Translate this page into:
Aetiological spectrum of severe community-acquired pneumonia in HIV-positive patients from Pune, India
*For correspondence: amane@nariindia.org
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Pulmonary infections are a major cause of morbidity and mortality in HIV-positive individuals, of which bacterial community-acquired pneumonia (BCAP) is reported to be 25 times more common than in the general community123. Studies also indicate increased BCAP-related mortality rates in HIV-positive patients24. Selection of initial empirical treatment depends on the common pathogens identified in previous aetiological studies and relevant treatment trials; however, the aetiological profile of CAP is different in different countries, and hence it is imperative that these recommendations are based on epidemiological data obtained from particular geographic location. Severe CAP (SCAP) occurs in approximately 18-36 per cent of all CAP cases with mortality rate of <5 per cent in outpatient cases, 10 per cent in hospitalized patients and can exceed 30 per cent in patients admitted to Intensive Care Units5. There is a paucity of data on the aetiological profile of SCAP from the South Asian countries, especially amongst HIV-positive patients. The present study was thus conducted to determine the aetiological spectrum of severe CAP and to assess the mortality predictors associated with BCAP in HIV-positive patients from Pune, India.
This prospective observational study was conducted in collaboration with the department of Chest and Tuberculosis, Sassoon General Hospitals, Pune, India, attached to B. J. Government College, during January 2012-2014. A total of 121 consecutive HIV-positive patients presented with SCAP during the study period, of whom 111 were enrolled. Seven patients were critically ill, whereas three refused to consent and hence were not included. The inclusion criteria for SCAP were patients presenting with symptoms of CAP6 and associated with either two or more of the criteria listed in parenthesis (systolic BP ≤90 mmHg, bilateral pneumonia or multilobar pneumonia and PaO2/FIO2≤250 mmHg) or with the presence of septic shock (hypotension not responding to adequate fluid resuscitation and required vasopressor/ionotropic support). Patients <18 yr of age, reporting hospitalization within seven days, critically ill and those refusing to consent were excluded from the study. The study was approved by the Institutional Ethics Committees of the B. J. Government College and ICMR-National AIDS Research Institute (NARI), Pune. Written informed consent was obtained from all participants.
All patients underwent complete history taking in structured questionnaires and physical examination by the attending physician. Chest radiography was done followed by the collection of induced sputum or bronchoalveolar lavage (BAL) and blood samples for microbiological workup, before instituting empirical therapy. The samples were sent to the Microbiology Laboratory, NARI, maintaining the cold chain for laboratory testing. The quality of the samples of induced sputum and BAL samples was assessed78. Bacterial identification, reporting of significant cultures and antibiotic sensitivity testing were performed using standard microbiological techniques91011. The criteria for labelling an organism as multidrug-resistant (MDR) were as per Magiorakos et al12. Atypical bacteria were detected by polymerase chain reaction (PCR) using primers that amplified 630bp fragment of mip gene for Legionella pneumophila, 277 bp fragment of 16S rRNA gene for Mycoplasma pneumoniae and 438 bp fragment of PstI fragment for Chlamydophila pneumoniae13.
Mycobacterial detection was done by Ziehl-Neelsen acid-fast staining and Lowenstein Jensen culture. Pneumocystis jiroveci, Cytomegalovirus and Herpes simplex virus were detected by PCR using primers targeting the mitochondrial large-subunit rRNA gene, IRL 11 region and simplex herpes virus (HSV) glycoprotein B gene, respectively1415. The aetiological cause to each case was assigned as per the criteria of Park et al16. Mortality was defined as death due to BACP during hospital stay.
Statistical analysis: Statistical analysis was done using SPSS statistical software version 15.0 (SPSS, Chicago, USA). Frequencies of aetiological agents were reported according to their monomicrobial or polymicrobial status. Mortality-associated factors with BCAP were analyzed by logistic regression. All variables found to be significant in univariate analysis were included in multivariate analysis.
