Translate this page into:
A study on the effect of mobile phone use on sleep
For correspondence: Dr Sanjeev Sinha, Department of Medicine, All India Institute of Medical Sciences, New Delhi 110 029, India e-mail: drsanjeevsinha@gmail.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Several studies have been conducted globally to assess the impact of usage of mobile phones on quality and duration of sleep as also on day time sleepiness. The objective of the present study was to assess the effect of mobile phone usage on the quality and composition of sleep in a sample from Indian population.
Methods:
The study was conducted at two tertiary care hospitals in north India from July 2014 to September 2019. A total of 566 participants were recruited in this study from both the centres. Sleep quality was assessed with the help of the Pittsburgh Sleep Quality Index (PSQI) questionnaire. Subsequently, actigraphy was done in 96 participants and polysomnography in 95 participants.
Results:
Of the 566 participants, 128 (22.61%) had PSQI ≥5, reflecting poor sleep quality. A higher use of mobile phone was significantly associated with a poor sleep quality as a component of PSQI questionnaire (P=0.01) and higher overall PSQI score (P=0.01). The latency from sleep onset to N2 and N3 sleep stages was significantly shorter in participants having a higher mobile phone usage as compared to those with a lower usage [Median (range): 13.5 min (1.5-109) vs. 6.5 min (0-89); P=0.02] and [Median (range): 49 min (8.5-220.5) vs. 28.75 min (0-141); P=0.03], respectively.
Interpretation & conclusions:
This study focused on the maladaptive changes brought on by mobile phone usage on sleep. More studies with larger sample sizes need to be done that may serve to confirm the hypothesis generating findings of our study.
Keywords
Actigraphy
mobile phone
Pittsburgh Sleep Quality Index
polysomnography
sleep
The usage of mobile phones in India has increased exponentially. Concerns about exposure to radiation both from phones and telecommunication infrastructure have led to an upsurge of studies examining the potential ill effects1234. The plausible effect of excessive mobile phone usage on sleep pattern and quality is also important due to it societal implications56. Concerns about the thermal effect of microwaves used in mobile phones are felt to be negligible at the power used by usual mobile phones7. Large epidemiological studies have not found a consistent effect of mobile phone usage on overall mortality except when used in hazardous circumstances like during driving89.
To assess the effect of radiation exposure on well-being and sleep, Hutter et al10 performed a cross-sectional study in urban and rural populations living near mobile phone towers in Austria and concluded that symptoms such as headache were common in these populations. However, their study failed to show any significant changes in sleep quality. Subsequent studies showed that exposure to electromagnetic waves and excessive use of mobile phones resulted in disrupted sleep1112. A cross-sectional study conducted by Demir and Sumer6 in migraine patients in Turkey, demonstrated that mobile phone usage was significantly associated with higher rates of headache, excessive daytime sleepiness and poor sleep quality. A similar study to assess the impact of mobile phone usage on sleep in Japanese adolescents found that an increase in use after lights out before sleep was associated with a shorter sleep duration, poorer quality of sleep, insomnia as well as excessive daytime sleepiness13. Similar data are sparse in the Indian population with its distinct genetic and sociocultural characteristics. This study was therefore, conducted to assess the effect of mobile phone usage on the quality and composition of sleep in a representative sample of the Indian population.
Material & Methods
This cross-sectional study was conducted from July 2014 to September 2019 at the All India Institute of Medical Sciences (AIIMS), New Delhi, and Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh. A total of 566 participants were recruited with the aim to see the effect between the frequency of mobile phone use for calls and short message service (SMS) as well as total duration of mobile phone usage on quality of sleep. Participants were enrolled from the outpatient departments, undergraduate hostels and post-graduate hostels at the AIIMS and PGIMER. All adults in the age group 20 to 60 yr who had used mobile phones for more than one year, were eligible for participation in the study. Those who were suffering from any neurologic or psychiatric illness, critically ill patients, chronic alcoholics and smokers, who had any visual or auditory impairment as well as those with a prior diagnosis of metabolic syndrome were excluded. The study was approved by the Institute Ethics Committee of AIIMS and PGIMER and written informed consent was obtained from each participant.
