Translate this page into:
Drug resistant Shigella flexneri in & around Dibrugarh, north-east India
Reprint requests: Dr Reema Nath, Associate Professor, Department of Microbiology, Assam Medical College Dibrugarh 786 002, Assam, India e-mail: reema_44@rediffmail.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Shigella flexneri is the most common species of Shigella causing diarrhoea and dysentery in Asia including India. Multidrug resistance in Shigella species has been reported worldwide and there is rising concern regarding development of fluoroquinolone resistance. This study was undertaken to find out the resistance pattern of Sh. flexneri, the commonest shigella isolated in Dibrugarh, north east India, including detection of fluoroquinolone resistance and extended spectrum beta lactamases.
Methods:
Stool samples collected from patients of diarrhoea and dysentery were tested for bacterial enteropathogens. Strains of Shigella species were confirmed by biochemical tests. Speciation was done using commercially available polyvalent antiserum. Antimicrobial susceptibility test was performed by Kirby Bauer disc diffusion method against 18 different antibiotics. Extended spectrum beta lactamase (ESBL) detection was done by disc approximation test as well as combination disc method and minimum inhibitory concentrations (MIC) of different antibiotics were also measured.
Results:
Multidrug resistance in Sh. flexneri was found to be common (90.2%) and the commonest phenotypic multi-drug resistance profile was ampicillin-tetracycline-co-trimoxazole-nalidixic acid. High resistance to nalidixic acid was detected in 90.3 per cent isolates (MIC >240 μg/ml) and ciprofloxacin resistance was seen emerging in this region (11.2%, MIC >4 μg/ml). Present of ESBL was phenotypically confirmed in two cases. Besides the fluoroquinolones, chloramphenicol, piperacillin-tazobactum and the third generation cephalosporins were effective in 87-100 per cent of the isolates.
Interpretation & conclusions:
Our study showed high resistance (MIC >240 μg/ml) against nalidixic acid in Sh. flexneri isolates. Ciprofloxacin resistance is also emerging in this region. Shigellosis due to ESBL carrying Shigella can become a serious threat to public health. Guidelines for therapy should be monitored and modified based on regional reports of resistance to antimicrobial agents.
Keywords
Assam
drug resistance
Shigella flexneri
Shigellosis is an important public health problem, particularly in the developing world. The most important species responsible are Shigella sonnei in Europe and US and Sh. flexneri in Asia and Africa1. Antimicrobial therapy is given in most cases to curtail the duration of illness1. Shigella species represent one of the growing numbers of antimicrobial-resistant bacteria in developing countries2. Earlier ampicillin, co-trimoxazole, chloramphenicol and nalidixic acid were used worldwide for empirical treatment of shigellosis. But due to emergence of different degrees of resistance in different parts of the world to these drugs, the World Health Organization (WHO) has recommended that ciprofloxacin should be considered as the first line antibiotic for the treatment of shigellosis, and the use of nalidixic acid is not encouraged even in areas where it is still effective against Shigella3. But ciprofloxacin resistant Shigella isolates have been reported from different parts of India2. Therefore, treatment options are becoming limited. The use of third generation cephalosporin is also increasing day by day in cases of multiresistant Shigella infection specially in paediatric cases where ciprofloxacin is used with caution due to the adverse effects and in adult cases found to be resistant to fluoroquinolones. This increases the possibility of emergence of extended spectrum beta lactamase (ESBL) producing Shigella species. In comparison to the studies on ciprofloxacin resistance, the studies on ESBL producing Shigella from India are only a few45. This study was carried out to determine the susceptibility pattern of Sh. flexneri isolates as also detection of ESBL in a tertiary level hospital from sporadic cases occurring in and around Dibrugarh, situated in eastern part of Assam.
