Translate this page into:
Costing analysis of an information & communications technology-enabled primary healthcare facility in India
For correspondence: Dr Dharamjeet Singh Faujdar, Department of Community Medicine, Armed Forces Medical College, Pune 411 040, Maharashtra, India e-mail: vintoof5@yahoo.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Information and communications technology (ICT) has often been endorsed as an effective tool to improve primary healthcare. However, evidence on the cost of ICT-enabled primary health centre (PHC) is lacking. The present study aimed at estimating the costs for customization and implementation of an integrated health information system for primary healthcare at a public sector urban primary healthcare facility in Chandigarh.
Methods:
We undertook economic costing of an ICT-enabled PHC based on health system perspective and bottom-up costing. All the resources used for the provision of ICT-enabled PHC, capital and recurrent, were identified, measured and valued. The capital items were annualized over their estimated life using a discount rate of 3 per cent. A sensitivity analysis was undertaken to assess the effect of parameter uncertainties. Finally, we assessed the cost of scaling up ICT-enabled PHC at the state level.
Results:
The estimated overall annual cost of delivering health services through PHC in the public sector was ₹ 7.88 million. The additional economic cost of ICT was ₹ 1.39 million i.e. 17.7 per cent over and above a non-ICT PHC cost. In a PHC with ICT, the cost per capita increased by ₹ 56. On scaling up to the state level (with 400 PHCs), the economic cost of ICT was estimated to be ₹ 0.47 million per year per PHC, which equates to approximately six per cent expenditure over and above the economic cost of a regular PHC.
Interpretation & conclusions:
Implementing a model of information technology-PHC in a state of India would require an augmentation of cost by about six per cent, which seems fiscally sustainable. However, contextual factors related to the availability of infrastructure, human resources and medical supplies for delivering quality PHC services will also need to be considered.
Keywords
Costing analysis
eHealth
information and communications technology
integrated health information system for primary healthcare
primary healthcare
After the declaration of Sustainable Development Goals1, primary healthcare has again come into focus in low- and middle-income countries (LMICs) which are struggling with the challenge of providing high-quality, people-centred services at an affordable cost2. In most of these countries, universal health coverage (UHC) goals have set important benchmarks on health and well-being to promote evidence-based, rational and proactive responses to health needs and social expectations3. In this endeavour, integrating information and communications technology (ICT) in primary health centre (PHC) is expected to accelerate progress by catalyzing access to services and information and supporting efficient care4.
In 2005, the World Health Assembly (WHA)5 acknowledged that ‘eHealth is the cost-effective and secure use of information and communications technologies in support of health and health-related fields’. Therefore, the WHA urged the member states to develop and implement eHealth technologies5. It is expected that eHealth solutions for primary healthcare will empower patients, maintain or improve health outcomes, reduce the workload of primary healthcare professionals and generate cost-effective gains. However, while implementing eHealth in PHC, technical infrastructure, the eHealth intervention function, its usability and financial aspects need to be considered6.
The Indian Government is committed to UHC. Hence, strengthening primary healthcare services is required. Information technology (IT) support is envisaged to play an important role in it. The automation of many national health programmes and health management information system (HMIS) has already been carried out7. However, there is still a felt need to have an ICT-supported people-centric primary healthcare system which can meet the primary healthcare needs of the community. To meet this requirement, an integrated health information system for primary healthcare (IHIS4PHC) was developed and implemented at a PHC as a pilot and an evaluation showed significant improvement in many of the selected health indicators8.
Several other studies have also shown that IT use in healthcare can improve the quality of care, but none of these studies provided the costs incurred to achieve the desired results9. The cost of eHealth interventions is required to estimate the net economic effect10. In the absence of an economic evaluation of eHealth implementation, it is difficult to reach investment decisions in LMICs11,12.
Although a few studies have provided the implementation cost of PHC, majority of these studies on the costing of primary healthcare have been undertaken in settings which did not have eHealth initiatives13-17. The national health system cost database also does not contain estimates of the cost of eHealth initiatives in primary healthcare18. Whatever estimates are available, are for focal interventions rather than system-level reform in the use of IT for delivering primary healthcare19,20. The Health Technology Assessment Board in India places greater emphasis on providing information on value for money for new interventions before these are incorporated into the programme. However, the starting point of such an evaluation is the assessment of the incremental cost of the new intervention. In view of this gap in existing evidence, the present study was carried out to estimate the costs that will be required for developing an IHIS4PHC for creating a fully operational IT-enabled primary healthcare facility.