Measures:
Demographic data: Age, gender and educational qualifications of all participants were recorded. A basic medical history was taken. Mobile phone use was quantified in terms of total number of calls and SMSs received per day for the past 30 days. If the total number of calls and SMSs per day was ³12 or either of these individually exceeded 11, the participant was considered to be a high user11.
Subjective sleep quality: The subjective sleep quality was assessed with the help of the Pittsburgh Sleep Quality Index (PSQI) questionnaire14. PSQI is a self-rated questionnaire that assesses sleep quality over the preceding one month. It has 19 individual items that generate seven component scores in the following domains-subjective sleep quality, sleep latency (SL), sleep duration, habitual sleep efficiency, sleep disturbances, need to use medications for sleep and daytime dysfunction. A PSQI global score of ≥5 yielded a diagnostic sensitivity of 89.6 per cent and specificity of 86.5 per cent in distinguishing good and poor sleepers14.
Actigraphy: Actigraphy sleep data were collected using the SOMNO watch (Actiwatch Spectrum Plus; Philips Respironics Inc., Murrysville, PA, USA). The monitor provided the estimates of SL, wake after sleep onset (WASO) and the sleep efficiency. SL is defined as the length of time taken to fall asleep - the time between ‘lights off’ to the first period of three minutes of consecutive epochs scored as sleep. WASO refers to the number of minutes awake between sleep onset and time of final waking. Sleep efficiency is defined as the proportion of the estimated sleep periods spent asleep. The data were collected for a period of three days for each participant. The average SL, sleep efficiency and WASO were calculated for period of three days.
Polysomnography (PSG): Polysomnography studies were conducted in the sleep laboratory using Alice 3 or ALICE PDx systems (Philips Respironics, Murrysville, PA, USA). A continuous polygraphic recording was done from surface electrodes for electroencephalogram, electromyogram, electrooculogram, electrocardiogram, thermistors for oral and nasal flow, thoracic and abdominal impedance belts for respiratory efforts, pulse oximetry, tracheal microphone for snoring and sensors for leg and sleep position. PSG records and sleep data were scored as per American Academy of Sleep Medicine (AASM) criteria15. The following sleep parameters were recorded: total sleep time (TST), SL, stage R latency (RL), WASO, time spent in stages N1, N2, N3 and R in per cent of TST and latency from sleep onset to stage N2 and N3.
Statistical analysis: Analysis was done with Stata11.2 (StatCrop LP, College Station; TX, USA). Quantitative variables were presented as mean with standard deviation, median with range and frequency percentage as appropriate. Categorical variables were compared using Chi-square and Fisher’s exact test. Continuous variables were compared by Kruskal-Wallis test.
Results
A total of 566 participants were enrolled with recording of demographic variables and administration of PSQI questionnaire. The mean age of the participants was 31.03 ± 9.82 yr. The proportion of male participants was 57.60 per cent. 42.4 per cent of the participants had an undergraduate degree. Based on the number of mobile phone calls and messages received each day, 39 per cent of the participants interviewed had a high daily mobile phone usage (Table I).
| Parameters | Low usage (n=345) | High usage (n=221) |
|---|---|---|
| Age (yr), mean (SD)* | 32.33 (10.88) | 29 (7.45) |
| Gender, n (%)## | ||
| Male | 164 (50.31) | 162 (49.69) |
| Female | 181 (75.42) | 59 (24.58) |
| Educational qualification, n (%)*** | ||
| Below 12th standard | 139 (75.54) | 45 (24.46) |
| Undergraduate | 130 (57.52) | 96 (42.48) |
| Post-graduate | 76 (48.72) | 80 (51.28) |
P *<0.01, ***<0.001 (Mann-Whitney U test); ##<0.001 (Chi square test). SD, standard deviation; SMS, short message service
Overall, 128 of 566 participants (22.61%) had a subjectively poor sleep with a PSQI ≥ 5. A higher mobile phone usage was seen to be significantly associated with a poor sleep quality as a component of the PSQI questionnaire (P=0.01) and a higher overall PSQI score (P=0.01) (Figure). A subjectively longer SL period, a shorter total sleep duration, poorer sleep efficiency and evident daytime dysfunction were observed to be associated with excessive cell phone use although these trends did not attain significance (Table II).