Material & Methods
This prospective study was carried out in the department of Microbiology, Assam Medical College, Dibrugarh, India. All consecutive samples of stool from diarrheoa and dysentery cases sent to the department of microbiology during January 2008 to November 2010 were included in the study. All bacterial enteropathogens were looked for using standard protocol6. Of the 1411 stool samples tesed, 71 isolates of Shigella were obtained. Isolates were confirmed as Shigella by standard biochemical tests6 and speciation was done using commercially available polyvalent antisera (Denka Seikan, Japan). Antimicrobial susceptibility tests were performed by Kirby Bauer disc diffusion method in accordance with Clinical Laboratory Standards Institute guidelines7 for ampicillin (10 μg), co-trimoxazole (25 μg), tetracycline (30 μg), chloramphenicol (30 μg), nalidixic acid (30 μg), ciprofloxacin (5 μg), norfloxacin (10 μg), ofloxacin (5 μg), ceftriaxone (30 μg), azithromycin (15 μg), cefotaxime (30 μg), imipenem (10 μg), gentamycin (120 μg), amikacin (30 μg), amoxicillin-clavulanic acid (10 μg), ampicillin-sulbactum (10/10 μg) and furazolidone (50 μg) and piperacillin-tazobactum (100/10 μg) (Hi-media, Mumbai, India). Escherichia coli ATCC25922 was used for quality control in each batch of test. Minimum inhibitory concentrations (MIC) were determined for nalidixic acid, ciprofloxacin, ofloxacin, norfloxacin, chloramphenicol and azithromycin by (Hi comb, Hi-media, Mumbai). The results of minimum inhibitory concentrations determined by Hi comb were not used to analyse the findings of this study as Hi comb is not yet a recommended method by CLSI. ESBL was detected578 by CLSI phenotypic confirmatory tests by the disc approximation test and combination disc method78; MICs to different antibiotics were determined in ESBL producers by Sensititre® (TREK diagnostic systems, Magellan Biosciences, Cleveland, Ohio, USA)8. Mueller-Hinton agar plates (Difco, USA) were used for susceptibility testing. In the disc approximation test, a disc containing amoxicillin- clavulanic acid was placed and cefotaxime, ceftriaxone or ceftazidime discs were placed at 30 mm distance on a lawn culture of the organism. An increased zone of inhibition towards the clavulanic acid disc was taken as positive for ESBL. For the combination disc method78, disks containing 30 μg of ceftazidime or cefotaxime, with and without 10 μg of clavulanic acid were used. A 5 mm increase in zone diameter for ceftazidime or cefotaxime tested in combination with clavulinic acid versus its zone when tested alone was considered indicative of ESBL production. E. coli ATCC25922 and Klebsiella pneumoniae ATCC 700603 were used as quality reference strains.
Results & Discussion
Of the 1411 stool samples tested, Shigella species was isolated in 71 cases (5.03%). Sh. flexneri was the predominant serotype (87.3%, n=62) and others were Sh. dysenteriae (6 isolates, 8.45%) and three (4.22%) non agglutinable but biochemically confirmed Shigella species. Sh. flexneri were isolated from patients of all ages groups ranging from 0-80 yr (Table I).