Material & Methods
The study was carried out at the department of Community Medicine & School of Public Health, Postgraduate Institute of Medical Education & Research (PGIMER), Chandigarh, India. The study was approved by the Institutional Ethics Committee, vide their letter no. INT/IEC/2017/195.
An integrated health information system for primary healthcare (IHIS4PHC) was developed and implemented in a public sector urban primary healthcare facility catering to about 25,000 population in a resettlement colony of Chandigarh (India), using open and free source software21, i.e. District Health Information System 2 (DHIS2) and OpenMRS (Medical Record System). In view of the availability of the infrastructure required for converting a PHC into an ICT-enabled centre, an urban PHC (UPHC) located in Sector 25, Chandigarh, was purposively selected for piloting the IHIS4PHC application. This facility was under the administrative control of the Chandigarh Union Territory health services but was being managed by the staff of PGIMER, Chandigarh. In conformance with the Government of India policy, free and open-source software were used for the development of the IHIS4PHC application, so that the end user can access and modify source code if needed and vendor lock-in can be avoided. The open-source software have also been claimed to have better modularity and interoperability than closed-source software21. The IHIS4PHC system was customized to the needs of primary healthcare which included creation of an electronic family folder having demographic details of each family member and enrolling them into various national health programme’s modules. It covered all aspects of preventive, promotive and curative care (e.g. antenatal care, immunization, TB, malaria and hypertension treatment).
The IHIS4PHC had data of 22,353 population, which was used in the outpatient clinic (electronic health record system for tracking of patients), national health programmes, inventory management, registration, work plan preparation and aggregate report generation and for sending short message service (SMS) for appointment reminders and health education8.
Costing of the primary healthcare facility and eHealth component was undertaken from a health system perspective using bottom-up approach22. A health system perspective was used, as almost all costs related to the IHIS4PHC intervention are likely to be borne by the government or the health system. A bottom-up approach was used as it provides a more accurate estimation of costs by comprehensively covering the costs of each component in a detailed manner23. All resources consumed by the health system for converting a normal PHC into an ICT-enabled PHC were identified, measured and valued. The costing estimates were based on (a) actual cost that was incurred on various components of the primary healthcare facility in one complete financial year, and (b) the cost of creating ICT infrastructure, customization and maintenance of software. The capital cost, which included the cost of equipment, furniture and software customization was annualized for their expected lifetime. The recurring cost comprised estimated rental of building, consumables, salaries, electricity and water. A discount rate of three per cent was considered during costing analysis to provide for the valuation of costs overtime and also to account for opportunity costs (Supplementary Box I). The study was conducted for two months from July to August 2018 with cost estimates obtained for the reference period from April 1, 2017 to March 31, 2018.
The data for costing were collected through a checklist from all the persons employed at PHC giving details of their employment at PHC (full-time or part-time), salaries received and the type and volume of services provided by them during the reference period (Supplementary Table). The information on services provided through PHC and the salaries of employees were cross-checked through facility registers and the salary slips of the employees, respectively. A facility survey was undertaken to assess the capital infrastructure and recurrent costs. All capital and recurrent costs associated with the day-to-day functioning of the PHC including that of human resources (HR), equipment, consumables and overhead charges (electricity, water, internet and SMS service) during the reference period were included for costing.
| Serial number | Designation | Work schedule | n | Full-time equivalent (routine) | Full-time equivalent (IT set-up) |
|---|---|---|---|---|---|
| Already existing staff in PHC | |||||
| 1 | Senior medical officer | Full time | 1 | 1 | 1 |
| 2 | Junior medical officer | Part time | 1 | 0.75 | 0.75 |
| 3 | Multi-purpose worker cum medicine dispenser | Full time | 1 | 1 | 1 |
| 4 | Auxiliary nurse midwives | Full time | 5 | 1 | 1 |
| 5 | Sanitation worker | Full time | 1 | 1 | 1 |
| 6 | Medical social worker | Part time | 1 | 0.5 | 0.5 |
| 7 | Public health nurse | Part time | 1 | 0.5 | 0.5 |
| 8 | Accredited social health activist | Part time | 4 | 0.25 | 0.25 |
| 9 | Lab technician | Part time | 1 | 0.4 | 0.4 |
| 10 | Lab technician (State AIDS Control Society) | Part time | 1 | 0.2 | 0.2 |
| 11 | Lady health visitor | Part time | 1 | 0.2 | 0.2 |
| Additional staff employed for supporting computerization of the PHC | |||||
| 1 | Junior software developer | Full time | 1 | 0 | 1 |
| 2 | Data entry operator | Full time | 1 | 0 | 1 |
PHC, primary health centre; IT, information technology
The data were divided into two parts: the first part involved the costing of primary healthcare facility, and the second part consisted of the costing of eHealth system.
