Translate this page into:
Effect of structured counselling on postpartum contraceptive acceptance: A cluster randomized controlled trial, Puducherry
For correspondence: Dr Venkatachalam Jayaseelan, Department of Preventive and Social Medicine, JIPMER International School of Public Health (JISPH), Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry 605 006, India e-mail: drvenkatpgi@gmail.com
-
Received: ,
Accepted: ,
Abstract
Background & objectives
As per District Level Household Survey-III, there are 44 million people with unmet contraceptive needs in India. Contraception uptake in postpartum is around 17 per cent within six months and 33 per cent within six to 12 months post-delivery. Through our study, we aimed to access the effectiveness of a structured counselling session on acceptance of postpartum contraception within six wk after delivery among third-trimester pregnant women in Puducherry.
Methods
A randomised controlled trial was conducted among 236 third-trimester antenatal women receiving care from four selected primary health centres in Puducherry between March 2023 and February 2024. Antenatal women undergoing intervention received a structured counselling session with audio-visual aid along with a health education booklet & controls received standard care. They were followed up six wk postpartum. The chi-square test was used to compare the effectiveness of intervention, and P<0.05 was considered significant. Relative risk with a 95 per cent confidence interval was calculated to measure the strength of association.
Results
Among 221 (93.6%) participants who completed the study, 78 (66.7%) out of 117 in the intervention arm and 25 (21%) out of 119 in the control arm accepted any contraceptive method at six wk postpartum. The contraceptive acceptance was significantly higher in the intervention arm, with a three-fold increase compared to the control arm [RR: 3.21 95% confidence interval (CI): 2.22-4.61; P<0.001]. Additionally, there was a significant improvement in knowledge levels among mothers in the intervention group.
Interpretation & conclusions
The findings demonstrate that the structured counselling sessions with audiovisual aids and educational materials enhanced postpartum contraceptive uptake and improved knowledge levels among mothers. Our intervention has the potential for broader implementation in routine maternal health services and would improve postpartum contraceptive acceptance at the national level.
Keywords
Contraception
contraceptive knowledge
pregnancy
Puducherry
structured counselling
The human population has transformed throughout history, with concerns about overpopulation or under population arising during each demographic shift. Now exceeding eight billion, the global population faces challenges like ensuring adequate food and healthcare1. This growth underscores the importance of family planning. Achieving sexual and reproductive health and rights is crucial for promoting gender equality, dignity, and opportunities. Alarmingly, over 40 per cent of women worldwide lack the power to decide on whether to have children. Empowering women through education and access to contraception allows them to make informed choices and achieve their goals2.
India accounts for 20 per cent of couples with unmet contraceptive needs and 17.3 per cent of protected couples globally3. The postpartum family planning acceptance rate is around 30 per cent4. According to District Level Health Survey III data, India has 44 million unmet contraceptive needs, with 16.3 million for spacing and 25.5 million for limiting5. Postpartum contraceptive use is below 17 per cent within six months and about 33 per cent between six and twelve months after delivery, highlighting the need for postpartum contraception for reproductive autonomy6. Maternal mortality has been reduced by 40 per cent worldwide, but efficient contraception use in underdeveloped nations could reduce it by an additional 30 per cent7.The strain on maternal health resources and the increased likelihood of complications during subsequent pregnancies significantly contribute to maternal mortality. Understanding how postpartum contraception prevents unintended pregnancies and lowers maternal health risks is key to addressing this issue.
As women navigate the third trimester, they focus on preparing for the postpartum period. Counselling during this receptive time can help prevent unwanted pregnancies. Providing a range of postpartum contraceptive options tailored to individual needs empowers women to make informed choices. An interventional study in Uganda found that prenatal counselling had no impact on postpartum contraceptive use8, while a study in Mumbai showed that counselling increased knowledge to 92.25 per cent9. Most studies have focused on assessing improvements in knowledge, while very few have evaluated the actual uptake of postpartum contraception following counselling. To enhance the adoption of postpartum contraception, there is a need for structured counselling sessions. Additionally, there is a paucity of randomized controlled trials (RCTs) in the Indian context that specifically examine the acceptance of peripartum contraception, particularly the insertion of copper-T post-delivery. Our study evaluated the effectiveness of structured counselling on postpartum contraception acceptance within six wk after delivery among third-trimester pregnant women in Puducherry.