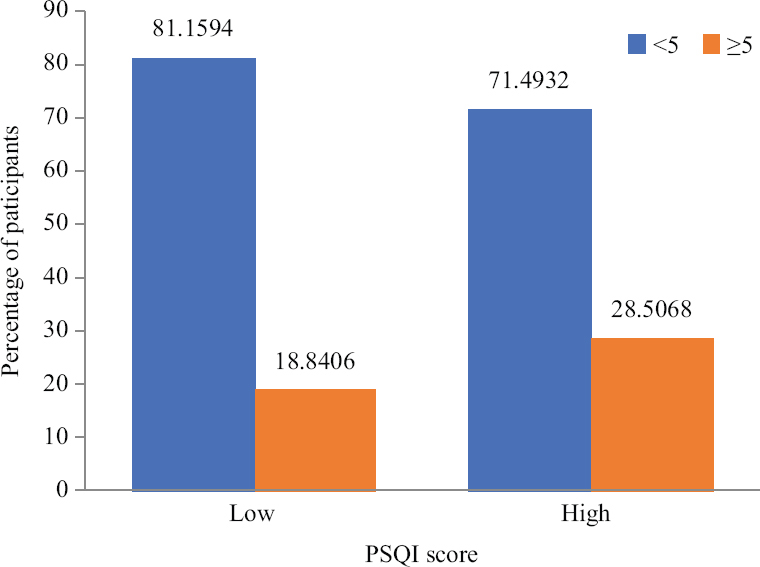
- Histogram showing the association between mobile phone use in terms frequency of calls and short message services (low vs. high) and the Pittsburgh Sleep Quality Index score low vs. high
| Component | Response | Low usage (n=345), n (%) | High usage (n=221), n (%) | P |
|---|---|---|---|---|
| Sleep quality | Very good (n=227) | 156 (68.72) | 71 (31.28) | 0.001 |
| Fairly good (n=307) | 174 (56.68) | 133 (43.32) | ||
| Fairly bad (n=25) | 12 (48.00) | 13 (52.00) | ||
| Very bad (n=7) | 3 (42.86) | 4 (57.14) | ||
| Sleep latency | No (n=243) | 158 (65.02) | 85 (34.98) | 0.016 |
| Low (n=227) | 140 (61.67) | 87 (38.33) | ||
| Moderate (n=64) | 32 (50.00) | 32 (50.00) | ||
| Severe (n=32) | 15 (46.88) | 17 (53.13) | ||
| Sleep duration (h) | >7 (n=326) | 208 (63.80) | 118 (36.20) | 0.104 |
| 6-7 (n=190) | 109 (57.37) | 81 (42.63) | ||
| 5-6 (n=42) | 24 (57.14) | 18 (42.86) | ||
| <5 (n=8) | 4 (50.00) | 4 (50.00) | ||
| Sleep efficiency (%) | ≥85 (n=512) | 319 (62.30) | 193 (37.70) | 0.0348 |
| 75-84 (n=35) | 20 (57.14) | 15 (42.86) | ||
| 65-74 (n=13) | 4 (30.77) | 9 (69.23) | ||
| <65 (n=6) | 2 (33.33) | 4 (66.67) | ||
| PSQI | <5 (n=438) | 280 | 158 | 0.001 |
| ≥5 (n=128) | 65 | 63 |
An objective assessment of sleep by actigraphy was done for 96 participants (Table III). The median SL for all the participants was 27.5 min (Range: 1-155 min). The median sleep efficiency was seen to be lower in those reporting a low total mobile phone usage as compared to high users [Median (range)=37.5% (0-130.5) vs. 75% (3.5-96.8); P=0.04]. Furthermore, the average SL over three days in users with low usage was higher than in those with a high usage [Median (range)=33.17 min (1-155) vs. 22.71 (1-92); P=0.04]. The average WASO for the period of observation was also seen to be higher among low mobile phone users although the difference was not significant.