Costing of primary healthcare facility: Standard tools for data collection, used in the costing of primary- and secondary-level health facilities in India, were utilized24. The cost of HR salaries (derived from payslips of employees) was apportioned for individual services as per the time spent on PHC work. The prices of equipment, furniture and consumables were derived from government procurement prices of the product or through an online search of the item cost where procurement price details were not available. The rates of Jan-Aushadi (Public-Medicine) store were used for the costing of drugs, and market rates were obtained when the drug/vaccine rates were not available through Jan-Aushadi. The Central Government Health Scheme (CGHS) rates were used for the costing of laboratory investigations. The quantity of resources consumed such as drugs, syringes, vaccines, contraceptives and testing kits was obtained from the inventory records available in the primary healthcare facility. The actual bills of electricity and water consumption at the primary healthcare facility for the last one year were obtained from the Municipal Corporation of Chandigarh. The cost of equipment and furniture was annualized as per the expected life of the equipment at a discount rate of three per cent to determine per annum cost. The prevailing rental rates (per square feet) for the building space, in the area where the primary healthcare facility was located, were applied to determine the capital cost of the PHC facility building. The register entries of the cash benefits paid to the patients and accredited social health activist (ASHA) incentives in the last one year were also added in the cost of the primary healthcare facility.
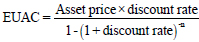
Costing of eHealth system: Inception to full customization of the software (DHIS2 and OpenMRS) into IHIS4PHC took around 11 months (February to December 2017). The cost of additional HR employed on ad hoc basis (one data entry operator and one junior software developer) to make up for the deficiency in HR and extra workforce needed to run the ICT-enabled PHC was also estimated. The HR wages for ad hoc employees were based on Deputy Commissioner’s notification for minimum wages in Chandigarh. The customization cost of software included apportioned value of salaries of the personnel involved in the customization of software (public health expert, project lead, system administrator, software developer, implementor, HMIS consultant and public health consultant), as well as the cost of workshops, informal meetings, travel cost and training cost of full-time employees. Internet charges were obtained from Bharat Sanchar Nigam Limited. For assumptions regarding the requirement of cloud services on scaling up scenario, the rental rates were obtained from National Informatics Centre’s cloud services providing Infrastructure as a Service (IaaS). Prior to customization only one desktop and a printer was available with the PHC, the details of required IT equipment for full computerization of the PHC are provided (Supplementary Box IA). The IT equipment (desktop and laptop computers, router, switch box and printers) procurement price was the actual price spent for their purchase. Availability of these items was searched online, and the lowest priced items meeting the technical requirement were purchased. The cost of IT equipment and furniture required for ICT set up was annualized as per the expected life of equipment and furniture, discounting at three per cent per year. Extra space created for IT set-up was estimated, and its cost as per rental rates was added up in the capital cost to account for the opportunity cost of space. The quantity of consumables (cartridges, stationery, etc.) was obtained for the last one year. The overhead costs due to added electricity bill (average increase in electricity bill from the time when the eHealth system was not implemented), internet and SMS service were also included. The schematic flow chart of cost heads is shown in Figure 1.
