Translate this page into:
Effect of public-private partnership in treatment of sexually transmitted infections among female sex workers in Andhra Pradesh, India
Reprint requests: Dr Parimi Prabhakar, India HIV/AIDS Alliance, Sarovar Center, 5-9-22, Secretariat Road Hyderabad 500 063, India e-mail: pprabhakar@allianceindia.org
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Providing sexually transmitted infection (STI) services to female sex workers (FSWs) in rural and resource constrained settings is a challenge. This paper describes an approach to address this challenge through a partnership with government health facilities, and examines the effect of this partnership on the utilization of STI services by FSWs in Andhra Pradesh, India.
Methods:
Partnerships were formed with 46 government clinics located in rural areas for providing STI treatment to FSWs in 2007. Government health facilities were supported by local and State level non-government organizations (NGOs) through provision of medicines, training of medical staff, outreach in the communities, and other coordination activities. Data from programme monitoring and behaviour tracking survey were used to examine the accessibility and acceptability in utilization of STI services from partnership clinics.
Results:
The number of FSWs accessing services at the partnership clinics increased from 1627 in 2007 to over 15,000 in 2010. The average number of annual visits by FSWs to these clinics in 2010 was 3.4. In opinion surveys, the majority of FSWs accessing services at the partnership clinics expressed confidence that they would continue to receive effective services from the government facilities even if the programme terminates. The overall attitude of FSWs to visit government clinics was more positive among FSWs from partnership clinic areas compared to those from non-partnership clinic areas.
Interpretation & conclusions:
The partnership mechanism between the NGO-supported HIV prevention programme and government clinic facilities appeared to be a promising opportunity to provide timely and accessible STI services for FSWs living in rural and remote areas.
Keywords
Partnership clinic
PPP service delivery
rural sex work
sex workers
STI
Prevention and treatment of sexually transmitted infections (STIs) is a key component of HIV/AIDS programmes in developing countries123, as these infections can considerably increase the risk of HIV infection456. HIV prevention programmes in resource poor settings like India provide STI treatment services through various models including programme supported STI clinics [clinics funded and managed by non-governmental organization (NGO) under the HIV prevention project, located in an area with atleast 500 high-risk group members, staffed with a physician, nurse, and counselor and attached with drop-in-centre], mobile/satellite clinics (clinics which operates on a regular, fixed day and time in areas with relatively few high-risk groups), referrals to government clinics, and community preferred providers clinics (private health care doctors identified by local NGO and community members for STI treatment)2789. Of these, project-run static clinics are the most widely implemented clinics, located mainly in urban and semi-urban areas. These clinics operate from drop-in-centres located in and around the sites of sex work activities810. Empirically it has been observed that static clinics have not been able to provide adequate STI services to sex workers in rural areas due to the scattered nature of the sex worker population in those areas, and the stigma associated with sex work as well as the high operating cost associated with static clinics11.
To ensure the delivery of sustainable and, quality of STI services at low operating costs beyond the static clinics two options were considered: setting up a preferred provider model clinic, and partnering with public health facilities. In the first approach, preferred private providers, identified after consultations with sex workers from the area, were contracted to provide STI treatment services to sex workers visiting their clinics8. In the second approach, a partnership was forged with government health providers in rural areas, such as staff in primary health centres (PHCs) and community health centres (CHCs) to provide quality STI treatment services. It has been shown that private-public sector partnerships can serve as an effective and sustainable service delivery model provided issues related to quality of care and efficiency of service delivery are addressed in government health facilities1213141516. Though the private-public partnership approach has been adopted to provide services to general populations in many Indian settings17, literature documenting the provision of STI services to high-risk groups using this approach is scarce.
This study provides a detailed description of a partnership model between non-governmental organizations (NGOs) and government health facilities to provide STI treatment services to female sex workers (FSWs) as part of an HIV prevention programme in Andhra Pradesh, India. It describes the process of negotiation and engagement with government health facilities to provide STI treatment to FSWs, and examines the evidence regarding the accessibility, acceptability and utilization of this partnership model during the period 2007-2010.
