Translate this page into:
Childhood cerebral adrenoleukodystrophy
*For correspondence: alizamittal@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
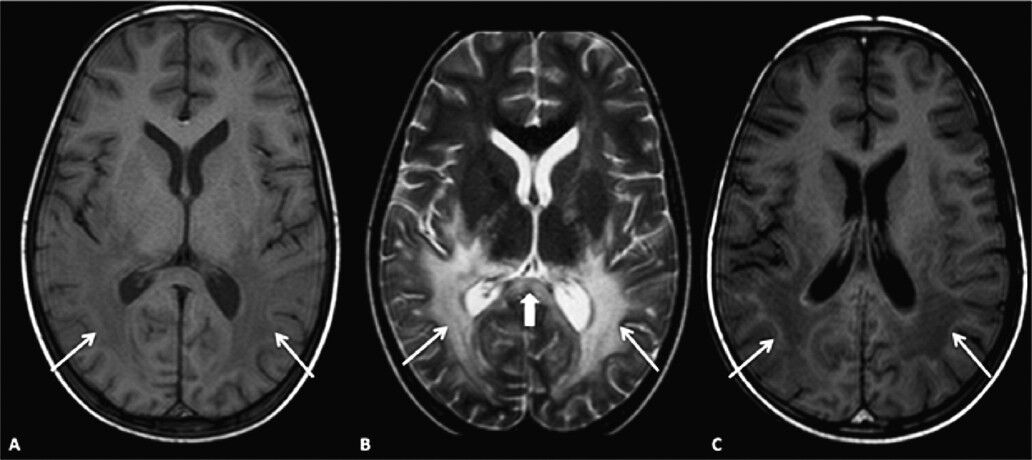
A 7- year old male child presented to the Department of Pediatrics at Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India in June 2013 with skin bronzing (hyperpigmentation) involving the skin, oral mucosa and pressure points (Fig. 1A, B, C). Born to a non consanguineous marriage he was also noted to have progressive neurological deterioration, difficulty in speech, worsening scholastic performance and upper motor neuron involvement of long tracts for the last seven months. Blood pressure was normal. On investigation, serum sodium was 138 meq/l and potassium was 4.1meq/l, random blood sugar was 90 mg/dl. Serum cortisol was 62 ng/ml (normal, 60-230 ng/ml) and serum adrenocorticotropic hormone (ACTH) levels were 45 pg/ml (normal 0-46 pg/ml). No waves were recordable on visual evoked potential suggestive of cortical blindness. Brainstem evoked response audiometry was normal. Tandem mass spectroscopy for aminoacid & acyl carnitine profile was normal. Magnetic resonance imaging (MRI) of brain was done which revealed abnormal T2 hyperintensities involving the splenium of corpus callosum and peritrigonal region which clinched the diagnosis of adrenoleukodystrophy (Fig. 2A, B). Post-contrast MR images showed enhancement of the intermediate zone (zone of active demyelination and inflammation) suggestive of progressive nature of the disease (Fig. 2C). CT abdomen showed normal adrenals. The child was given supportive treatment, along with dietary restriction in the form of low fat diet to reduce the VLCFA (very long chain fatty acid levels) and lovastatin was started as a lipid lowering agent. He did not show any significant improvement over six months follow up and has been planned for referral to higher centre for bone marrow transplantation.

-
(A). Clinical photograph of the child showing generalized hyperpigmentation compared to mother's hand (curved arrowhead) and hyperpigmented nail (arrowhead). (B) Picture showing mucosal hyperpigmentation (arrows). (C) Image showing hyperpigmented lateral malleolus-pressure point (arrow).
-
(A). Axial MR brain T1WI showing abnormal hypointense signal intensity involving peritrigonal region (arrows). (B) Axial MR brain T2WI showing abnormal hyperintense signal involving the peritrigonal region (arrows) and splenium of corpus callosum (thick arrow). (C) Axial MR brain T1 post- contrast image showing enhancement of the intermediate zone (arrows).