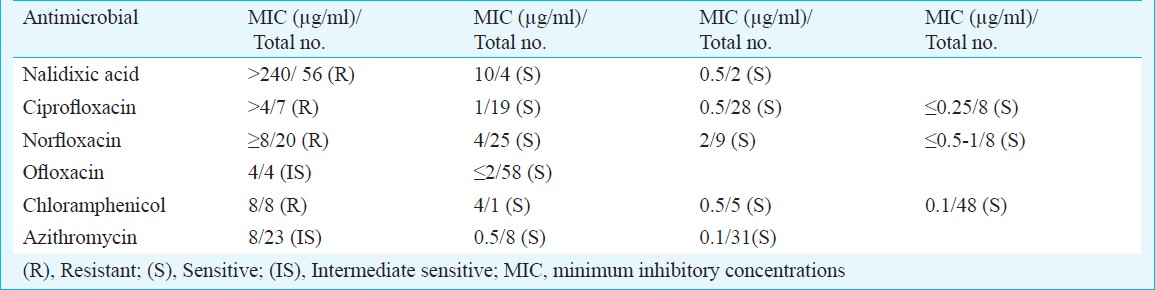
Resistance to nalidixic acid was high (90.3%, n=56/62) and the MIC was >240 μg/ml. Ciprofloxacin resistance was low but slowly emerging (11.2%, n=7/62). In these ciprofloxacin resistant isolates, the MIC was >4 μg/ml. One of these isolates showed high MIC to nalidixic acid (>240 μg/ml), ofloxacin (4 μg/ml) and norfloxacin (>8 μg/ml). All these isolates were sensitive to chloramphenicol, azithromycin, ceftriaxone and cefotaxime. Twenty isolates (32.3%) showed MIC of norfloxacin >8 μg/ml, four (6.5%) had ofloxacin MIC >4 μg/ml; eight (12.8%) had chloramphenicol MIC > 8 μg and 23 (37%) had azithromycin MIC >8 μg/ml. Multidrug resistance (MDR) (resistance to more than 4 antibacterials) was found in 90.2 per cent isolates and the most common MDR profile was ampicillin, nalidixic acid, tetracycline, co-trimoxazole. Sensitivity to different antibiotics tested were, ampicillin 6.4 per cent (n=4), azithromycin 62.9 per cent (n=39), ampicillin-sulbactum 67.7 per cent (n=42), amoxiclav 79 per cent, (n=49), piperacillin-tazobacturm 100 per cent (n=62), furazolidine 74.1 per cent (n=46), tetracycline 4.8 per cent (n=3), amikacin 85.4 per cent (n=53), gentamicin 77.4 per cent (n=48), co-trimoxazole 8 per cent (n=5), chloramphenicol 87.1 per cent (n=54), ciprofloxacin 88.7 per cent (n=55), norfloxacin 67.7 per cent (n=42), ofloxacin 93.5 per cent (n=58), ceftriaxone and cefotaxime 95.1 per cent each (n=59) and imipenem 100 per cent (n=62). Two isolates were phenotypically confirmed to be ESBL producers, and were sensitive to ciprofloxacin, ofloxacin, azithromycin, chloramphenicol and imipenem, ciprofloxacin and chloramphenicol.
MICs (μg/ml) were ampicillin (256), aztreonam (1), ceftazidime (1), imipenem (<0.5), meropenem (<1), cefotaxime (32 and 64), ceftriaxone (256), amoxycillin-clavulanate (4), cefoxitin (<4), cephalothin (>16), and ampicillin-sulbactum (8 and 12), piperacillin-tazobactum (4), ceftazidime-clavulinic acid (0.25), cefotaxime-clavulinic acid (4 and 8). The two ESBL producers were resistant to ampicillin (MIC >256 μg/ml), cefotaxime (MIC >64 μg/ml), ceftazidime (MIC >2 and 8 μg/ml), aztreonam (MIC >4 μg/ml). The MICs for amoxicillin-clavulanate were 4 and 8 μg/ml, respectively and for pipercillin-tazobactum was 1 μg/ml.
Shigellosis is endemic in India. The isolation rate of Shigella varies from 2-6 per cent in different studies across India9–11. S. flexneri was found to be the most prevalent serogroup (87.3%) in our study similar with other studies from India912.
Analysis of antibiotic resistance revealed a high degree of resistance to the drugs used empirically for treatment of shigellosis and other diarrhoeal diseases like ampicillin, tetracycline, co-trimoxazole and nalidixic acid. Another drug once used for empirical treatment of shigellosis, chloramphenicol was found to be effective in 87 per cent isolates in our study as against 88 per cent of ciprofloxacin. The use of chloramphenicol for enteric infections was long abandoned in this region, once quinolone antibiotics were introduced. Resistance to the nalidixic acid was recorded in 90.3 per cent cases with very high MIC of >240 μg/ml. Similar finding have been reported earlier from India910. Resistance to ciprofloxacin was seen in seven cases (MIC >4 μg/ml). In other cases lowered susceptibility to ciprofloxacin (MIC between 0.25 and 0.5 μg/ml) along with nalidixic acid resistance was observed. As fluoroquinolones are used extensively in the treatment of diarrhoea, dysentery and other infectious diseases empirically, the resistance to this group of drugs is slowly emerging. Ciprofloxacin is being used in empirical treatment of dysentery cases, there is a possibility of increasing its resistance to a higher level in near future. Srinivasa et al12 reported susceptibility of Shigella isolates to neomycin and furazolidine along with ceftriaxone. Azithromycin has also shown promise in treatment of shigellosis13. In our study chloramphenicol, piperacillin-tazobactum, and the third generation cephalosporins were effective for more than 87-100 per cent cases.