Materials & Methods
This randomised control trial was conducted by the departments of Preventive and Social Medicine and Obstetrics and Gynaecology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, after obtaining the ethical approval from the Institute Ethics Committee. The trial was registered with the Clinical Trial Registry of India (CTRI/2024/01/061854) before commencement of the study.
This cluster RCT was conducted in Puducherry, India, from March 2023 to February 2024, involving third-trimester pregnant women. Puducherry, a Union Territory comprising four enclaves, has a population of 1.244 million (2011 census), with 68 per cent urban residency, a sex ratio of 1112 women per 1000 men, and high literacy rates (NFHS-5 data)10. The territory boasts a comprehensive healthcare network. Four primary health centres (PHCs) out of 32 were purposively selected based on feasibility, representing both urban2 and rural2 settings. Each PHC service area was designated as a distinct cluster for the trial. An independent researcher randomized the selected PHCs into intervention and control groups using the lottery method, ensuring unbiased allocation for the study.
After getting informed consent from participants, basic sociodemographic details, reproductive details, knowledge, previous practice and current acceptance of postpartum contraception were collected in both groups.
The intervention comprised a one-hour structured counselling session conducted in the third trimester for groups of 15-20 women. Before initiating the counselling, baseline sociodemographic and reproductive characteristics were collected, and participants’ knowledge about postpartum contraception was assessed using a validated, self-administered, and semi-structured questionnaire with outcomes categorised as binary variables. This comprehensive session covered several key aspects of postpartum health and contraception. Participants received education on the risk of early pregnancy after childbirth, a detailed overview of available contraceptive options, and the benefits, potential side effects, and contraindications of each method. The counselling also included instructions for follow-up care and emphasised the importance of nutrition during both antenatal and postnatal periods. The session addressed rest requirements during pregnancy; danger signals to be aware of, and postpartum care and hygiene practices. Audio-visual aids supplemented the oral presentation, and participants received health information booklets for future reference. This booklet, originally developed in English based on a literature review and expert input, was translated into Tamil and back-translated to ensure accuracy. The participants in the control arm received standard care, which consisted of routine advice provided by healthcare practitioners. Pilot testing was conducted with six pregnant women not involved in the RCT. At the six-wk postpartum follow up, we conducted an endline assessment to evaluate contraceptive initiation among the selected participants. We re-evaluated post-counselling knowledge using a semi-structured questionnaire. For participants who had returned to their maternal homes post-delivery, as per local custom, we conducted follow ups via mobile phone calls. To ensure data authenticity, we verified photographs of case sheets for intervention participants who had undergone surgical contraceptive procedures. In cases of non-compliance, we inquired about and documented the reasons.
Statistical analysis
Using experts’ opinion, assuming unexposed with an outcome of 30 per cent, exposed with an outcome of 50 per cent, absolute precision of five per cent, power 80 per cent, and the ratio of intervention: control as one, using OpenEpi version 3.03, the initial estimate of sample size was 208 and on applying 10 per cent loss to follow up and design effect of 1.3, the total final sample size was 302 with a cluster size of 76.
Data entry was done using the Epicollect software, and the data was exported directly from Epicollect to the Excel spreadsheet followed by data cleaning and coding. Categorical variables like gender, residence, family type, socio-economic status, educational status, history of abortion, and presence of relevant comorbidities were expressed as frequencies with proportions with 95% confidence interval (CI). We recorded continuous variables like age, order of pregnancy, and number of previous pregnancies into categorical variables and expressed them as proportions with 95% CI. Chi-square test at end-line for two groups using IBM SPSS v 23.0. Statistical significance was determined by reporting relative risk with 95% CI and P value of 0.05. Knowledge and awareness of contraception were assessed in both groups, along with improvements in knowledge following the intervention. The McNemar test was used to evaluate the within-group impact of counselling on contraceptive acceptance rates. Effect sizes were calculated using Cohen’s h, with a corresponding 95% CI, to quantify the magnitude of the observed effects.