| Server: 1 |
| Laptops (5) and desktops (3) |
| 2×doctors |
| 1 each for DEO, lab/MPW and software developer/system manager |
| 3×desktops at registration, Triage (measurement of vitals and entry in EHR) and with ANMs for record keeping and MIS report generation) |
| Printers (3) |
| 2×printers with doctors for issuing prescription |
| 1×ANM for generation of reports |
| Invertor (3KVA) with batteries for uninterrupted electricity supply to server, computers and printers |
| Air conditioner (1) for server room |
| Switchboard and Lan installation |
| Assumption for cost calculation |
| Software development cost |
| Total cost incurred on development of Software was Rs. 2,642,097, while based of assumed software life, equivalent uniform annual cost for software was calculated as Rs. 542,444/year (The software IHIS4PHC is assumed to have life of 10 yr) |
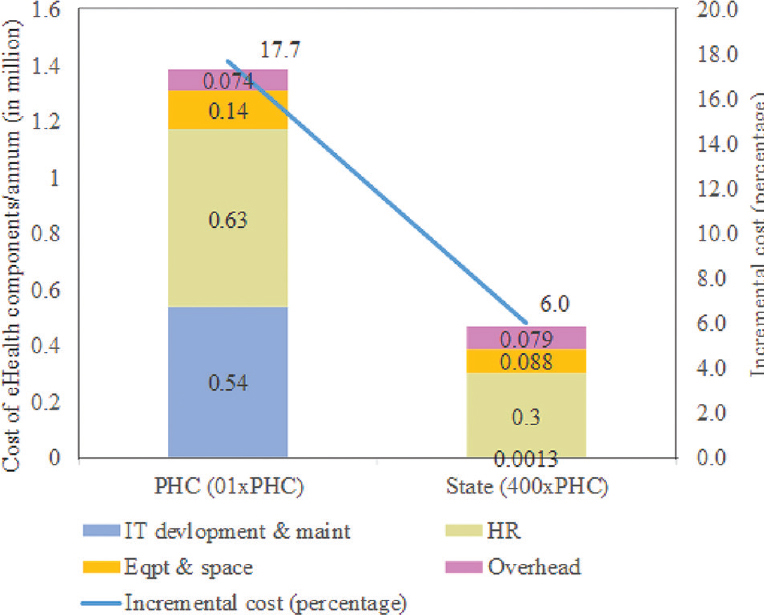
| EUAC calculated as=EUAC (capital) + (annual maintenance cost) where |
 |
| (Discount rate of 3% was considered for EUAC calculation and annual maintenance cost as 10% of development cost was added to it to arrive at total EUAC) |
| Equipment/furniture cost |
| Similarly individual EUAC costs for equipment used in PHC facility were calculated based on the expected life of each equipment (e.g., laptop life was taken as five years) and annual maintenance cost (5% of equipment cost) added to it |
| Capital costs |
| Capital cost was calculated as rental cost of the building and cost of additional space (80 sq ft) required for installing server, switchbox and providing work place for developer/technical assistant |
| Other costs |
| Costs of drugs, consumables, laboratory investigation, IEC material development and overhead (electricity, water) were based on the actual costs incurred in last one year by the PHC |
| The added electricity and Internet charges due to ICT inclusion in PHC were calculated separately (i.e., electricity bill received before and after ICT inclusion and actual Internet charges paid after ICT inclusion at PHC) |
EUAC, equivalent uniform annual cost; PHC, primary health centre; ICT, information and communications technology; IEC, information education communication; MIS, management information system; EHR, electronic health record; IHIS4PHC, integrated health information system for primary healthcare; ANM, auxiliary nurse midwife; MPW, multi-purpose worker; DEO, data entry operator.
- A schematic flow diagram of cost heads of IT-enabled PHC. PHC, primary health centre; IT, information technology
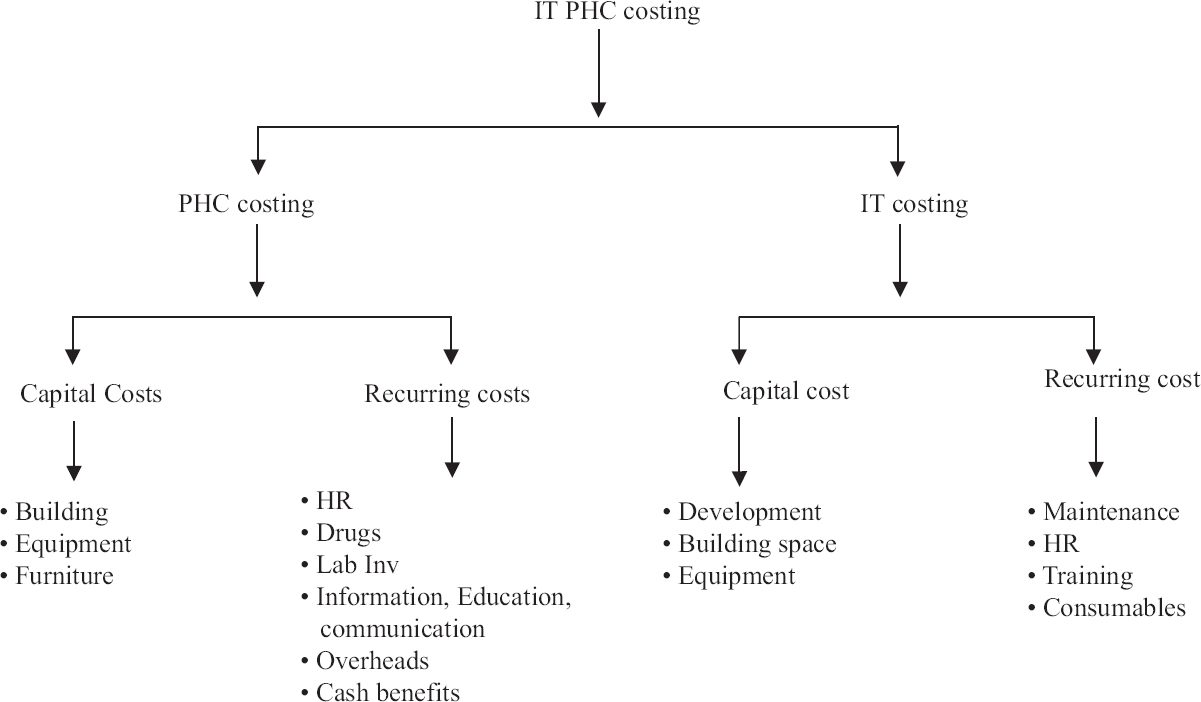
