Translate this page into:
Effect of gender, biochemical parameters & parathyroid surgery on gastrointestinal manifestations of symptomatic primary hyperparathyroidism
Reprint requests: Dr Sanjay Kumar Bhadada, Associate Professor, Department of Endocrinology, Postgraduate Institute of Medical Education & Research, Chandigarh 160 012, India e-mail: bhadadask@gmail.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Information on gastrointestinal manifestations and then response after curative parathyroid surgery is scarce in symptomatic primary hyperparathyroidism (PHPT). This study was carried out to analyse gastrointestinal manifestations in patients with PHPT and their associations with biochemical parameters.
Methods:
This retrospective study included 153 patients with symptomatic primary hyperparathyroidism (PHPT). The signs and symptoms pertaining to gastrointestinal system were analyzed. The difference of symptoms between men and women and difference in biochemical parameters in presence of different symptoms were evaluated. The relationship between serum calcium, phosphate and parathyroid hormone (PTH) levels with presence of gallstone and pancreatitis was also studied.
Result:
Of the 153 patients, 46 (30%) were men. The mean age was 39.2 ± 13.9 yr. Nearly 80 per cent of PHPT patients had at least one symptom/ sign related to gastrointestinal system. The most common gastrointestinal manifestations were abdominal pain 66 (43%), constipation 55 (36%), and nausea/or vomiting 46 (30%). Nearly one-fourth 34 (22%) of patients had a history of either gallstone disease or cholecystectomy or both. The prevalence of gallstone disease was higher in women (P<0.05). Imaging and biochemical evidence of pancreatitis was found in 27 (18%) patients. Pancreatitis was more common in men compared to women (P<0.05) despite the higher prevalence of gallstones in women. Serum calcium, phosphate or PTH levels were not associated with high risk for gallstone disease, however, serum calcium (P<0.05) was associated with 1.3 times higher risk of developing pancreatitis. In majority of patients, gastrointestinal manifestations resolved within three months of curative parathyroidectomy. Except two patients, none had recurrence of pancreatitis.
Interpretation & conclusions:
The study revealed that the gastrointestinal symptoms were common in patients with symptomatic PHPT. There was not much gender difference in gastrointestinal symptoms except higher occurrence of gallstones in women and pancreatitis in men. There was no difference in biochemical profile between those who had and did not have gastrointestinal symptoms.
Keywords
Gall stone
gastrointestinal symptoms
pancreatitis
primary hyperparathyroidism
The primary hyperparathyroidism (PHPT), is characterized by inappropriately elevated serum parathyroid hormone (PTH) in presence of hypercalcaemia and the most common cause of PHPT is parathyroid adenoma1. The classical PHPT was considered as a multisystem disorder with clear neurologic, psychiatric, gastrointestinal, and cardiovascular consequences2. Though there are many reports on isolated gastrointestinal symptoms like gallstones and pancreatitis in patients with PHPT, the earliest description on gastrointestinal manifestations as a presenting feature of PHPT was reported by St Goar WT in 19573. A cause and effect relationship has not yet been established for these gastrointestinal symptoms and data regarding the association of gallstones456 and pancreatitis78 with PHPT are still conflicting. Further, with the use of autoanalyzer and routine estimation of calcium profile as a part of annual physical examination in the United States, presentation of PHPT changed dramatically from symptomatic one to asymptomatic9, and this created further controversies in the nature and extent of involvement of these target organs in PHPT2.
Most of the studies reported isolated incidence of either gallstones456 or pancreatitis78 and a few studies on clinical presentations of PHPT described high incidence of some gastrointestinal symptoms1011 but the gastrointestinal manifestations have not been analysed systemically. Though some studies on gastrointestinal manifestations of PHPT have been published, but all are two decades old3121314. Since gastrointestinal symptoms are non specific and lack the cause and effect relation in patients with PHPT, the literature is limited on this aspect. Further, studies on effect of curative parathyroidectomy on gastrointestinal symptoms are also lacking. The present study was, therefore, planned to analyze the gastrointestinal manifestations and their association with biochemical parameters in patients with PHPT.