Results
An interim analysis revealed significant inter-group differences, leading to early recruitment cessation. Of the 302 planned participants, 236 were enrolled, with 117 assigned to the intervention arm and 119 to the control arm. An attrition rate of 6.35 per cent (15 participants; 8 in the intervention and 7 in the control) was observed. The final analysis was conducted according to the intention-to-treat principle.
Figure 1 depicts the number of participants approached, excluded, recruited and followed up at various stages in both groups according to the consort flow diagram. From tables I and II, it can be observed that there was no significant difference between the socio-demographic and reproductive characteristics between the participants in both groups and they were comparable.
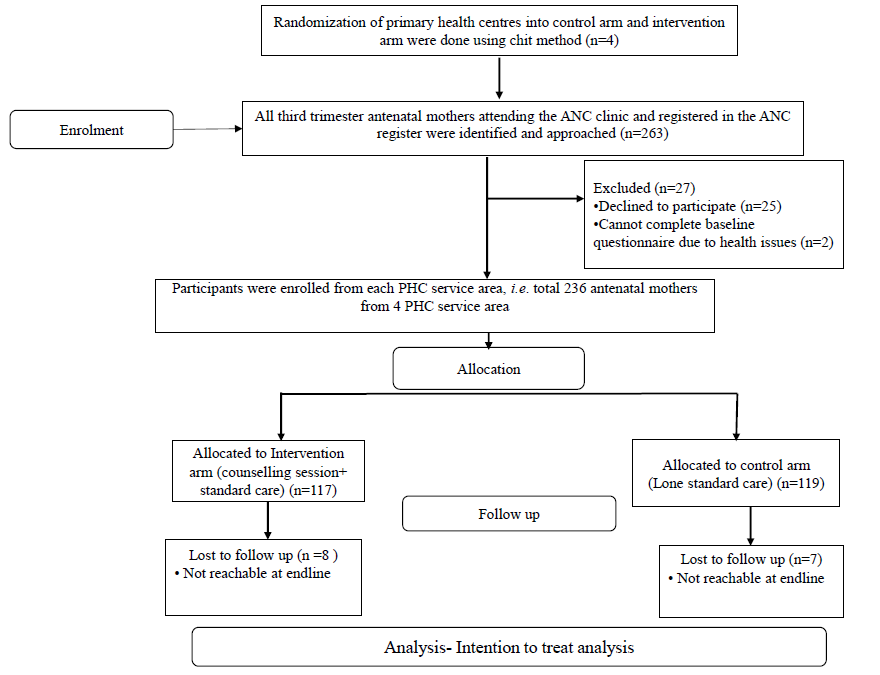
- CONSORT flow diagram showing the number of participants at each stage. ANC, antenatal care; PHC, primary health centre.