Sensitivity analysis: The sensitivity analysis was carried out to account for uncertainties in the assumptions regarding inputs (HR, equipment, customization and maintenance costs), prices and discount rates25. The costs involved were kept at minimum considering the resource-constraint setting of the primary healthcare facilities in India; however, based on expert advice, sensitivity analysis was undertaken for variation in costs from minus 20 per cent to plus 100 per cent for overall cost and similarly for each major costing head. The difference between lower and upper bound was based on the argument that for the current eHealth system, the costs were kept as minimal as possible considering the resource-constraint environment but not compromising the quality.
Per capita cost: An estimate of per-capita cost was arrived at by dividing the total cost of primary healthcare facility and ICT-enabled primary healthcare facility by the total population served by the health facility.
Scaling up costs: The estimation of cost due to scaling of IHIS4PHC to all government primary healthcare facilities up to the state level was also done. The change in ICT infrastructure and human resource requirement with scaling up like moving the ICT applications from local server to the cloud and for sharing of human resources, e.g. that of software developers, was suitably factored in the scale-up estimation. Various assumptions for scaling up of ICT-enabled PHC facility are provided in Supplementary Box I.
| Scaled to State Level |
| Assumed 400× PHCs in a State |
| Application will be moved to NIC’s cloud, no server required |
| At least 02× IT professional will be needed at state level |
| Data managers (IT) required in each district (a total of 24) |
| Additional space required only at State level office for IT professional |
| Software development cost shared between 400× PHCs |
| Requirement of hardware 04× laptop and 03× desktop at each PHC, additional laptop to be catered for IT professionals and data managers |
| All computers will have password-protected restricted access and anti-malware antivirus will be installed |
IT, information technology; PHC, primary health centre; NIC, National Informatics Centre
Statistical analysis: The statistical analysis of costing data for apportioning, equivalent uniform annual cost, sensitivity analysis and scaling costs was done using Microsoft Excel, version 2016.
Results
The annual cost of primary healthcare facilities was estimated as ₹ 7.88 million. The overall initial financial cost of ICT component was ₹ 3.09 million (customization cost ₹ 2.64 million + hardware and furniture cost ₹ 0.45 million). After the annualization of the above ICT component cost, and the addition of the annual maintenance and recurrent costs, the annual cost of adding an ICT component to the existing PHC was ₹ 1.39 million. Thus, the total economic cost of ICT-enabled primary healthcare facilities was ₹9.28 million per year. The incremental cost that has to be incurred annually on ICT-enabled primary healthcare facilities was 17.7 per cent.