Material & Methods
Patient selection: Data for this retrospective study were retrieved from PHPT registry of the department of Endocrinology, Postgraduate Institute of Medical Education & Research (PGIMER), Chandigarh, India. All cases of histopathological proven PHPT from January 2001 to December 2009 were included in the study. PHPT was defined as inappropriately elevated PTH in presence of hypercalcaemia. Preoperatively parathyroid adenoma was localized in most with either ultrasonography and/or sestamibi scintigraphy. Patients with secondary or tertiary hyperparathyroidism were excluded from the study. The study protocol was approved by the ethics committee of the Institute.
Definition of gastrointestinal symptoms: Subjective symptoms like anorexia, nausea/vomiting and abdominal pain were reported as present if patient reported these symptoms at the time of presentation. All PHPT patients were evaluated for the presence of gallstone and pancreatitis. Gall stone(s) was defined as either imaging evidence of gallstones and/or a history of cholecystectomy. Acute pancreatitis was diagnosed based on the presence of typical symptoms, elevation of pancreatic enzymes more than three times and positive radiological evidences. Renal stone disease was defined as either imaging findings consistent with renal stone disease or history of surgery for renal stone(s). Anaemia was defined as haemoglobin <13 g/dl in male and less than 12 g/dl in female.
Biochemical and hormonal investigations: Serum calcium (8.6-10.2 mg/dl), inorganic phosphate (2.7-4.5 mg/dl), albumin (3.4-4.8 mg/dl), and alkaline phosphatase (40-129 IU/l) were measured by autoanalyzer (Roche diagnostics, Modular P 800, Indianapolis, USA). Serum intact PTH (15-65 pg/ml) was measured by chemiluminescence assay (Roche, ELYCYS 2010) and 25 (OH) D (11.1-42.9 ng/ml) was measured by radioimmunoassay using commercially available kits (DiaSorin Inc., Stillwater, MN, USA).
Statistical analysis: The statistical analysis was carried out using SPSS 15 (Chicago, USA). Continuous variables were described as mean ± SD and categorical variables were described as frequencies and proportions. Chi square test was applied to assess significant difference in symptoms between men and women. Paired t-test was applied to find out the difference in biochemical parameters in presence of different symptoms. Binary logistic regression analysis was performed to calculate odd ratio (OR) for development of gallstone and pancreatitis in relation to high calcium, low phosphate and elevated PTH levels. All statistical tests were two-sided and performed at a significance level of P<0.05.
Results
One hundred and fifty three patients with PHPT were analyzed in the present study; 46 were men (30%) and 107 (70%) were women. The mean age of patients with PHPT was 39.2 ± 13.9 yr (range; 11-74 yr, 36.4 ±13.7 yr for men and 40.4 ±13.8 yr for women). The lag time between the symptoms suggestive of PHPT and diagnosis was 46.3 ± 39.9 months (Median 36, 37-54; 95% CI). The mean (±SD) preoperative serum calcium, phosphate, 25 (OH)D and PTH levels were 11.5± 1.6 mg/dl, 3.1±0.9 mg/dl 27.6 ± 28.3 pg/ml and 735.2 ± 622.9 pg/ml (Median- 526 pg/ml), respectively. The most common location of parathyroid adenoma in our study was left inferior parathyroid region (36%) followed by right inferior parathyroid region (22%). One patient had parathyroid carcinoma and none of these patients had parathyroid hyperplasia. The mean weight of parathyroid adenoma was 6.2 ± 5.9 g (Median-4.0, 4.2-8.2; 95% CI).
Clinical presentations of patients with PHPT: The most common symptom noted at the time of diagnosis was fatigue 105 (69%) followed by bone pain 89 (58%), renal stones 75 (49%) and fracture 60 (39%) while anaemia was present in 89 (58%) of the PHPT patients.
Eighty per cent of PHPT patients had at least one symptom or sign related to gastrointestinal system. The most common gastrointestinal manifestation was abdominal pain 66 (43%). Other symptoms pertaining to gastrointestinal system were constipation 55 (36%), nausea and/or vomiting 46 (30%), anorexia 40 (26%), and dyspepsia 37 (24%). Thirty four (22%) patients had history of either imaging evidence of gallstone and/ or cholecystectomy. Twenty two (14%) patients had imaging evidence of gallstones and 27 (18%) had history of cholecystectomy for symptomatic gall stone disease. Twenty seven patients (18%) had imaging and biochemical parameters consistent with pancreatitis. Of the 27 patients with pancreatitis, none had history of alcohol abuse or other risk factor known to cause pancreatitis, four had gallstone disease but underwent cholecystectomy prior to pancreatitis. Twenty six of these (96.29%) had two or more episodes of pancreatitis before the diagnosis of PHPT was established.