| Parameter | Low usage | High usage | P | ||
|---|---|---|---|---|---|
| n | Median (range) | n | Median (range) | ||
| WASO day one | 47 | 45 (1-211) | 43 | 44 (2-430) | 0.93 |
| WASO day two | 45 | 43 (1-300) | 43 | 47.5 (2-991) | 0.45 |
| WASO day three | 36 | 42.25 (2-298) | 40 | 44.5 (1-208) | 0.79 |
Mann–Whitney U-test. WASO, wake after sleep onset
A polysomnographic study was done for 95 participants (Table IV). The mean TST was 343 ± 93 min with a mean sleep efficiency of 83.1 per cent. The TST, sleep efficiency and SL were similar in the two groups of mobile phone usage. However, the latency from sleep onset to N2 and N3 sleep stages were significantly shorter in participants having a higher mobile phone usage as compared to those with a lower usage [Median (range):13.5 min (1.5-109) vs. 6.5 min (0-89); P=0.02] and [Median (range): 49 min (8.5-220.5) vs. 28.75 min (0-141); P=0.03], respectively.
| Parameter | Low usage | High usage | P | ||
|---|---|---|---|---|---|
| n | Median (range) | n | Median (range) | ||
| Total sleep time | 46 | 352 (148.5-527) | 48 | 322.25 (158.5-516) | 0.27 |
| Sleep efficiency | 46 | 86.4 (59.9-98) | 49 | 86 (45.3-855) | 0.97 |
| Sleep latency | 46 | 15 (0-90) | 49 | 14 (1-116) | 0.14 |
| WASO | 46 | 35 (5-114.5) | 49 | 38.5 (4-182) | 0.38 |
| N1 | 45 | 77 (7.5-197) | 43 | 54 (8.5-218) | 0.51 |
| N2 | 45 | 139.5 (71-238) | 43 | 127 (39-236) | 0.61 |
| N3 | 45 | 80.5 (15.5-251) | 43 | 78 (0-226) | 0.63 |
| REM | 45 | 39 (0-111) | 43 | 29 (0-153) | 0.38 |
| N1% | 45 | 19.6 (2.8-58.4) | 43 | 21.4 (3.3-84.8) | 0.80 |
| N2% | 45 | 41.4 (20.2-69.9) | 43 | 42.2 (10.75) | 0.77 |
| N3% | 45 | 23.6 (4.3-61.8) | 43 | 24.10 (0-55.10) | 0.81 |
| REM% | 45 | 10.3 (0-23.6) | 43 | 9.9 (0-31.7) | 0.91 |
| Latency N1 - sleep onset | 39 | 0 | 33 | 0 (0-34.5) | 0.27 |
| Latency N2 - sleep onset | 39 | 13.5 (1.5-109) | 33 | 6.5 (0-89) | 0.02 |
| Latency N3 - sleep onset | 39 | 49 (8.5-220.5) | 32 | 28.75 (0-141) | 0.03 |
| Latency REM - sleep onset | 38 | 148 (0-400) | 31 | 154 (49-343.5) | 0.67 |
N, non-rapid eye movement; REM, rapid eye movement; WASO, wake after sleep onset
Discussion
High mobile use is a risk factor for sleep disturbance. Sufficient sleep and recovery is an established predictor of physical and psychological well-being, also among adolescents and young adults16171819202122. Sleep disturbances are more prevalent among high mobile phone users due to an increase in SL. Usage of mobile phone at bedtime, significantly increases SL and adversely affects sleep5,23,24. Calls and text messages received during sleeping hours may lead to recurrent night awakenings.
In this study, subjective sleep quality was evaluated with the help of the PSQI questionnaire wherein a score ³5 was indicative of poor sleep. Our findings were coherent with similar studies in the past where exposure to light and altered melatonin metabolism has been implicated in sleep disturbances caused due to mobile phone usage25. In the current study, quantification of mobile phone use was done only by interviewing the study participants. Several studies have used parameters such as average mobile screen usage time, mobile after the lights have been turned off and using mobile in pre bed time etc2627.
Previous studies have found that mobile phone usage, especially near bedtime worsens sleep quality as assessed by PSQI5,24,28,29. Because PSQI relies on the administration of a questionnaire to assess various parameters, it becomes vulnerable to self-reporting bias26 where participants may give biased answers because of their perspective, beliefs and expectations. Because the degree of usage of mobile phones was based on self-reporting, there might have been under-as well as overestimation27282930 of the effect of usage on the parameters being studied based on factors such as age, sex and educational qualification3132.