Material & Methods
The setting: The partnership between NGOs and government health facilities to provide STI treatment to FSWs was implemented in 13 inland districts of Andhra Pradesh where the adult HIV prevalence has been estimated to be nearly 1 per cent18. Unlike the coastal districts, these inland districts are mainly rural, and the population is dependent on subsistence agriculture. There were considerable variations in economic and development indicators across these districts19. The HIV prevention programme in these 13 districts was started in 2004 providing services to about 15000 FSWs initially. The programme expanded its coverage to include another 13,000 FSWs by 2006. These FSWs were located across 139 mandals (sub-districts) including 46 rural mandals. Mapping and needs assessment exercise in these districts highlighted the lack of access to STI treatment facilities as a major barrier in HIV prevention efforts, particularly in rural areas with the existing model of static clinic and network of preferred providers.
The intervention
Pilot phase: The aim of initiating the partnership was to provide effective STI services to FSWs in the underserved rural areas and strengthen the institutional capacity of health providers. The availability of government health facilities, mainly PHCs, in the rural areas provided an opportunity to establish partnerships between government facilities and local NGOs. Partnerships with government health facilities were piloted in six mandal headquarters of a district. Two NGOs were selected as implementing partners and were trained in outreach activities and the provision of STI clinical services. National AIDS Control Organization (NACO) intervention guidelines for FSWs were followed for selecting health facilities and service providers20. Discussions were held with local sex worker groups to obtain their opinions and reactions regarding locations and the acceptability of the health facilities.
While the process of building partnerships with doctors from government health facilities was underway, local NGOs negotiated with district health officials to obtain permission for engaging doctors from these facilities. The team from State level NGO also met with officials from the State AIDS Control Society (SACS), the government agency managing the State HIV prevention programme to seek help in advocating with the State Directorate of Health Services for partnership arrangement approvals. Auxiliary nurse mid-wives (ANMs) were recruited at each facility to support the doctors in providing STI services. ANMs were trained to conduct routine clinic operations, including drug procurement, clinic system management, infection control, documentation, and risk-reduction counselling.
The STI technical officer from the State level NGO visited the government health facilities to orient doctors about syndromic case management and STI clinic operational guidelines10. Efforts were also made to sensitize doctors and ANMs on issues related to FSW, in particular, the need for confidentiality and respect for patients’ rights. NACO recommended guidelines on management of STI was used to train medical doctors and ANMs in the study areas to ensure uniformity in trainings20. Doctors were provided with appropriate treatment algorithms and other written materials on syndromic case management.
Scale-up of the programme: Soon after permissions were obtained from the State and district health officials for the government health facilities to engage in this initiative, the model was upscaled to all the rural areas with similar protocols as followed in the pilot phase. In addition to regular trainings for doctors and nurses, two annual reorientation training sessions were conducted in every six months.
Roles of the partners in the partnership: The primary role of local level NGOs was to negotiate with the district authorities to obtain permission for engaging doctors from government health facilities and allow them time to attend training sessions. They were also responsible for recruiting ANMs, procuring drugs and supplies, and reporting to the State level NGO. The peer educators and outreach workers at these NGOs met groups of sex workers at the places of solicitation (hotspots of sex work activity) and provided information on STI/HIV, motivated them to seek services from government health facilities, provided free condoms, and conducted verbal screening for tuberculosis. Staff at the State level NGO were responsible for training the doctors, supporting the establishment of clinic systems according to the operational guidelines, facilitating the supply of drugs, testing kits, and other materials, and providing supportive supervision. The Health department at the State and district approved the use of the clinic facilities and the services of doctors. District health officials were responsible for ensuring doctors’ availability at the health facilities and giving them permission to attend trainings organized by State level NGO.
Sex worker treatment package: The basic minimum services provided in the partnership clinics included quarterly medical check-ups, presumptive treatment, STI treatment using the syndromic approach, follow up for STI cases, risk-reduction counselling including condom promotion, verbal screening and testing for tuberculosis, biannual syphilis testing and referral for HIV testing. All these services and necessary medicines were provided free of cost to FSWs.