In the sensitivity analysis, on varying the costs from minus 20 per cent to plus 100 per cent, the incremental cost of the ICT component varied from 14.1 to 35.2 per cent. If the variation is considered in only human resource cost, then the incremental cost varied from 16 to 25.7 per cent, whereas if the variation is considered only for customization and maintenance cost, the incremental cost varied from 16.2 to 24.1 per cent, and if only equipment cost is taken into consideration, the incremental cost varied from 17.3 to 19 per cent (Fig. 2).
- Sensitivity analysis of ICT-enabled PHC costing. PHC, primary health centre; ICT, information and communications technology
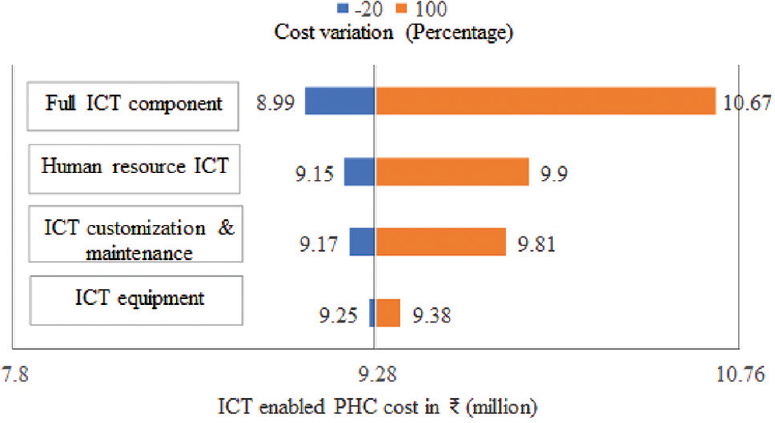
The share of capital cost in the ICT component cost was 48.9 per cent (₹ 0.68 million), of which 80 per cent (₹ 0.54 million) was spent on ICT system customization and maintenance. For the annualization of ICT system cost, the annual maintenance cost (ten per cent) was also added to the customization cost. The share of the recurrent cost was 51 per cent (₹ 0.71 million) of which 89 per cent (₹ 0.63 million) had to be spent on salaries of ICT staff (one junior software developer and one data entry operator) (Table).
| Cost head | Cost (₹ in million) | ||
|---|---|---|---|
| Health facility | ICT component | Total | |
| Capital items | |||
| Building/space | 0.66 | 0.029 | 0.69 |
| Furniture | 0.056 | 0.0018 | 0.058 |
| Equipment | 0.052 | 0.108 | 0.16 |
| IT development and maintenance* | 0 | 0.54 | 0.54 |
| Total | 0.77 | 0.68 | 1.45 |
| Recurrent items | |||
| Human resources# | 4.64 | 0.64 | 5.28 |
| Drugs | 0.73 | 0 | 0.73 |
| Consumables | 0.34 | 0.0025 | 0.34 |
| Lab investigations | 0.32 | 0 | 0.32 |
| Overheads | 0.091 | 0.074 | 0.16 |
| IEC materials | 0.026 | 0 | 0.026 |
| Cash benefits paid | 0.96 | 0 | 0.96 |
| Total | 7.11 | 0.71 | 7.82 |
| Total capital + recurrent | 7.88 | 1.39 | 9.28 |
*Annual maintenance cost of software was kept as 10% of development cost; #ICT component includes salaries of one Software developer and one data entry operator. ICT, information and communications technology; IT, information technology; IEC, information education communication
On analysis of the PHC per annum cost and population served by the PHC, the cost per capita was estimated as ₹ 315. Following the implementation of the eHealth system, the estimates of cost per capita were found to increase by ₹ 56.
Estimates of the economic cost (annualized ICT component cost, annual maintenance and recurrent costs) of scaling up indicated that with ICT component scaled up to the state level, the ICT implementation costs would reduce to ₹ 0.47 million (6% of PHC cost per annum; Fig. 3).
- Costing of eHealth component on scaling.
The reduction in costs in scaling up is mainly due to sharing of customization and maintenance cost which comes down from ₹ 0.54 million for one PHC to ₹ 1,356 for 400 PHCs in the state. The human resource cost gets reduced almost by 52.6 per cent, if scaled to the state level as data managers and software developers will be needed at the district or state level only. However, a data entry operator or technical assistant will be needed for each PHC facility. In the scaling up, additional cost saving will occur when the software application is shifted from the local server to the cloud. This change will lead to a reduction in costs under the equipment head. However, overhead costs will slightly increase because of the cost of cloud rental (Fig. 3).