| Variable | Intervention group, n (%) | Control group, n (%) | P value* |
|---|---|---|---|
| Age groups of females (yr) | |||
| ≤28 | 74 (63.2) | 77 (64.7) | 0.89 |
| >28 | 43 (36.8) | 42 (35.3) | |
| Education status of females | |||
| Less than primary | 10 (8.5) | 14 (11.8) | 0.52 |
| More than primary | 107 (91.5) | 105 (88.2) | |
| Educational status of spouse | |||
| Less than primary | 7 (6) | 16 (13.4) | 0.08 |
| More than primary | 110 (94) | 103 (86.6) | |
| Family type | |||
| Nuclear | 36 (30.8) | 46 (38.7) | 0.22 |
| Joint/extended | 81 (69.2) | 73 (61.3) | |
| Religion | |||
| Hindu | 109 (93.2) | 110 (92.4) | 1 |
| Non-Hindu | 8 (6.8) | 9 (7.6) | |
| Occupation of women | |||
| Unemployed | 89 (76.1) | 84 (70.6) | 0.38 |
| Employed | 28 (23.9) | 35 (29.4) | |
| Occupation of spouse | |||
| Employed | 115 (98.3) | 113 (95) | 0.28 |
| Unemployed | 2 (1.7) | 6 (5) | |
| Distance from nearby health facilities | |||
| <5 km | 102 (87.5) | 103 (85.9) | 1 |
| >5 km | 15 (12.8) | 16 (13.4) | |
| Variable |
Intervention group N (117), n (%) |
Control group N (119), n (%) |
P value* |
|---|---|---|---|
| Age of women at marriage (yr) | |||
| ≤28 | 111 (94.9) | 104 (87.4) | 0.06 |
| >28 | 6 (5.1) | 15 (12.6) | |
| History of abortion | |||
| Yes | 42 (35.9) | 29 (24.4) | 0.06 |
| No | 75 (64.1) | 90 (75.6) | |
| Reason for abortion | n (21) | n (20) | |
| Unplanned pregnancy | 2 (9.5) | 4 (20) | 0.08 |
| Complication in pregnancy | 9 (42.9) | 13 (65) | |
| Others | 10 (47.6) | 3 (15) | |
| Presence of comorbidities | |||
| Yes | 20 (17.1) | 31 (26.1) | 0.11 |
| No | 97 (82.9) | 88 (73.9) | |
| No. of living child | |||
| No children | 53 (45.3) | 60 (50.4) | 0.44 |
| ≥1 Child | 64 (54.7) | 59 (49.6) | |
| Parity | |||
| Primipara | 57 (48.7) | 71 (59.7) | 0.09 |
| Multipara | 60 (51.3) | 48 (40.3) | |
From figure 2, it can be visualised the contraception uptake was higher in the intervention arm in all forms of contraception compared to the control arm at six wk postpartum, and the most accepted method was permanent sterilisation in both arms. But on asking the reason for not adopting contraception, the control arm mothers said that they would after six months.
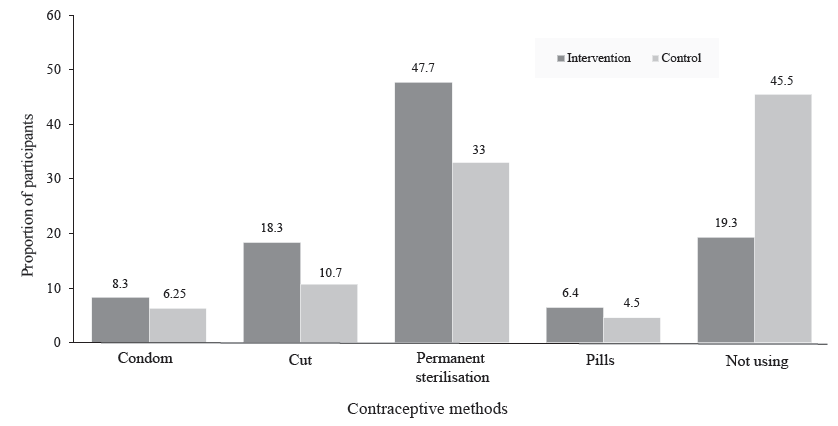
- Bar diagram showing comparison of contraceptive methods accepted across the intervention and control arm.
Table III presents the proportion of participants with acceptance of postpartum contraception after six wk of delivery across the intervention and control arm. In the intervention arm, 78 (66.7%) out of 117 participants, and in the control arm, 25 (21%) out of 119 participants had accepted any contraceptive methods within six wk postpartum. The effectiveness of the structured counselling session showed a three-fold increase in acceptance of contraceptives among mothers who received it compared to mothers who received routine care alone, and the results were statistically significant.