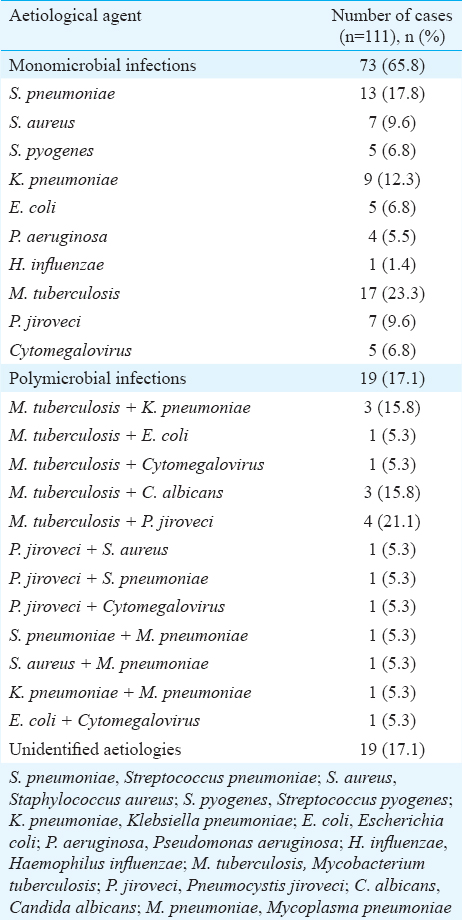
Of the 111 cases, 92 (82.9%) had identifiable aetiologies, of which 73 (79.3%) were monomicrobial and 19 (20.7%) were polymicrobial infections. The aetiological distribution is presented in Table I. To restrict the analysis to BCAP, patients with diagnosis of mycobacterial, fungal and viral aetiologies were excluded from further analysis.
Amongst the cases with identifiable aetiologies, 47 (51.1%) were definitive BCAP cases. BCAP patients were predominantly males (63.8%, n=30), with median age 39 [interquartile range (IQR) 35, 44] yr, 55.3 per cent (n=26) were on antiretroviral therapy (ART) and 21.3 per cent (n=10) were receiving co-trimoxazole prophylaxis. The median CD4+ count was 338 (IQR 238, 441) cells/μl in patients on ART and 92 (IQR 65, 122) cells/μl in ART-naive ones. Co-morbid conditions [chronic obstructive pulmonary disease (n=2), chronic liver disease (n=4), asthma (n=1) and diabetes mellitus (n=2)] were present in 19.1 per cent (n=9) patients. There were no significant differences in the overall characteristics of patients with and without BCAP. The presenting symptoms were cough (95.7%, n=45), fever (80.8%, n=38), breathlessness (42.5%, n=20) and chest pain (17.02%, n=8). Radiological involvement revealed monolobar involvement in 35 (74.5%) cases, whereas 12 (25.5%) had multilobar involvement of whom four had pleural effusion.
Streptococcus pneumoniae was the predominant pathogen isolated (14 of 47, 29.8%). A total of 35.8 (n=5), 28.6 (n=4) and 7.2 (n=1) per cent isolates were resistant to penicillin, erythromycin and co-trimoxazole, respectively, while all were sensitive to tetracycline, cefotaxime and ciprofloxacin. MDR was seen in 7.1 per cent (n=1) isolates. Gram-negative bacilli (GNB) including Klebsiella pneumoniae (n=9), Escherichia coli (n=5) and Pseudomonas aeruginosa (n=4) were detected in 40.4 per cent (n=19) cases. A total of 68.4 (n=13), 52.7 (n=10), 47.4 (n=9), 26.4 (n=5), 21.1 (n=4) and 15.8 (n=3) per cent isolates were resistant to co-trimoxazole, amoxicillin-clavulanic acid, tetracycline, cefotaxime, ciprofloxacin and gentamicin, respectively, whereas all were sensitive to imipenem. Extended spectrum beta-lactamase production was seen in 5 of 15 (33.3%) isolates. MDR was seen in 31.6 per cent (n=6) isolates. S. aureus was isolated in 8 of 47 (17.02%) cases. Methicillin resistance was observed in 37.5 per cent (n=3) isolates, whereas 50 per cent isolates (n=4) were resistant to erythromycin and co-trimoxazole, 37.5 per cent (n=3) to amoxicillin-clavulanic acid and tetracycline, 25 per cent (n=2) to ciprofloxacin and 12.5 per cent (n=1) to gentamicin, whereas all were sensitive to vancomycin. MDR was seen in 12.5 per cent (n=1) isolates. Beta-haemolytic streptococci and Haemophilus influenzae were seen in 10.6 (n=5) and 2.1 per cent (n=1) cases, respectively. A total of 40 per cent (n=2) streptococcal isolates were resistant to co-trimoxazole and amoxicillin-clavulanic acid and 20 per cent (n=1) to erythromycin and tetracycline, while all were sensitive to cefotaxime, ciprofloxacin and vancomycin. The single H. influenzae isolate was sensitive to amoxicillin-clavulanic acid, erythromycin, tetracycline, cefotaxime and ciprofloxacin.