Clinic-outreach coordination: Weekly meetings were organized by NGO project coordinators to ensure coordination between clinic and outreach activities. If any FSW was diagnosed with an STI, the ANM discussed the case with the peer educator to ensure compliance with treatment and follow up visits to the clinic.
Monitoring mechanism: Technical officers from the State level NGO visited the health facilities every quarter to monitor the quality of clinical services and provide technical support. The monitoring team made regular assessment of the clinic performance and systems using a validated standardized quality-monitoring tool. The performance of a clinic was assessed based on the number of FSWs (i) accessing clinical services, (ii) diagnosed with STI, (iii) provided presumptive treatment, (iv) referred to other facilities for services such as HIV testing and syphilis testing.
Two data sources were used to examine the accessibility and utilization of the partnership model for STI service delivery: (i) programme monitoring data, and (ii) behavioural tracking survey.
Program monitoring data: The State level NGO developed and defined programme monitoring indicators and established monitoring and information system (MIS) to gather data periodically on different indicators related to programme inputs and outputs. The MIS designed for this programme was independent of the structure of NACO's MIS. Programme monitoring data were collected monthly at the local level NGO which were aggregated in paper formats and consolidated by the State level NGO. FSWs who accessed services at the programme clinics were assigned an unique identification number to track their service utilization during the programme. The staff from State level NGO provided technical support to local level NGO to ensure integrity and quality of data as well as flow of data and maintenance of MIS.
Behavioural tracking survey: Independent of the programme monitoring data, a cross-sectional survey, named as behavioural tracking survey (BTS), was conducted among FSWs in five districts: Ananthpur, Warangal, Khamam, Kurnool and Medak. The objective of BTS was to monitor the key components of the HIV prevention programme: safe sex behaviour, STI treatment seeking behaviours and community mobilization. Data were collected using a two-stage sampling design, wherein FSWs’ hotspots were selected during the first stage and FSWs were selected randomly from each selected hotspot during the second stage. A sample size of 400 FSWs was estimated for each district, allowing for detection of an absolute difference of 15 per cent or more from the assumed value of 50 per cent for consistent condom use with all clients, with 95 per cent confidence, 90 per cent power and a design effect of 1.7. Detailed sampling procedures for selection of sites and sex workers are discussed elsewhere21222324. At the end of the survey, 2389 FSWs were approached, of whom 403 either refused to participate or withdrew during the interview. This resulted in a total analytical sample of 1986 FSWs with a response rate of 83 per cent. Sample weights were calculated to account for the unequal selection probability of respondents and non-response rates. The institutional review boards of Family Health International (FHI) and Karnataka Health Promotion Trust (KHPT) reviewed and approved the protocols of BTS. A comprehensive informed consent process was followed and no names or identifying information was recorded.
Measures: Indicators were developed to assess the utilization and acceptability of services from the partnership model. Six indicators from the programme monitoring data were used and these were monitored annually from 2007 to 2010. The indicators used to assess service utilization from programme monitoring data were: (i) number of FSWs who visited clinic, (ii) FSWs who visited clinic with STI-related symptoms, (iii) FSWs who were provided with presumptive treatment, (iv) FSWs who underwent speculum examination, (v) FSWs who were screened for tuberculosis, and (vi) number of FSWs who were tested for and diagnosed with syphilis.
BTS collected wide range of information on FSWs’ behaviour including experience of STI-related symptoms, service utilization and attitude towards health facilities. Single item questions were asked to understand if they had experienced one of the following STI-related symptoms in the six months prior to survey: genital ulcer/sore, genital discharge, or lower abdominal pain. To understand service utilization in the last six months, single item questions on number of times visiting STI clinics (recoded into “0” if less than two visits; else coded as “1” to indicate at least two visits), and HIV test conducted were asked. FSWs were asked single item questions to understand their attitude towards utilization of government health services. Responses were as follows: not at all confident, somewhat confident, very confident, and completely confident. FSWs who responded either ‘very confident’ or ‘completely confident’ were combined to represent confident attitude and coded as ‘1’, and the remaining were coded as ‘0’.