Overall, at least ₹ 0.47 million per annum will be required per PHC facility to implement and maintain IHIS4PHC when it is scaled up in all PHC facilities of the state. In this scenario, annualized capital cost will be ₹ 0.09 million per PHC facility and the recurring cost will be ₹ 0.38 million per annum per PHC facility.
Discussion
Information and communications technology (ICT) is being increasingly seen as a potential tool to strengthen primary healthcare by providing integrated, coordinated, continuous, holistic, patient-centric and cost-effective healthcare with improved access. The impact of ICT implementation at the UPHC was evaluated through a quasi-experimental study in Chandigarh, and significant improvements were observed in the adequacy of primary healthcare delivery, treatment seeking for chronic illness and in some of the selected tracer conditions8. However, despite emerging evidence on ICT-led improvement in health services, policymakers may require estimation of the cost of ICT implementation in health system as the same can be used for planning the scaling up of eHealth intervention.
So far very few economic evaluations of eHealth systems have been conducted26. Cost analysis of the ICT-enabled PHC in the urban community of Chandigarh indicated that an incremental cost of 17.7 per cent would be required per annum over and above the existing cost of primary healthcare facility (₹ 7.88 million). The cost per capita was found to be increased by ₹ 56 after the implementation of the ICT component.
Krishnan et al20 in their study have estimated the annual cost of computerization of health management information system (HMIS) of PHCs at Ballabgarh, India, to be ₹ 0.24 million (capital cost, maintenance and consumables) at 2008 rates. Whereas in the present study for capital, maintenance and consumables, the estimated cost was ₹ 0.76 million at 2018 rates. The higher cost was due to time-based inflation, and the comprehensiveness of ICT components which in addition to HMIS also included an electronic health record system, inventory management and SMS service, etc., requiring more intricate customization, maintenance and additional hardware.
The per annum costs estimated in our normative primary healthcare facility were similar to the study conducted by Prinja et al15 in North India, whereas the per capita cost in our study was higher, as the size of the population served by the PHCs in the studies differed, thus affecting the denominator. Studies have shown human resource cost as the major component of the overall cost of primary care centre costing (62-90%)15,17 in the present study also, human resource accounted for 56.9 per cent of ICT-enabled PHC per annum cost.
A systematic review looking for factors contributing to the failure or success of eHealth interventions found costs and national policies on eHealth investment to be important27. However, the same review also found that most of the studies were done during the implementation phase when costs were high and full results were yet not evident resulting in unproven cost-effectiveness27. However, in developed countries, it has been seen that although technological innovations have increased unit healthcare costs, it is expected that with increasing demand, market share and size, competition among vendors and availability of low cost technologies, the trend can get reversed28. Another study highlighted that if the start-ups are adequately funded and maintenance costs are covered, then, people can be more willing to use the new interventions8. At the government level, the decision for resource allocation is often guided by the cost of the intervention, feasibility of implementation, the implications on patient care and health outcomes; hence, the data on cost are an important input in decision-making.
This study had the limitation that the cost data were based on a single urban primary healthcare facility. Although the basic level of services and report generation remain similar in both urban and rural primary healthcare facilities, some modifications in the ICT system will have to be made for scaling at rural PHCs. The software being customizable at the local level, the same can be carried out by software developers with support from IT agencies through their maintenance contract. The simulations included the expected changes in infrastructure and human resources to arrive at the scaling up the cost to the state level. The present study estimated costs comprehensively using a well-established methodology24 for managing all functions of PHC using an open source and free ICT-based system. However, while implementing ICT at scale in PHC settings, several technological and behavioural challenges also need to be addressed besides the allocation of financial resources. Perceptions of all stakeholders (administrators, healthcare providers and users) and availability of mobile phones in the households also need to be taken into consideration while planning the scale-up of ICT interventions29.
In conclusion, customization of open-source software and implementation of IHIS4PHC led to an incremental cost of six per cent (₹ 0.47 million) per primary healthcare facility per annum if the eHealth intervention is scaled up to the state level. In view of the Government of India’s emphasis on ICT use in primary healthcare, cost estimates in the present study can be used for planning IHIS4PHC-like systems in primary healthcare facilities. However, adequate infrastructure and human resources as per Indian Public Health Standards are also needed.
Financial support and sponsorship
The study was funded by the Norwegian Research Council and the University of Oslo, Norway.
