparable genetic susceptibility and disease characteristics are also likely.
Worldwide, studies on colorectal cancer have documented distinct differences in disease characteristics of younger and older patients in terms of stage, grade, location of tumours and survival. The younger patients present with a more aggressive disease, are advanced in stage with unfavourable histopathological findings (mucinous and signet ring cells)1314151617. Our study and also studies from other hospitals in West Bengal have documented similar findings for younger patient79. This might be as a result of distinct molecular signatures of the younger and older patients, the younger patients being more likely to have microsatellite instability (MSI) related changes indicating towards familial predisposition like hereditary non-polyposis colorectal cancer (HNPCC)14. In many of the reports on young age CRC from the developed countries, a positive family history was observed in 25-35 per cent of the patients131617. However, in most of the studies on Indian and Bangladeshi patients and also in the patients of our population a positive family history was very rare (<1%), if at all reported6789. In one study conducted in UK10, distinct differences were observed between gene expression profiles of Bangladeshi CRC patients (61% below 40 yr) and their western counterparts. However the MSI status was similar for both the groups (16% vs. 15% MSI positive)10. This triggers a suspicion of underlying genetic factors associated with RC at a younger age in this population, which might be different from the already known familial cancer of large bowel like HNPCC or familial adenomatous polyposis (FAP). Further, the role of non-environmental factors is indicated by the fact that incidence of CRC in Indians and Bangladeshis migrated to western countries is much lower than the local population18.
In conclusion, the current study has documented a high proportion of young age rectal cancer in a hospital based study from Southern Assam and identified distinct clinicopathological differences with the older patients. As there are no routine screening programmes available for RC in this area, clinicians should give more emphasis on rectal examination by sigmodoscopy or colonoscopy in younger patients with rectal symptoms. Detailed epidemiological and molecular studies need to be done to identify the aetiology of young age rectal cancer in this region.
References
- GLOBOCAN 2008. Cancer Incidence and Mortality Worldwide. 2010. Lyon, France: International Agency for Research on Cancer; Available from: http://globocan.iarc.fr
- [Google Scholar]
- Cancer incidence in five continents, vol. IX. IARC Scientific Publication No. 160. Lyon, France: International Agency for Research on Cancer; 2007.
- [Google Scholar]
- International trends in colorectal cancer incidence rates. Cancer Epidemiol Biomarkers Prev. 2009;18:1688-94.
- [Google Scholar]
- Racial differences in the incidence of colorectal cancer. Can J Gastroenterol. 2010;2:47-51.
- [Google Scholar]
- Three-years report of Population Based Cancer Registries 2006-2008 (Detailed Tabulations of Individual Registries Data). National Cancer Registry Programme (Indian Council of Medical Research), Bangalore November. 2010. Available from: http://www.PBCR_2006_2008.aspx
- [Google Scholar]
- Rectal cancer in young adults: a series of 102 patients at a tertiary care centre in India. Colorectal Dis. 2009;11:475-9.
- [Google Scholar]
- Proportionate increase in incidence of colorectal cancer at an age below 40 years: an observation. J Cancer Res Ther. 2006;2:97-9.
- [Google Scholar]
- Colorectal carcinoma in young adults: a retrospective study on Indian patients: 2000-2008. Colorectal Dis. 2010;12:e182-9.
- [Google Scholar]
- Microarray profiling of colorectal cancer in Bangladeshi patients. Colorectal Dis. 2005;7:571-5.
- [Google Scholar]
- TNM classification of malignant tumors, fifth edition (1997) Cancer. 1997;80:1803-4.
- [Google Scholar]
- Consolidated Report of Hospital Based Cancer Registries 2004-2006 (Detailed Tabulations of Individual Registries Data) 2009. Bangalore: National Cancer Registry Programme (Indian Council of Medical Research); Available from: http://ncrpindia.org/HBLR_2004_2006/Preliminary_Pages_HBCR_Report_2004_06.pdf
- [Google Scholar]
- Young patients with colorectal cancer: how do they fare? ANZ J Surg. 2001;71:707-10.
- [Google Scholar]
- Clinicopathological and molecular biological features of colorectal cancer in patients less than 40 years of age. Br J Surg. 2003;90:205-14.
- [Google Scholar]
- The impact of young age on cancer-specific and non-cancer-related survival after surgery for colorectal cancer: 10-year follow-up. Br J Cancer. 2009;101:557-60.
- [Google Scholar]
- Clinicopathological features of colorectal cancer in patients under 40 years of age. Int J Colorectal Dis. 2010;25:823-8.
- [Google Scholar]
- Presentation and outcomes of patients aged 30 years and younger with colorectal cancer: a 20-year retrospective review. Med Oncol. 2011;28:1058-61.
- [Google Scholar]
- Cancer incidence in the south Asian population of England (1990-92) Br J Cancer. 1999;79:645-54.
- [Google Scholar]





