Translate this page into:
Antimicrobial resistance pattern in Escherichia coli causing urinary tract infection among inpatients
Reprint requests: Dr Malini A., Associate Professor, Department of Microbiology, Indira Gandhi Medical College & Research Institute Vazhudavur Road, Kadirkammam, Puducherry 605 009, India e-mail: drmalinirb@yahoo.co.in
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Recent studies suggest an increasing antimicrobial resistance among Escherichia coli causing urinary tract infection (UTI). We undertook this study to know the resistance pattern of E. coli causing UTI in patients admitted to a tertiary care hospital in north India, and to know the treatment given and response of the patients.
Methods:
The details of E. coli grown from urine samples and their antibiotic sensitivity pattern were collected from the laboratory registers and the patient details were collected from the case records. The urine samples received were processed using standard methods and antibiotic susceptibility was done by Kirby-Bauer disk diffusion test.
Results:
Of the total 311 E. coli isolates, 119 (38.2%) were isolated from in-patients, which were considered for the study. Of these 119 E. coli isolates, 91 (76.51%) were multi drug resistant (MDR). The isolates showed high levels of resistance to ampicillin (88.4%), amoxicillin-clavulanic acid (74.4%), norfloxacin (74.2%), cefuroxime (72.2%), ceftriaxone (71.4%) and co-trimoxazole (64.2%). The isolates were sensitive to amikacin (82.6%), piperacillin-tazobactum (78.2%), nitrofurantoin (82.1%) and imipenem (98.9%). Ceftriaxone was most commonly used for empirical therapy for UTI among inpatients in our hospital. Of the 93 cases of UTI due to MDR E. coli, 73 improved on treatment and 12 worsened, which were referred to higher centres.
Interpretation & conclusions:
Our study showed that 76.5 per cent of E. coli isolates from urine samples of inpatients were MDR. Diabetes, chronic renal disease and catherization were some of the risk factors associated. The high rate of resistance could be because only inpatients were included and the increased usage of cephalosporins in our hospital for empirical therapy.
Keywords
Antimicrobial resistance
Escherichia coli
MDR
therapy
UTI
Urinary tract infection (UTI) can be caused by Gram-negative bacteria such as Escherichia coli, Klebsiella species, Enterobacter species, Proteus species and Gram-positive bacteria like Enterococcus species, and Staphylococcus saprophyticus. E. coli is the most common organism causing both community as well as hospital acquired UTI1. Studies from various parts of India have shown occurrence of high rates of antimicrobial resistance among E coli. The resistance rates of uropathogenic E. coli to various antibiotics have been reported as beta-lactams (57.4%), co-trimoxazole (48.5%), quinolones (74.5%), gentamicin (58.2%), amikacin (33.4%), cefuroxime (56%), nalidixic acid (77.7%)12345. UTI due to multi drug resistant (MDR) E. coli increases the cost of treatment, morbidity and mortality especially in developing countries like India67. This study was undertaken to know the resistance pattern of E. coli causing UTI in patients admitted to a hospital in Puducherry, south India. Further analysis was done to identify the associated risk factors and data were also collected regarding the treatment given.
Material & Methods
This hospital record based cross-sectional study was conducted in a 750 bedded tertiary care centre located in Puducherry, south India. The analysis was done on all E. coli isolates obtained from urine samples among hospital inpatients, admitted during the period of August 2011 to July 2012. All the inpatients with UTI at the time of admission or acquired during their stay in the hospital were included in the study. Ethical clearance for the study was obtained from the institutional ethics committee.
Urine culture was done by standard loop method, a semi-quantitative method. The organisms isolated from urine culture were identified by standard methods1. The antibiotic sensitivity test was done on Mueller-Hinton agar by Kirby-Bauer disc diffusion test as per Clinical and Laboratory Standard Institute (CLSI) guidelines8. The isolates were tested for ampicillin (10 μg), cefuroxime (30 μg), ceftriaxone (30 μg), norfloxacin (10 μg), nitrofurantoin (300 μg), amoxicillin-clavulanic acid (10/20 μg), co-trimoxazole (1.25/23.75 μg), cefepime (30 μg), ciprofloxacin (5 μg), amikacin (30 μg), piperacillin-tazobactam (100/10 μg) and imipenem (10 μg) (Hi-media, Mumbai). An isolate was considered as MDR if found resistant to three or more antimicrobials belonging to different classes/groups of antimicrobials.
The data regarding the urine culture and sensitivity pattern were obtained from the Microbiology laboratory registers. The patients’ details were collected from case sheets in the Medical Records Department and wards.