Gender difference in gastrointestinal symptoms among patients with PHPT: Gastrointestinal symptoms were comparable in both sexes except anaemia (P<0.05) and gallstones (P<0.05) were more prevalent in women while abdominal pain (P<0.05) and pancreatitis (P<0.05) were more common in men. History of cholecystectomy was higher but statistically insignificant in women compared to men. Pancreatitis was more common in men compared to women despite the prevalence of gallstones being greater in women (Fig.).
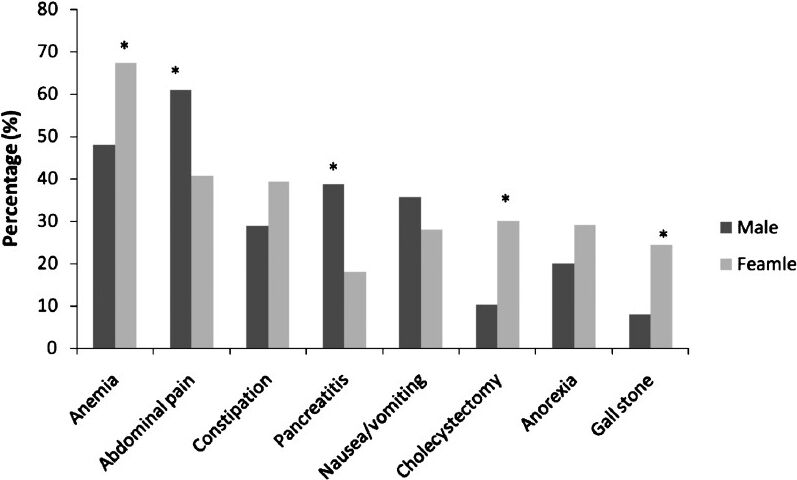
- Gastrointestinal symptoms and signs in male and female PHPT patients (n=153). *P<0.05.
Differences in biochemical parameters in presence of different symptoms: Patients of PHPT with nausea/vomiting had higher serum phosphate (P<0.05) but comparable serum calcium and PTH levels than those who did not have nausea/vomiting. Constipation in patients with PHPT was associated with low phosphate (P<0.01) but not with hypercalcaemia. Pancreatitis was more common in those who had low PTH levels P<0.01 (Table).
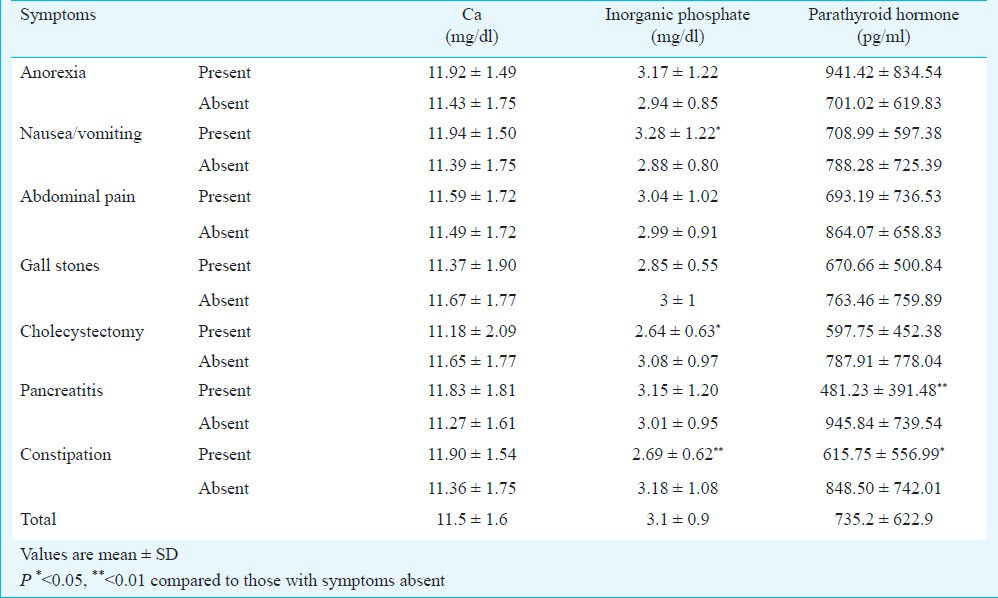
Association between biochemical parameters with gallstone and pancreatitis: Using binary logistic regression analysis, serum calcium [odds ratio (OR)-0.88 (0.6-1.1, 95% CI), P=0.4], phosphate [OR= 0.81 (0.4-1.4, 95% CI), P=0.5] or PTH levels [OR=1 (0.9-1.1, 95% CI), P=0.6] were not found to be risk factors for development of gallstones, however, higher calcium levels [OR=1.3 (1.0-1.9, 95% CI), P=0.04] but not the low phosphate [OR=1.1 (0.6-1.5, 95% CI), P=0.6] were associated with high chance of pancreatitis while high PTH levels [OR=0.9 (0.90-0.99, 95% CI), P=0.02] was found to be protective factor for pancreatitis.