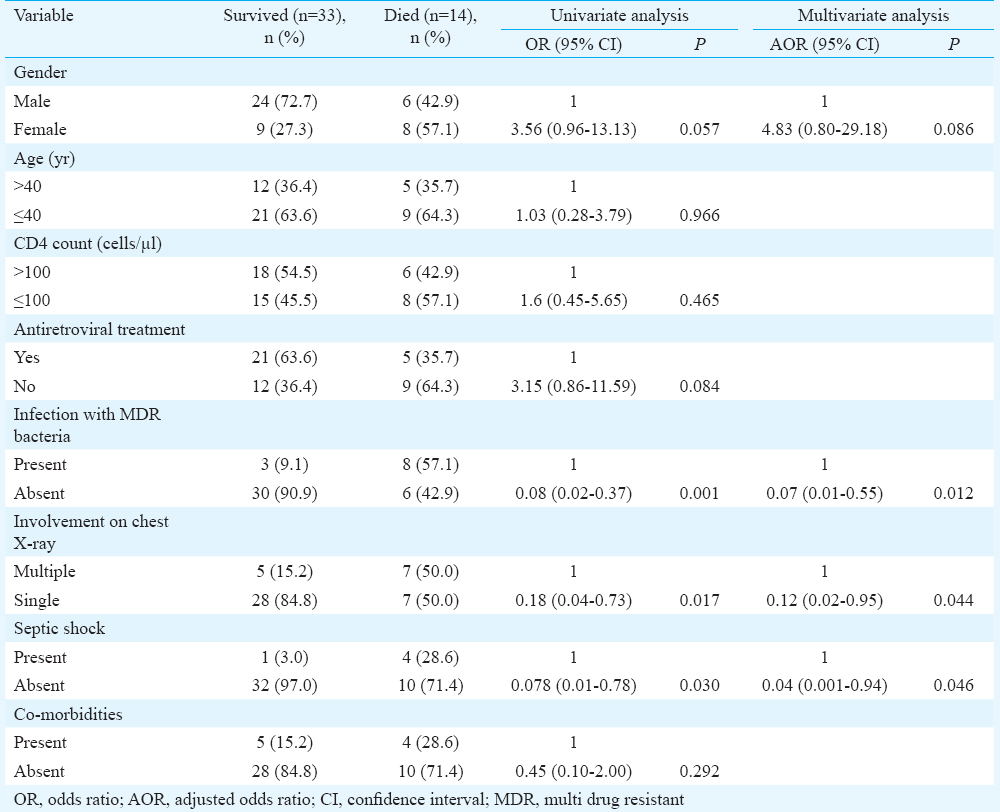
Overall MDR was observed in 23.4 per cent (n=26) isolates, whereas bacteraemia was seen in 7.2 per cent (n=8) cases. Atypical bacteria, all M. pneumoniae, were detected in 6.4 per cent (n=3) cases. Mortality during hospital stay in BCAP cases was 29.8 per cent (14/47). The bacterial isolates in the 14 fatal cases were S. aureus (n=5), K. pneumoniae (n=4), P. aeruginosa (n=2) and S. pneumoniae (n=3). Fatality was seen in 62.5 per cent S. aureus, 50 per cent P. aeruginosa, 40 per cent K. pneumoniae and 21.4 per cent S. pneumoniae infections. Table II shows the risk factors associated with BCAP mortality. On multivariate analysis, infection with MDR bacteria [P=0.012, adjusted odds ratio (AOR)=0.07, 95% confidence interval (CI)=0.01-0.55], multilobar involvement (P=0.044, AOR=0.12, 95% CI=0.02-0.95) and septic shock (P=0.046, AOR=0.04, 95% CI=0.001-0.947) were independently associated with mortality.