Proportions were used to study the resistance pattern of E. coli and to study the association of risk factors in UTI due to MDR E. coli.
Results & Discussion
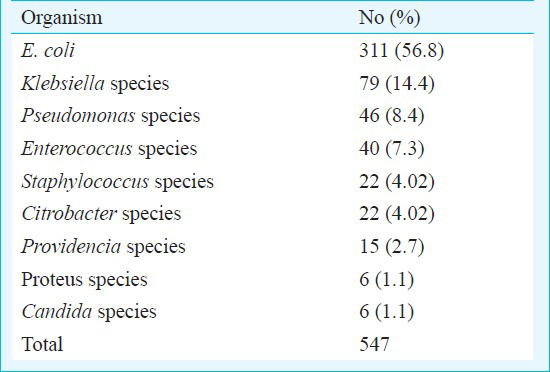
A total of 2941 urine samples were received for culture and sensitivity during the study period. Among these, 547 samples (18.5%) yielded significant bacteriuria; 2323 samples (79.1%) showed no growth and 74 samples (2.4%) showed mixed growth.
The various organisms isolated from urine culture are shown in Table I. E. coli was the commonest accounting for 56.8 per cent of the uropathogens. Of the 311 E. coli isolates, 119 (38.2%) were isolated from 119 inpatients (age range on 6 months-80 yr) and hence were included in the analysis.
The isolates were sensitive to amikacin (82.6%), piperacillin-tazobactum (78.2%), nitrofurantoin (82.1%) and imipenem (98.9%); 91 of 119 (76.5%) E. coli isolates were multi drug resistant. The sensitivity to ampicillin, cefuroxime, ceftriaxone, norfloxacin, ciprofloxacin varied from 11-25 per cent.
During the analysis it was observed that empirical therapy was started in 80 cases. In 42 cases ceftriaxone was used, in 20 ciprofloxacin, in seven cases norfloxacin and in the remaining few ampicillin, amoxicillin, cephalexin and doxycycline were used.
Of the 91 patients with UTI due to MDR E. coli, 73 (80.2%) patients improved after the treatment, whereas 12 (13.2%) worsened with the treatment and hence were referred to higher centres. Four patients were discharged at request and two left the hospital against medical advice. No deaths were observed in the study.
The most common risk factor associated with MDR E. coli were diabetes mellitus (19 patients, 28.7%) followed by renal pathologies (14 patients, 21.2%) like nephrotic syndrome, chronic renal disease, hydroureteronephrosis (HUN), and posterior urethral valve. The other risk factors were catheterisation (9, 13.6%), renal calculi (6, 9.1%); 39 of 91 patients did not have any risk factors.
Formation of biofilms inside the bladder causes recurrent infections and also increases the chance of MDR strain causing UTI910. Studies from India have reported. E. coli as one of the commonest organisms causing UTI234. In our study also E. coli was the commonest organism followed by Klebsiella species.
In our study, 76.5 per cent isolates of E. coli were MDR. This is quite high when compared to other studies. Prevalence of MDR E. coli was about 52.9 per cent in a study done by Hasan et al2 in a tertiary care Indian hospital and 7.1 per cent in a study done by Sahm et al11 in the USA. A study by Mathai et al5 in southern India has showed that 8.4 per cent of commensal E. coli were MDR5.
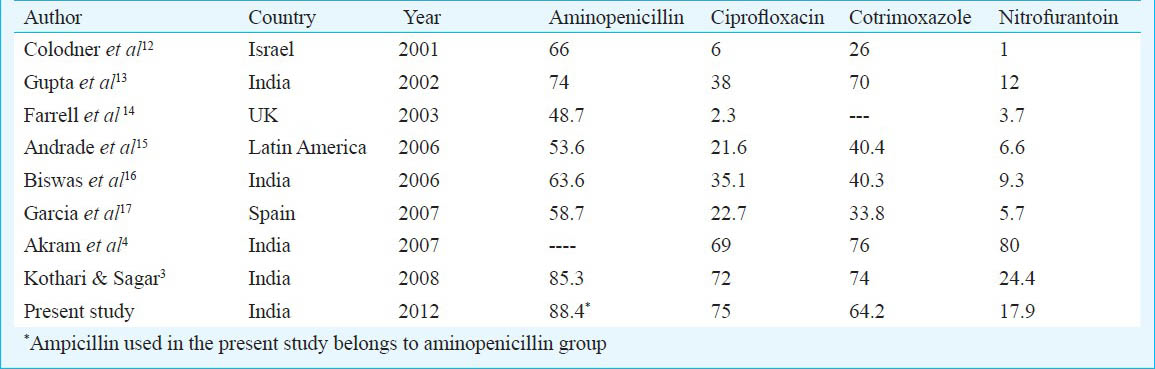
The antimicrobial sensitivity pattern of the E. coli isolates in our study was similar to previous studies done in India. The comparison of resistance patterns of uropathogenic E. coli in various studies is shown in Table II34121314151617.