The FSWs were grouped into three groups based on information on the type of clinic providing services in the survey area. These groups were: area covered by partnership clinics (coded as ‘2’), area covered by non-partnership clinics (coded as ‘1’), and area covered by other clinics (coded as ‘0’). ‘Non-partnership clinics’ included either static clinics or preferred-provider clinics; and ‘other clinics’ were clinics functioning without support from State level NGO. This variable was considered as the key independent variable for multivariate analysis.
Statistical analyses: Programme monitoring data are presented in terms of absolute numbers and percentages. Bivariate and multivariate analyses were conducted to present the results of the behavioural tracking survey. A series of multiple logistic regression models were generated to examine the differences in programme outcomes, and attitude towards government clinic and service utilization. The logistic regression models were adjusted for age (continuous), educational status (no formal education versus some formal education), marital status (currently/formerly/never married), duration in sex work, solicitation location (home, brothel, street, and phone), and residential location (rural, semi-urban, and urban). All the analyses were performed using Stata 11.1 (Stata Corp, USA).
Results
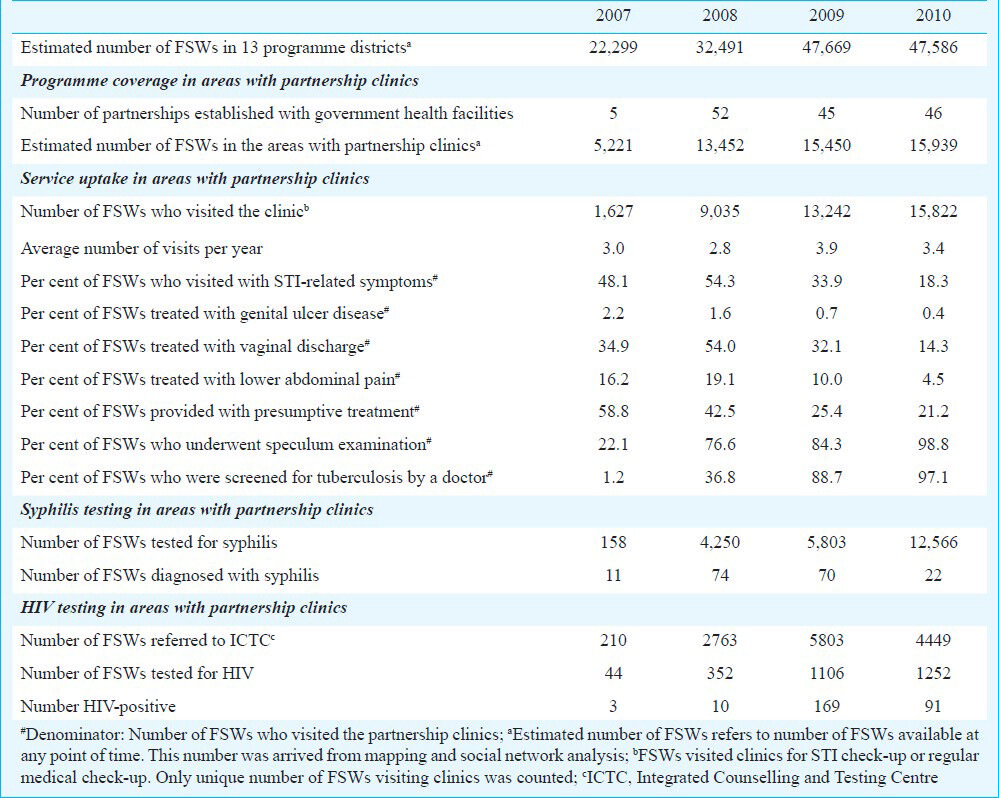
Programme coverage and utilization of STI services from government health facilities under the partnership model during 2007-2010 are presented in Table I. The data indicated that the number of FSWs visiting government health facilities increased sharply after the initiative was scaled-up in 2008. During 2008-2010, there was a decline in reporting of STI symptoms (from 54 to 18%) and presumptive treatment (from 43 to 21%) among FSWs. Notable increases were observed in the proportion of FSWs who underwent speculum examination, TB screening, syphilis and HIV testing.