| Variable | Acceptance of postpartum contraception | RR (95% CI) | P value | |
|---|---|---|---|---|
| Yes (%) | No (%) | |||
| Intervention arm (n=109) | 78 (66.7) | 31 (26.5) | 3.21 (2.22 – 4.61) | <0.001* |
| Control arm (n=112) | 25 (21) | 87 (73.1) | ||
Table IV presents significant improvements in postpartum contraception knowledge following structured health education, with the intervention group showing consistently larger effect sizes across most variables when compared to the control group. Key enhancements included substantial gains in various aspects of contraception knowledge, emphasising the effectiveness of the structured educational sessions. However, changes in contraceptive misconceptions were minimal across both groups.
| Variables | Intervention | Control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline n=117, n (%) |
Endline n=109, n (%) |
P value* | Effect size^ | 95%CI |
Baseline n=119, n (%) |
Endline n=109, n (%) |
P value* | Effect size^ | 95%CI | |
| Ideal spacing between pregnancies (yr) | ||||||||||
| >=2 yr | 41 (35) | 93 (79.5) | <0.01 | 1.13 | 0.94-1.33 | 47 (39.5) | 47 (39.5) | <0.01 | 0.13 | -0.15-0.41 |
| Aware about complications of closely spaced pregnancy | ||||||||||
| Aware | 26 (22.2) | 91 (77.8) | <0.01 | 1.32 | 1.14-1.54 | 24 (20.2) | 47 (39.5) | <0.01 | 0.61 | 0.23-0.93 |
| Aware about postpartum contraception | ||||||||||
| Aware | 39 (33.3) | 102 (87.2) | <0.01 | 1.39 | 1.25-1.64 | 42 (35.3) | 63 (52.9) | <0.01 | 0.51 | 0.24-0.78 |
| Side effects of contraceptives | ||||||||||
| Yes | 23 (19.7) | 80 (68.4) | <0.01 | 1.21 | 0.99-1.44 | 27 (22.7) | 52 (43.7) | <0.01 | 0.61 | 0.29-0.92 |
| Misconceptions of contraceptives | ||||||||||
| Yes | 11 (9.4) | 8 (6.8) | <0.45 | -0.07 | -0.42-0.27 | 36 (30.3) | 30 (30.3) | <0.06 | -0.10 | -0.43-0.23 |
| Aware of copper T | ||||||||||
| Aware | 39 (33.3) | 80 (68.4) | <0.01 | 0.82 | 0.67-1.12 | 37 (31.1) | 49 (41.2) | <0.01 | 0.37 | 0.09-0.66 |
Discussion
The acceptance of postpartum contraception after six wk of delivery showed approximately 45 per cent increase in the intervention arm compared to the control arm, which was statistically significant. A similar result was observed in an RCT conducted in Bangkok, Thailand, among 280 mothers with gestational diabetes mellitus, showing 87.1 per cent uptake in the intervention arm compared to 55 per cent in the control arm (Phaloprakarn et al11). This difference in uptake might be due to the resource-limited setting in India compared to Thailand, where health system is well developed. In contrast to our study, an RCT conducted at the Pondicherry Institute of Medical Sciences (PIMS), Puducherry showed no significant difference between the comparison and intervention groups in the acceptance of contraception (Chauhan et al12), and this discrepancy could have stemmed from sociodemographic differences between study populations. Our study, conducted in a public healthcare setting with free services, likely included lower-income participants compared to PIMS, potentially influencing the intervention’s differential impact on contraception acceptance.
A study by Odelola et al13 found that the intervention group had higher uptake compared to the control, but the difference disappeared when accounting for other factors, suggesting the intervention itself might not be solely responsible for the increase but may be a contributing factor. The consistent positive associations found across different contexts and study designs, such as the cross-sectional study by Abd-Elaziz et al14 in Egypt and the prospective cross-sectional study by Singh et al15 in India, underscore the importance of integrating structured contraceptive counselling into routine antenatal care as an effective strategy to improve postpartum contraceptive acceptance and empower informed contraceptive choices. A cross-sectional interview-based study conducted by Singh et al15 on postpartum women who delivered at the department of Obstetrics and Gynaecology, Safdarjung Hospital, New Delhi, demonstrated a notable increase of 35.6 per cent in the number of family planning acceptors due to the counselling services provided to postpartum women before discharge from the hospital and this increase aligns with our study.