In the present study, aetiological diagnosis was possible in 82.9 per cent (n=92) cases. Worldwide, variable rates of aetiological diagnosis in CAP have been reported and these differences can be attributed to factors such as geographical locales, patient groups studied, samples used, aetiologies assessed and diagnostic assays employed. The ability to investigate an array of pathogens and collection of induced sputum or BAL allowed us to better define the aetiologies in our patients.
Overall 51.1 per cent CAP cases (n=47) were attributable to bacterial aetiologies. Worldwide, prevalence rates of BCAP ranging from 10.7 to 52.7 per cent have been reported from HIV-positive individuals1718192021. In confirmation with previous reports, S. pneumoniae was the most common bacterial isolate and exhibited considerable resistance to routinely prescribed antibiotics1720212223242526. Bacteraemia and high recurrence rates complicating pneumococcal pneumonia amongst HIV-positive individuals have been reported27, warranting an urgent need for evaluation of pneumococcal vaccine for its potential benefits in Indian HIV-positive patients. Although reported to account for approximately five per cent pneumonias in HIV-positive persons, GNB were detected in a considerable number of cases. GNB constitute the common pathogens reported in HIV-negative CAP cases in Indian settings222324. The high mortality observed with S. aureus infection was in corroboration with earlier studies1728. Our results were in contrast with the only study from India that reported a high prevalence of M. pneumonia infection amongst HIV-positive individuals22.
Mortality during hospital stay was 29.8 per cent. Studies worldwide have reported mortality rates ranging from 5 to 30 per cent in HIV-positive patients with BCAP12345. The association between septic shock and radiological progression has been reported previously32129; however, there are limited data on the impact of drug-resistant bacteria on clinical outcome of BCAP. We found a significant association between initial infection with MDR organism and mortality in HIV-positive patients. High in vitro resistance was observed towards commonly prescribed antibiotics with about one-fourth MDR isolates, highlighting the need to institute appropriate initial antimicrobials directed towards the pathogen, which may lead to favourable clinical outcome and prevent the chronology to death.
This study was a single centre study; hence the results may not be generalizable to the entire country. However, all patients were enrolled prospectively and consecutively, lending consistency to data in contrast to the retrospective reports published earlier329. To conclude, this study identified the predominance of bacterial aetiologies and high in vitro resistance to commonly prescribed antibiotics in SCAP amongst HIV-positive patients, highlighting the need for choosing appropriate initial pathogen-directed antimicrobial therapy for proper management of BCAP.
Acknowledgment
The authors would like to thank all the participants enrolled and the staff at Sassoon General Hospitals for their support rendered in this study.
Financial support & sponsorship: The study was financially supported by the Indian Council of Medical Research, New Delhi (intramural grant)
Conflicts of Interest: None.
References
- Pulmonary infections in HIV-infected patients: An update in the 21st century. Eur Respir J. 2012;39:730-45.
- [Google Scholar]
- A clinical predictor score for 30-day mortality among HIV-infected adults hospitalized with pneumonia in Uganda. PLoS One. 2015;10:e0126591.
- [Google Scholar]
- Clinical outcomes of HIV-infected patients hospitalized with bacterial community-acquired pneumonia. Int J Infect Dis. 2010;14:e22-7.
- [Google Scholar]
- Community-acquired lung respiratory infections in HIV-infected patients: Microbial aetiology and outcome. Eur Respir J. 2014;43:1698-708.
- [Google Scholar]
- Etiology and outcome of severe community acquired pneumonia in immunocompetent adults. BMC Infect Dis. 2013;13:94.