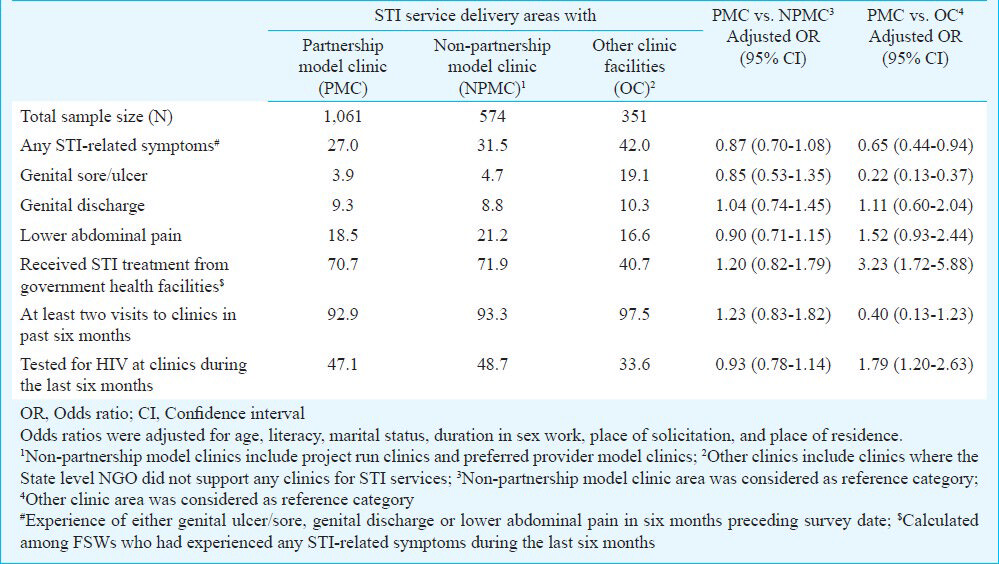
The effects of partnership model clinics on experience of STI-related symptoms, STI treatment seeking behaviour and other clinical outcomes among FSWs are presented in Table II. Experience of any STI-related symptom, including genital ulcers/sores, genital discharge, and lower abdominal pain, were similar whether FSWs belonged to areas with partnership clinics or non-partnership clinics. Among those who experienced at least one STI symptom in the last six months, FSWs from areas with a partnership clinic were three times more likely to seek treatment from the government health facilities than those belonged areas where clinics were not supported by State level NGO (71 vs. 41%, AOR: 3.23, 95% CI: 1.72–5.88). There were no significant differences in frequency of clinic visits by FSWs in areas with or without a partnership clinic. Moreover, the odds of HIV testing were approximately two times higher among FSWs in areas with a partnership clinic than in areas with areas with clinics without State level NGO support (47 vs. 34%, AOR: 1.79, 95% CI: 1.20-2.63) (Table II).