The consistency in results across various studies suggests that the intervention approach has the potential to address the unmet need for postpartum family planning and contribute to the overall reproductive health and well-being of women in India and other similar settings.
Assessment of change in contraceptive knowledge among the mothers reveals that the intervention arm exhibited a significantly higher proportion of mothers with a good understanding across all knowledge variables post-intervention compared to the control arm. Effect size analysis using Cohen’s h revealed robust improvements in awareness of postpartum contraception and understanding of complications associated with closely spaced pregnancies in the intervention group. These effect sizes markedly surpassed those observed in the control group, establishing the substantial clinical impact of structured counselling. The magnitude of these effect sizes exceeds those documented in comparable interventions, including the RCT conducted by Sey-Sawo et al16 in Gambia. Specific content and delivery methods of our counselling program may have played a role in getting more significant knowledge improvement observed in our study.
In the intervention arm, knowledge regarding optimal pregnancy spacing demonstrated notable improvement (h=1.13, 95% CI: 0.94-1.33) in contrast to minimal changes observed in the control group (h=0.13, 95% CI: -0.15-0.41). This finding is particularly relevant in the Indian context, where a significant proportion of pregnancies occur unintentionally and are often characterised by insufficient intervals between births.
The increased contraceptive knowledge observed in our study, coupled with the improved postpartum contraceptive acceptance in the intervention group, highlights the potential for structured counselling interventions to bridge the knowledge-practice gap. This is particularly relevant in the context of the cross-sectional study by Singh et al17 in Uttarakhand, which found high contraceptive awareness (95.2%) that did not translate into high practice rates (42.8%).
The findings of our study align with existing literature, highlighting critical gaps in postpartum contraceptive services in Puducherry. Among the total postnatal mothers enrolled for the study by Selvaraj et al18 (n=227), nearly all (99.6%) received counselling on at least one topic, such as nutrition, hygiene, contraception, essential newborn care, breastfeeding, or immunization. However, according to Indian Public Health Standards (IPHS) guidelines, only 37.4 per cent of mothers received adequate counselling services by any health personnel from any health facility.
Additionally, postpartum home visits, a vital component for reinforcing contraceptive counselling and promoting service uptake, were found to be significantly under-utilised. Only 20.7 per cent of mothers received at least one visit by healthcare workers, and none received the recommended three visits required for adequate follow up. Similarly, the study conducted by Chauhan et al19 reported an existing contraceptive uptake of 20 per cent and 20.7 per cent in the comparison and intervention groups, respectively, in Puducherry at baseline. This underscores the systemic challenges that hinder the effective delivery of quality postnatal care, including contraceptive counselling and, thereby, poor contraceptive acceptance and uptake.
The findings of our study emphasise the urgent need for a more integrated and strengthened approach to postpartum care. Implementing structured counselling sessions, along with consistent follow ups and systemic support, could significantly enhance the acceptance and sustained use of postpartum contraceptives. Such strategies, if scaled and adapted effectively, have the potential to address the unmet need for family planning, reduce the prevalence of unintended pregnancies, and improve maternal and child health outcomes, particularly in similar resource-constrained settings.
The methodological strengths of this study include its parallel-arm cluster RCT design, implementation of evidence-based and culturally tailored counselling materials validated through expert review, and minimal loss to follow up. However, several limitations warrant consideration. The reliance on self-reported data introduces potential recall and social desirability biases. Additionally, the six-wk follow up period may not capture long-term contraceptive behaviours and continuation rates.
In clinical practice, these findings have immediate implications for antenatal care delivery. For a typical obstetric unit attending to 100 postpartum women monthly, implementation of structured contraceptive counselling could result in approximately 46 additional women initiating effective postpartum contraception. This substantial increase in contraceptive uptake has the potential to significantly reduce unintended pregnancies and their associated maternal-foetal complications, particularly in resource-limited settings where the burden of unmet contraceptive needs remains high.