Effect of curative parathyroidectomy on gastrointestinal manifestations: Seven days post curative parathyroidectomy, mean serum calcium, phosphate and PTH levels were 8.9±1.4 mg/dl, 2.9±0.8 mg/dl and 84.7± 11.9 pg/ml, respectively. Three months post curative parathyroidectomy, persistent or recurrent symptoms and signs were as follows; abdominal pain, anorexia and acid peptic disease like symptoms were noted in two cases each, nausea and/or vomiting in four. Of the 27 patients with pancreatitis and PHPT, 23 had no recurrence of pancreatitis after mean follow up of 3.7 years of successful parathyroidectomy, two patients had recurrence of pancreatitis; probably attributed to severe calcification involving the pancreatic ducts as well as parenchyma and two patients died due to obstructive uropathy leading to end stage renal dysfunction.
Discussion
This study reports higher prevalence of gastrointestinal symptoms among patients with symptomatic PHPT. Gallstone disease was more common in women while pancreatitis was more common in men. In majority of patients, gastrointestinal symptoms resolved within three months after successful parathyroidectomy. Pancreatitis did not re-occur after successful parathyroidectomy in majority (85%) of patients.
The women: men ratio was 7:3 with mean age of 39.2 ± 13.9 yr at the time of diagnosis. All PHPT patients were symptomatic. These findings are in consonance with other studies from India suggesting that Indian PHPT patients are younger at the time of diagnosis and have symptomatic disease compared to PHPT patients in western countries1011. The possible reason for more severe and symptomatic PHPT in our study may be due to a delay in diagnosis as evident from lag time (between symptoms suggestive of PHPT and diagnosis of PHPT) of 46.3 ± 39.9 months.
The most common gastrointestinal symptoms were abdominal pain and constipation in this study. High incidence of abdominal pain was noted by us10 and others13 previously in small number of PHPT subjects. The most common digestive symptom noted was constipation in earlier studies1314. However, one study from western India reported absence of gastrointestinal symptoms15. These differences in symptomatolgy are due to difference in number of subjects, population and retrospective design of these studies.
Various mechanisms have been proposed for abdominal pain in patients with PHPT like nausea and/or vomiting, dyspepsia, referred pain due to renal colic, symptomatic gallstone and pancreatitis. Anorexia and nausea/vomiting were present in nearly one third of patients with PHPT. The exact mechanism for nausea and vomiting in PHPT is not known but animal experimentation suggested that it could be because of increased calcium ion concentration in the sympathetic ganglia, impeding transmission of afferent stimuli and diminishing efferent discharges16. Hebert et al17 have shown that the Ca2+-sensing receptor is expressed along the entire gastrointestinal tract and its function was suggested to regulate acid secretion in stomach and fluid secretion in colon. However, we did not find significant difference in the level of serum calcium between patients with and without anorexia, nausea/vomiting and constipation.
High occurrence of gallstone was seen in patients with PHPT and it was more common in women. Gallstones as such are more common in women compare to men18 and that may be the possible reason for higher prevalence of gallstones among women in the present study. Pancreatitis was observed in 18 per cent patients in the study. The prevalence of pancreatitis was reported to be greater in Indian patients with PHPT than those in western countries7101119. Cholelithiasis is a common cause of pancreatitis. However, in this study, gallstones were seen more in women and pancreatitis was higher in men. The reason for this paradox is not known, but this finding implicates that factors other than gallstone are more important for development of pancreatitis in patients with PHPT. High calcium has been implicated in the pathogenesis of pancreatitis but exact mechanism is yet to be elucidated. Plausible mechanisms include calcium-phosphate deposition in the pancreatic ducts; calcium-dependent conversion of trypsinogen to trypsin; increased permeability of pancreatic duct due to hypercalcaemia; and an apparent direct toxic effect of PTH on the pancreas719. A large US population-based study revealed no increase in pancreatitis among PHPT patients8.