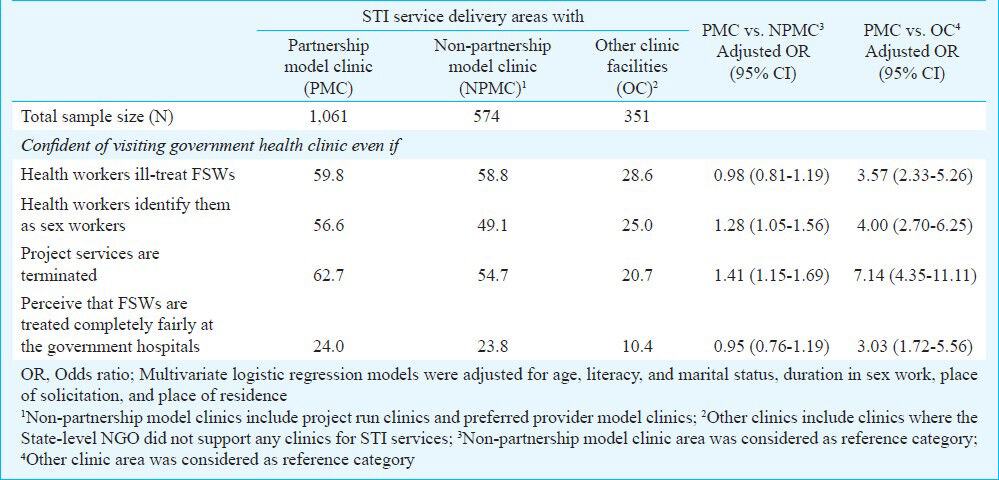
Further, FSWs were four times more likely to receive STI services from clinics despite being ill treated by health workers in areas with partnership clinics than FSWs from areas with other clinics (60 vs. 29%, AOR: 3.57, 95% CI: 2.33-5.26) (Table III). Compared to FSWs from areas with non-partnership clinics, those from areas with partnership clinics were more likely to be confident in accessing services from government facilities, even if they were identified as sex worker (57 vs. 49%, AOR: 1.28, 95% CI: 1.05-1.56) or even if the project services were terminated (63 vs. 55%, AOR: 1.41, 95% CI: 1.15-1.69). Compared to FSWs from areas with programme supported statis clinics, those from areas with partnership clinics were more likely to perceive fair treatment at government hospitals (10 vs. 24%, AOR: 3.03, 95% CI: 1.72-5.56) (Table III).
Discussion
The study findings indicated that providing STI treatment services through partnership with government health facilities improved the utilization of such facilities among female sex workers in Andhra Pradesh. This also showed that the outreach activities of NGOs and peer educators successfully motivated FSWs to visit the partnership clinics. These findings were consistent with results from another study in Andhra Pradesh, which indicated that FSWs in intervention areas had a positive attitude to seeking services from government health facilities21. The monitoring data indicated that certain services were better utilized as compared to certain other indicators. For example, proportion of FSWs who underwent speculum examination was higher than those who were screened for tuberculosis in 2007 and 2008. This can be due to the fact that the programme has emphasized on FSWs’ speculum examination since the inception; however, efforts for screening of tuberculosis were generated much later. Although no specific information on cost involved was collected in these partnership clinic model, information from secondary sources25 suggested that the cost invested per sex worker was lower in these clinics as compared to that in static clinics. Analysis of costing data suggests that the State level NGO spent around ₹ ≅ 600 INR (12 USD) per sex worker of which 14 per cent was spent on STI services25. As the partnership clinics required less investment in developing infrastructure, it would have cost lesser than the average cost spent indicating cost efficiency of this model of STI service delivery.
Although the data suggest that the partnership with government health facilities has been relatively successful, the effectiveness of such partnerships is highly context specific. The criticism of partnership between private and public facilities is well known26, and it is noteworthy that in rural under-served areas, only a few alternative approaches beyond the partnership model exist for the delivery of health services27. In resource-constrained settings, innovative actions are required to overcome deficient health facilities, and in many of those resource-poor rural areas, government health facilities are the only available resources. In a partnership mechanism in rural Karnataka17, the government had assigned NGOs to manage staff and operate some PHCs. Another example of successful partnership programme was the program implemented by the Society for Education, Welfare, and Action (SEWA) rural in Gujarat12. The private-public partnership clinics described here were located within the government-operated PHCs or CHCs and utilized government doctors and infrastructure; these facilities were strongly supported by the NGOs in terms of training, outreach and monitoring including data collection activities. This arrangement was more flexible than those adopted in the ‘conventional models’, such as SEWA rural and other NGO-dominated arrangements.