In 21 cases though the clinical picture was not UTI, the culture grew MDR E. coli. This could be due to improper collection of the mid-stream urine sample or there could have been a delay in transporting the sample to the laboratory which might have given a false positive culture report. The limitations of the study were that it included only the inpatients, as a result of which the resistance rates could be high. The study did not test for ESBLs and genotyping of the resistance genes was not done.
To conclude, this study showed high resistance among uropathogenic E. coli to ampicillin, cephalosporins, and fluoroquinolones. The increased occurrence of UTI due to MDR E. coli could be due to increased prevalence of MDR strains in the community.
Acknowledgment
The authors acknowledge the Indian Council of Medical Research (ICMR), New Delhi, India for providing Short term research studentship (STS) to the first author (NV) (STS Ref ID : 2012-02494).
References
- Urinary tract infections. In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas and Bennett's principles and practice of infectious diseases Vol 1. (7th ed). Philadelphia, USA: Churchill Livingstone Elsevier publication; 2010. p. :958-72.
- [Google Scholar]
- Resistance patterns of urinary isolates in a tertiary Indian hospital. J Ayub Med Coll Abbottabad. 2007;19:39-41.
- [Google Scholar]
- Antibiotic resistance in pathogens causing community-acquired urinary tract infections in India: a multicenter study. J Infect Dev Ctries. 2008;2:354-8.
- [Google Scholar]
- Etiology and antibiotic resistance patterns of community acquired urinary tract infections in JNMC hospital Aligrah, India. Ann Clin Microbiol Antimicrob. 2007;6:4.
- [Google Scholar]
- Antimicrobial resistance surveillance among commensal Escherichia coli in rural and urban areas in Southern India. Trop Med Int Health. 2008;13:41-5.
- [Google Scholar]
- Al-Sharif. UTI with E. coli and antibacterial activity of some plant extract. Int J Microbiol Res. 2011;2:1-7.
- [Google Scholar]
- Bailey & Love's short practice of surgery. (25th ed). London: United Kingdom: Edward Arnold Publishers; 2008. p. :1329-30.
- [Google Scholar]
- Performance standards for antimicrobial susceptibility testing, 20th information supplement M100-S20. Wayne, PA, USA: CLSI; 2010.
- [Google Scholar]
- Urinary tract infections, pyelonephritis, prostatitis. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, eds. Harrison's principles of internal medicine Vol 2. (17th ed). New York USA: Mc-Graw Hill; 2008. p. :1820-5.
- [Google Scholar]
- Urinary tract infections. In: Kliegman RM, Behrman RE, Jenson HB, Stanton BE, eds. Nelson Textbook of pediatrics Vol 2. (18th ed). Philadelphia USA: Saunders Elsevier; 2007. p. :2224-5.
- [Google Scholar]
- Multidrug-resistant urinary tract isolates of Escherichia coli: Prevalence and patient demographics in the United States in 2000. Antimicrob Agents Chemother. 2001;45:1402-6.
- [Google Scholar]
- Antimicrobial susceptibility of community-acquired uropathogens in northern Israel. Int J Antimicrob Agents. 2001;18:189-92.
- [Google Scholar]
- Antibiotic resistance pattern in uropathogens. Indian J Med Microbiol. 2002;20:96-8.
- [Google Scholar]
- A UK multicentre study of the antimicrobial susceptibility of bacterial pathogens causing urinary tract infection. J Infect. 2003;46:94-100.
- [Google Scholar]
- Increased resistance to first-line agents among bacterial pathogens isolated from urinary tract infections in Latin America: time for local guidelines? Mem Inst Oswaldo Cruz. 2006;101:741-8.
- [Google Scholar]
- Choice of antibiotic for empirical therapy of acute cystitis in a setting of high antimicrobial resistance. Indian J Med Sci. 2006;60:53-8.
- [Google Scholar]
- Spanish Cooperative Group for the Study of Antimicrobial susceptibility of Community Uropathogens. In vitro susceptibility of community-acquired urinary tract pathogens to commonly used antimicrobial agents in Spain: a comparative multicenter study (2002-2004) J Chemother. 2007;19:263-70.
- [Google Scholar]