Overall, the findings of this study have important implications for maternal and child health programmes in India. The effectiveness of the structured counselling intervention in improving postpartum contraceptive knowledge and acceptance underscores the potential for similar interventions to be integrated into routine antenatal and postnatal care services. This approach could contribute to reducing unintended pregnancies, improving birth spacing, and ultimately enhancing maternal and child health outcomes. Further research is warranted to explore the long-term sustainability of the observed improvements in postpartum contraceptive use, as well as the feasibility and scalability of the counselling intervention in diverse healthcare settings.
Financial support & sponsorship
The present study received funding from the Intramural Research Fund Committee, JIPMER (JIP/Res/Intramural/phs-1/2023-2024).
Conflicts of Interest
None.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- World population by country. Available from: https://www.worldometers.info/world-population/population-by-country/, accessed on December 4, 2023.
- World population day Statement 2023. Available from: https://www.unfpa.org/press/world-population-day-statement-2023, accessed on December 4, 2023.
- Family Planning. Available from: https://nhm.gov.in/index1.php?lang=1&level=2&sublinkid=821&lid=222, accessed on February 24, 2023.
- Acceptance of post-partum family planning among mothers attending for child immunisation services at Tertiary Care Hospital, Kolkata. Healthline. 2021;12:19-25.
- [CrossRef] [Google Scholar]
- Acceptance of contraceptive methods among postpartum women in a tertiary care center. J Obstet Gynaecol India. 2017;67:91-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Postpartum modern contraception utilsation and its determinants in Ethiopia: A systematic review and meta-analysis. PLoS One. 2020;15:1-21.
- [Google Scholar]
- The effect of prenatal counselling on postpartum family planning use among early postpartum women in Masindi and Kiryandongo districts, Uganda. Pan Afr Med J. 2015;21:138.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Impact of structured counseling on choice of contraceptive method among postpartum women. J Obstet Gynaecol India. 2016;66:471-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- National Family Health Survey (NFHS-5), 2019-21. India report. Available from: https://dhsprogram.com/pubs/pdf/FR375/FR375.pdf, accessed on December 4, 2023.
- Effect of prenatal counseling on postpartum follow-up and contraceptive use in women with gestational diabetes mellitus: A randomized controlled trial. Am J Obstet Gynecol MFM. 2023;5:101107.
- [CrossRef] [PubMed] [Google Scholar]
- The role of behavior change communication on knowledge and uptake of postpartum contraception among antenatal mothers in Puducherry: A randomized controlled trial. Int J Reprod Contracept Obstet Gynecol. 2020;9:2024.
- [CrossRef] [Google Scholar]
- Structured antenatal counselling and postpartum contraceptive uptake in South West Nigeria. J West Afr Coll Surg. 2019;9:8-14.
- [CrossRef] [Google Scholar]
- Effect of antenatal counseling on postpartum family planning among women attending family medicine units in 6th of October city. Med Integr Student Res J. 2018;1:1-8.
- [CrossRef] [Google Scholar]
- Awareness and acceptance of contraception in post-partum women in a tertiary care hospital of Delhi. Int J Reprod Contracept Obstet Gynecol. 2015;4:690-5.
- [CrossRef] [Google Scholar]
- Effects of postpartum family planning counselling on contraceptive knowledge, attitude and intention among women attending a general hospital in the Gambia: A randomized controlled trial. Open Access J Contracept. 2023;14:61-72.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Awareness, attitude and practise of contraception among antenatal women in a tertiary care hospital in Uttarakhand. Int J Med Heal Res. 2020;6:13-6.
- [Google Scholar]
- Community-based assessment of postnatal care in Puducherry – A cross-sectional study. J Fam Med Prim Care. 2021;10:798.
- [Google Scholar]
- The role of behavior change communication on knowledge and uptake of postpartum contraception among antenatal mothers in Puducherry: a randomized controlled trial. Int J Reprod Contracept Obs Gynecol. 2020;9:2024-8.
- [CrossRef] [Google Scholar]