The study findings indicate scope for further experimentation with flexible partnerships, which does not require an NGO to assume complete control over the operation and management of the clinics. No strict single formula needs to be followed to build partnerships with government health facilities. Further, building a partnership with the government health facilities for STI service delivery was not always easy. Alongside the challenges faced by the programme due to frequent transfers of doctors, some doctors were unwilling to continue the partnership arrangements, which resulted in the loss of a few clinics in 2009. In some ‘lost clinic’ cases, FSWs complained that the clinic provider had a negative attitude towards them.
While service utilization by sex workers in areas with partnership clinics was improved, there were several challenges to this approach. These included: (i) doctors’ attendance at the training sessions was irregular; (ii) frequent transfers of doctors across health facilities requiring a significant number of trainings; and (iii) frequent absence of doctors, particularly during senior government officials’ visits. These issues need to be taken into consideration if the programme needs to be scaled-up.
Overall, the HIV prevention initiative in Andhra Pradesh has utilized three different models for STI service delivery based on the special geographical and social characteristics of the areas with FSW populations. It is not particularly useful to compare the static clinic, preferred private provider, and partnership clinic models, as each was designed to meet the requirements of particular social and geographic locations. In settings like Andhra Pradesh where sex work is prevalent in both rural and urban areas28, it is likely that all three types of clinic facilities are necessary and useful. Irrespective of the level of STIs among sex workers, the partnership model can serve as an alternative mechanism to provide STI and other general health services to sex workers in areas where sex workers are scattered and establishing static clinic may not be cost effective. Moreover, STI prevalence ranging from 3-10 per cent has been reported among FSWs in the area where the partnership clinics were established28. This study also observed that FSWs who belonged to the areas with partnership clinic models were less likely to experience STI and more likely to receive STI treatment and undergo HIV test than those residing in area where clinics were not supported by the State level NGO. This indicates that the support of State level NGO in building the capacity of partnership clinics and providers have resulted in better service provision and ultimately resulting in better utilization of services as compared to areas where such support systems were not in place.
Although the current study findings offered important recommendations on the usefulness of partnership with government health clinics over other models, the study findings should be interpreted in the light of certain limitations. No biological data were collected on STI and HIV and only self-reported STI symptoms were used as the study outcomes. Future studies should make an attempt to include the STI and HIV incidence/prevalence as outcomes to assess the behaviour change. Further, it can be argued that improved service utilization over time may not necessarily reflect behavioural modification/change. However, studies conducted in this geographical area have demonstrated a significant improvement in the safe sex behaviour of FSWs29 and hence to some extent the decline in STI symptoms as well as improvement in treatment seeking behaviour could be linked to the change in behaviours.
In summary, the HIV prevention initiative in Andhra Pradesh, which used government health facilities to provide STI treatment to FSWs, offers a sustainable approach to provide timely and accessible services. Such partnerships may not only promote HIV prevention services, but also promote the utilization of other health services from the government health facilities by marginalized populations. The side effects of such a partnership model have not been carefully assessed through well-designed operations research; however, upscaling partnership clinics to provide sex workers STI treatment and other services could help reduce institutional and individual level stigma and provide a one-stop shop for comprehensive and accessible health services.
References
- Assessment of attitudes and practices of providers of services for individuals at high risk of HIV and sexually transmitted infections in Karnataka, south India. Sex Transm Infect. 2010;86:131-5.
- [Google Scholar]
- Pursuing scale and quality in STI interventions with sex workers: initial results from Avahan India AIDS Initiative. Sex Transm Infect. 2006;82:381-5.
- [Google Scholar]
- Syndromic management of sexually-transmitted infections and behaviour change interventions on transmission of HIV-1 in rural Uganda: a community randomised trial. Lancet. 2003;361:645-52.
- [Google Scholar]
- Advancement of global health: key messages from the Disease Control Priorities Project. Lancet. 2006;367:1193-208.
- [Google Scholar]
- Interventions against sexually transmitted infections (STI) to prevent HIV infection. Br Med Bull. 2001;58:129-53.
- [Google Scholar]
- Syndromic approach for treatment of STIs: time for a change. Lancet. 2006;367:1380-1.
- [Google Scholar]
- The Sonagachi Project: a sustainable community intervention program. AIDS Educ Prev. 2004;16:405-14.