We noted the disappearance of gastrointestinal signs and symptoms within three months in majority of patients after successful parathyroidectomy. Chan et al14 also reported significant reduction in symptom rates after parathyroidectomy. The persistent symptoms of nausea, vomiting, fatigue and abdominal pain in a few patients in our study might be explained by concurrent renal stone disease and or renal failure.
In conclusion, this study reveals high frequency of gastrointestinal symptoms in patients with symptomatic PHPT. There was not much gender difference in gastrointestinal symptoms except higher occurrence of gallstones in women and pancreatitis in men. The biochemical profile was also similar in those who had and did not have gastrointestinal symptoms.
References
- Clinical practice. Asymptomatic primary hyperparathyroidism. N Engl J Med. 2004;350:1746-51.
- [Google Scholar]
- Non-classical target organs in primary hyperparathyroidism. J Bone Miner Res. 2002;17(Suppl 2):N117-25.
- [Google Scholar]
- Gastrointestinal symptoms as a clue to the diagnosis of primary hyperparathyroidism: a review of 45 cases. Ann Intern Med. 1957;46:102-18.
- [Google Scholar]
- Analysis of 645 patients with primary hyperparathyroidism with special references to cholelithiasis. Intern Med. 2005;44:917-21.
- [Google Scholar]
- High prevalence of cholelithiasis in primary hyperparathyroidism: a retrospective analysis of 120 cases. Indian J Gastroenterol. 2011;30:100-1.
- [Google Scholar]
- Cholelithiasis in subjects with hypercalcaemia and primary hyperparathyroidism detected in a health screening. Gut. 1977;18:543-6.
- [Google Scholar]
- Does hyperparathyroidism cause pancreatitis? A South Indian experience and a review of published work. ANZ J Surg. 2006;76:740-4.
- [Google Scholar]
- Acute pancreatitis in primary hyperparathyroidism: A population-based study. J Clin Endocrinol Metab. 2009;94:2115-8.
- [Google Scholar]
- Changing biochemical presentation of primary hyperparathyroidism. Langenbecks Arch Surg. 2010;395:925-8.
- [Google Scholar]
- Primary hyperparathyroidism in north India: a description of 52 cases. Ann Saudi Med. 2005;25:29-35.
- [Google Scholar]
- Symptomatic primary hyperparathyroidism: a retrospective analysis of fifty one cases from a single centre. J Assoc Physicians India. 2008;56:503-7.
- [Google Scholar]
- Gastrointestinal manifestations of primary hyperparathyroidism: experience at the Mount Sinai Hospital and review of the literature. J Mt Sinai Hosp NY. 1958;25:339-45.
- [Google Scholar]
- Primary hyperparathyroidism and the gastrointestinal tract. South Med J. 1981;74:197-9.
- [Google Scholar]
- Clinical manifestations of primary hyperparathyroidism before and after parathyroidectomy. A case-control study. Ann Surg. 1995;222:402-12.
- [Google Scholar]
- Clinical profile of primary hyperparathyroidism from western India: a single center experience. J Postgrad Med. 2010;56:79-84.
- [Google Scholar]
- Gastro-intestinal manifestations of hyperparathyroidism. Can Med Assoc J. 1959;81:33-5.
- [Google Scholar]
- Functions and roles of the extracellular Ca2+-sensing receptor in the gastrointestinal tract. Cell Calcium. 2004;35:239-47.
- [Google Scholar]
- Rome Group for the Epidemiology and Prevention of Cholelithiasis (GREPCO). Prevalence of gallstone disease in an Italian adult female population. Am J Epidemiol. 1984;119:796-805.
- [Google Scholar]
- Chronic pancreatitis in primary hyperparathyroidism: comparison with alcoholic and idiopathic chronic pancreatitis. J Gastroenterol Hepatol. 2008;23:959-64.
- [Google Scholar]