- [Google Scholar]
- Guidelines for diagnosis and management of community- and hospital-acquired pneumonia in adults: Joint ICS/NCCP(I) recommendations. Lung India. 2012;29:S27-62.
- [Google Scholar]
- Usefulness of sputum culture for diagnosis of bacterial pneumonia in HIV-infected patients. Eur J Clin Microbiol Infect Dis. 2002;21:362-7.
- [Google Scholar]
- Immunocompromised host. In: Baughman RP, ed. Bronchoalveolar lavage. St Louis: Mosby Year Book Inc; 1992. p. :41-63.
- [Google Scholar]
- Color atlas and textbook of diagnostic microbiology. Philadelphia: Lippincott Williams & Wilkins; 2006.
- [Google Scholar]
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing; Twenty First Informational Supplement. M100-S21. Wayne, PA: CLSI; 2011.
- [Google Scholar]
- The clinical microbiology laboratory in the diagnosis of lower respiratory tract infections. J Clin Microbiol. 2011;49:S30-3.
- [Google Scholar]
- Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268-81.
- [Google Scholar]
- Rapid detection of bacterial atypical pneumonia agents by multiplex PCR. Cent Eur J Public Health. 2004;12:3-5.
- [Google Scholar]
- Amplification of mitochondrial ribosomal RNA sequences from Pneumocystis carinii DNA of rat and human origin. Mol Biochem Parasitol. 1990;43:69-76.
- [Google Scholar]
- Laboratory diagnosis of common herpesvirus infections of the central nervous system by a multiplex PCR assay. J Clin Microbiol. 2001;39:4426-32.
- [Google Scholar]
- The etiology of community-acquired pneumonia at an urban public hospital: Influence of human immunodeficiency virus infection and initial severity of illness. J Infect Dis. 2001;184:268-77.
- [Google Scholar]
- Prospective study of etiologic agents of community-acquired pneumonia in patients with HIV infection. AIDS. 2002;16:85-95.
- [Google Scholar]
- Acute community-acquired bacterial pneumonia in human immunodeficiency virus (HIV) infected and non-HIV-infected adult patients in cameroon: Aetiology and outcome. Tuber Lung Dis. 1996;77:47-51.
- [Google Scholar]
- Bacterial community acquired pneumonia in HIV-infected inpatients in the highly active antiretroviral therapy era. Infection. 2008;36:231-6.
- [Google Scholar]
- Community-acquired bacterial pneumonia in human immunodeficiency virus-infected patients: Validation of severity criteria. The Grupo Andaluz para el Estudio de las Enfermedades Infecciosas. Am J Respir Crit Care Med. 2000;162:2063-8.
- [Google Scholar]
- Epidemiological studies on pulmonary pathogens in HIV-positive and -negative subjects with or without community-acquired pneumonia with special emphasis on Mycoplasma pneumoniae. Jpn J Infect Dis. 2007;60:337-41.
- [Google Scholar]
- Clinical and bacteriological profile of community acquired pneumonia in Shimla, Himachal Pradesh. Indian J Chest Dis Allied Sci. 2004;46:17-22.
- [Google Scholar]
- Etiology and anti-microbial sensitivity of organisms causing community acquired pneumonia: A single hospital study. J Family Med Prim Care. 2013;2:244-9.
- [Google Scholar]
- Declining antimicrobial susceptibility of Streptococcus pneumoniae in the United States: Report from the SENTRY antimicrobial surveillance program (1998-2009) Diagn Microbiol Infect Dis. 2010;68:334-6.
- [Google Scholar]
- Pneumococcal pneumonia in HIV-infected patients by antiretroviral therapy periods. HIV Med. 2008;9:203-7.
- [Google Scholar]
- Pneumonia caused by methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2004;46:S378-85.
- [Google Scholar]
- Influence of HIV infection on the clinical presentation and outcome of adults with acute community-acquired pneumonia in Yaounde, Cameroon: A retrospective hospital-based study. BMC Pulm Med. 2012;12:46.
- [Google Scholar]