- [Google Scholar]
- Bill & Melinda Gates Foundation in India (BMGF). Treat and prevent: Avahan's experience in scaling Up STI services to groups at high risk of HIV infection in India. New Delhi, India: BMGF; 2010.
- [Google Scholar]
- Sexually transmitted infection control with sex workers: regular screening and presumptive treatment augment efforts to reduce risk and vulnerability. Reprod Health Matters. 2003;11:74-90.
- [Google Scholar]
- National AIDS Control Organisation (NACO). National AIDS: Control Programme: Phase IV, Technical Working Group: STI/RTI Prevention and Control Programme. New Delhi, India: NACO; 2011.
- [Google Scholar]
- A primary evaluation of service delivery under the National Rural Health Mission (NRHM): findings from a study in Andhra Pradesh, Uttar Pradesh, Bihar and Rajasthan. New Delhi, India: Planning Commission of India; 2009.
- [Google Scholar]
- An assessment of public-private partnership opportunities in India. New Delhi, India: United States Agency for International Development (USAID); 2004.
- [Google Scholar]
- Public-private partnerships for providing healthcare services. Indian J Med Ethics. 2007;4:174-5.
- [Google Scholar]
- Public - private ‘partnerships’ in health - a global call to action. Health Res Policy Syst. 2004;2:5-12.
- [Google Scholar]
- Public-private partnerships for health: their main targets, their diversity, and their future directions. Bull World Health Organ. 2001;79:713-20.
- [Google Scholar]
- Blurring of boundaries: Public-private partnerships in health services in India. Econ Pol Wkly. 2008;43:62-71.
- [Google Scholar]
- Public-private partnerships in health care in India: Lessons for developing countries. London, UK: Routledge; 2009.
- [Google Scholar]
- Estimate of HIV prevalence and number of people living with HIV in India 2008-2009. BMJ Open. 2012;2:e000926.
- [Google Scholar]
- Inter-district variation of socio-economic development in Andhra Pradesh. J Indian Soc Agric Stat. 2009;63:35-42.
- [Google Scholar]
- National AIDS Control Organisation (NACO). National AIDS Control Programme Phase III (2006-2011): strategy and implementation plan. New Delhi, India: NACO; 2006.
- [Google Scholar]
- Mobilizing community collectivisation among female sex workers to promote STI service utilisation from the government healthcare system in Andhra Pradesh, India. J Epidemiol Community Health. 2012;66(Suppl 2):ii62-8.
- [Google Scholar]
- Community advocacy groups as a means to address the social environment of female sex workers: a case study in Andhra Pradesh, India. J Epidemiol Community Health. 2012;66(Suppl 2):ii87-94.
- [Google Scholar]
- Community mobilisation programme for female sex workers in coastal Andhra Pradesh, India: processes and their effects. J Epidemiol Community Health. 2012;66(Suppl 2):ii78-86.
- [Google Scholar]
- Anal sex and associated HIV-related sexual risk factors among female sex workers in Andhra Pradesh, India. Sex Health. 2012;9:430-7.
- [Google Scholar]
- Economic analysis of Avahan Interventions in India. Expert consultation on Costing HIV Responses in Asia. October 28-29. 2010.
- [Google Scholar]
- Immunisation for All? A critical look at the first GAVI partners meeting. HAI Europe. 2001;6:1-9.
- [Google Scholar]
- Combating diseases associated with poverty financing strategies for product development and the potential role of public-private partnerships. Geneva, Switzerland: The Initiative on Public-Private Partnerships for Health, Global Forum for Health Research; 2001.
- [Google Scholar]
- Demography and sex work characterstics of female sex workers in India. BMC Int Health Hum Rights. 2006;6:5-15.
- [Google Scholar]
- Condom use and prevalence of syphilis and HIV among female sex workers in Andhra Pradesh, India - following a large-scale HIV prevention intervention. BMC Public Health. 2011;11(Suppl 6):S1.
- [Google Scholar]