Conflicts of interest
None.
Acknowledgment:
Authors acknowledge the Health Information System Programme, India, for providing technical help to set up IT system and development of an integrated health information system for primary healthcare. Authors acknowledge Mr Pankaj Bahuguna, Statistician, for helping us in developing the costing design and analyzing the data.
References
- Transforming our world: The 2030 agenda for sustainable development |department of economic and social affairs. Available from :https://sdgs.un.org/2030agenda
- Primary health care as a foundation for strengthening health systems in low- and middle-income countries. J Gen Intern Med. 2017;32:566-71.
- [Google Scholar]
- 2002. The governmental public health infrastructure. In: The future of the public's health in the 21st century, Ch. 3. Washington (DC): National Academies Press (US); :125. Available from:https://www.nap.edu/ download/10548#
- 2005. Available from: https:///www.who.int/healthacademy/media/WHA58-28-en.pdf
- A holistic framework to improve the uptake and impact of eHealth technologies. J Med Internet Res. 2011;13:e111.
- [Google Scholar]
- Public health information systems for primary health care in India: A situational analysis study. J Family Med Prim Care. 2019;8:3640-6.
- [Google Scholar]
- Field testing of a digital health information system for primary health care: A quasi-experimental study from India. Int J Med Inform. 2020;141:104235.
- [Google Scholar]
- How to measure costs and benefits of eHealth interventions: An overview of methods and frameworks. J Med Internet Res. 2015;17:e254.
- [Google Scholar]
- Financial effects of health information technology: A systematic review. Am J Manag Care. 2013;19:SP369-76.
- [Google Scholar]
- The need for cost-benefit analyses of eHealth in low and middle-income countries. Stud Health Technol Inform. 2015;216:981.
- [Google Scholar]
- 2009. Washington, DC: United Nations Foundation and Vodafone Foundation; Available from:http://www.globalproblems-globalsolutionsfiles.org/unf_webs ite/assets/publications/technology/mhealth/mHealth_for_Dev elopment_full.pdf
- Estimating the unit costs of healthcare service delivery in India: Addressing information gaps for price setting and health technology assessment. Appl Health Econ Health Policy. 2020;18:699-711.
- [Google Scholar]
- Economic analysis of delivering primary health care services through community health workers in 3 North Indian states. PLoS One. 2014;9:e91781.
- [Google Scholar]
- Cost of delivering health care services in public sector primary and community health centres in North India. PLoS One. 2016;11:e0160986.
- [Google Scholar]
- Cost of health services provided at a primary health centre. Natl Med J India. 1995;8:156-61.
- [Google Scholar]
- Cost analysis of a primary health centre in northern India. Natl Med J India. 1993;6:160-3.
- [Google Scholar]
- Addressing the cost data gap for universal healthcare coverage in India: A call to action. Value Health Reg Issues. 2020;21:226-9.
- [Google Scholar]
- Cost analysis of implementing mHealth intervention for maternal, newborn &child health care through community health workers: Assessment of ReMIND program in Uttar Pradesh, India. BMC Pregnancy Childbirth. 2018;18:390.
- [Google Scholar]
- Evaluation of computerized health management information system for primary health care in rural India. BMC Health Serv Res. 2010;10:310.
- [Google Scholar]
- Open source, open standards, and health care information systems. J Med Internet Res. 2011;13:e24.
- [Google Scholar]
- A handbook of health system costing. New Delhi: Department of Health Research Ministry of Health and Family Welfare; 2021.
- Using top-down and bottom-up costing approaches in LMICs: The case for using both to assess the incremental costs of new technologies at scale. Health Econ. 2016;25((Suppl 1)):53-66.
- [Google Scholar]
- Establishing reference costs for the health benefit packages under universal health coverage in India: Cost of health services in India (CHSI) protocol. BMJ Open. 2020;10:e035170.
- [Google Scholar]
- The economics of eHealth. Available from: https://www.r4d.org/wp-content/uploads/Economics-of-eHealth.final_.3Nov1010_0.pdf
- Factors determining the success and failure of eHealth interventions: Systematic review of the literature. J Med Internet Res. 2018;20:e10235.
- [Google Scholar]
- Perception of stakeholders towards implementation of a patient centric digital health application for primary healthcare, India. Healthc Inform Res. 2021;27:315-24.
- [Google Scholar]