Shigellosis due to ESBL carrying shigellae can become a serious threat to public health. ESBL was reported in Sh. dysenteriae in Kolkata in 19994. ESBL carrying Shigella species are recently being reported from different parts of the world514–16. In one recent study from Punjab, India, ESBL was reported in Sh. flexneri and Sh. boydii isolates5.
In conclusion, shigellosis due to Sh. flexneri is an important public health problem in Assam. Emerging resistance to empirically used drug ciprofloxacin and emerging ESBL in Shigella species can be a problem in near future. Treatment guidelines should be decided and monitored at the national level to check these emerging resistances. Chloramphenicol, piperacillin-tazobactum, and newer cephalosporins can become treatment options in this region after susceptibility test. Regular monitoring of susceptibility pattern locally including detection of common beta-lactamases need to be done in public health laboratories.
References
- Molecular characterization of multidrug-resistant Shigella species isolated from epidemic and endemic cases of shigellosis in India. J Med Microbiol. 2008;57:856-63.
- [Google Scholar]
- WHO. International note on antibiotics in the management of shigellosis. Wkly Epidemiol Rec. 2004;79:202-3.
- [Google Scholar]
- Molecular characterization of the SHV-11 Beta lactamase of Shigella dysenteriae. Antimicrob Agents Chemother. 1999;43:2081-3.
- [Google Scholar]
- Extended spectrum beta-lactamase production in Shigella isolates - A matter of concern. Indian J Med Microbiol. 2011;29:76-8.
- [Google Scholar]
- WHO. In: Manual for laboratory investigations of acute enteric infections. Geneva, Switzerland: World Health Organization; 1983. WHO CDD/83.3
- [Google Scholar]
- National Committee for Clinical Laboratory Standards (NCCLS) In: Performance standards for antimicrobial susceptibility testing. Approved Standards (14th ed). Villanova, PA: NCCLS; 2004. Document M100-S14
- [Google Scholar]
- National Committee for Clinical Laboratory Standards (NCCLS) In: Performance standards for antimicrobial disc susceptibility testing. Wayne Pa: NCCLS; 1998. 8th informational supplement. M-100-58
- [Google Scholar]
- Changing epidemiology of shigellosis and emergence of ciprofloxacin resistant Shigellae in India. J Clin Microbiol. 2007;45:678-9.
- [Google Scholar]
- Changing patterns of antimicrobial susceptibility of Shigella serotypes isolated from children with acute diarrhea in Manipal, South India, A five tear study. Southeast Asian J Trop Med Public Health. 2007;38:863-6.
- [Google Scholar]
- Magnitude of drug resistant Shigellosis: A report from Bangalore. Indian J Med Microbiol. 2009;27:358-60.
- [Google Scholar]
- Treatment of shigellosis: V. comparison of azithromycin and ciprofloxacin. A double blind randomized, controlled trial. Ann Intern Med. 1997;126:697-703.
- [Google Scholar]
- SHV-type extended-spectrum β-lactamase in a Shigella flexneri clinical isolate. J Antimicrob Chemother. 2001;47:685-8.
- [Google Scholar]
- Extended spectrum beta lactamase mediated third generation cephalosporin resistance in Shigella isolates in Bangladesh. J Antimicrob Chemother. 2004;54:846-7.
- [Google Scholar]
- CTX-M3 type beta lactamase producing Shigella sonnei isolates from paediatric bacillary dysentery cases. Jpn Infect Dis. 2008;61:135-7.
- [Google Scholar]