The actigraphy data showed an increase in sleep efficiency and a decrease in SL in patients with higher mobile phone usage while the average WASO was similar in the two groups. In the PSG subgroup, the sleep efficiency and SL were similar in the two groups. However, the latency to N2 and N3 sleep stages from sleep onset were shorter in the group with higher mobile phone use. These findings appear to be in conflict with the available literature. In a cross-sectional study in 2400 adolescents from 46 schools in Iran, SL was 24±21and 20±18 min in cell phone users and non-users, respectively33, suggesting that cell phone users had significantly higher SL than non-users (P<0.001) similar to our study where higher use for call/SMS was associated with higher sleep latencies.
In a cross-sectional study based on 9846 adolescents from Norway, 90 per cent of the adolescents reported to use their mobile phone in the hour before going to bed and this was related to self-reported sleep onset latency and sleep deficit34. The PSG subgroup showed that TST was non-significantly associated with mobile phone usage with participants with higher mobile phone usage having a reduction in overall sleep time as assessed by PSG.
SL showed a trend towards being higher in cases with high mobile phone use but the difference fell short of being significant. Similar changes were not observed in the WASO parameter. The increase in sleep efficiency and decrease in SL in high mobile phone users on actigraphy may be explained by the possible bias induced on account of being monitored. While being monitored by actigraphy, the participants likely avoided mobile phone use during sleep. As suggested by poor subjective sleep quality among high mobile phone users, it could be possible that this subgroup was sleep deprived and consequently compensated for sleep loss on the preceding days with an increase in sleep efficiency and a decrease in average latency on actigraphy. It has been reported that the effect of sleep deprivation on PSG is a rebound increase in TST, sleep efficiency and increased percentage of N3 sleep along with a decrease in REM latency and SL from lights off35. In PSG in participants with high mobile phone usage, a decrease was found in latency to N2 and N3 from sleep onset. The clinical significance of the same is not clear; however, this may represent an attempt to consolidate sleep and compensate for poor sleep on preceding days36. One may speculate that a first night effect during in-lab PSG might have nullified any effect of mobile phone use on recorded sleep efficiency and SL37.
Our study had certain limitations. We used number of calls and text messages as a measure of total phone use. In recent times, patterns of mobile phone use have changed with increasing use of social media platforms for messaging. A more objective quantification was not feasible as participants were using different makes of the mobile phones, wherein, usage data were not retrievable from the phones uniformly. Several participants had changed their devices in the previous few weeks or months. In conclusion, our study addresses an important question and paves the way for further studies looking at the relationship between all facets of smart phone usage and their impact on objectively measured sleep quality. Though the observational nature of the study may not fully account for all possible confounding factors in subgroups, but, dose-response between sleep quality and mobile phone use observed in our study supports the hypothesis that mobile phone use may alter sleep habits.
Acknowledgment
Authors acknowledge the support of all staff of Sleep Laboratory of the department of Medicine, AIIMS, New Delhi.
Financial support & sponsorship: This research received grant from Science and Engineering Research Board (SERB), Department of Science and Technology, Government of India, New Delhi.
Conflicts of Interest: None.
References
- Public health and the radio frequency radiation emitted by cellphone technology, smart meters and WiFi. N Z Med J. 2018;131:97-107.
- [Google Scholar]
- No evidence for increased brain tumour incidence in the Swedish National Cancer Register between years 1980-2012. Anticancer Res. 2019;39:791-6.
- [Google Scholar]
- Symptoms and cognitive functions in adolescents in relation to mobile phone use during night. PLoS One. 2015;10:e0133528.
- [Google Scholar]
- Effects of mobile phone use on driving performance in a multiresource workload scenario. Traffic Inj Prev. 2019;20:37-44.
- [Google Scholar]
- Effects of smartphone overuse on headache, sleep and quality of life in migraine patients. Neurosciences (Riyadh). 2019;24:115-21.
- [Google Scholar]
- Distracted driving and risk of road crashes among novice and experienced drivers. N Engl J Med. 2014;370:54-9.
- [Google Scholar]
- Subjective symptoms, sleeping problems, and cognitive performance in subjects living near mobile phone base stations. Occup Environ Med. 2006;63:307-13.
- [Google Scholar]
- Mobile phone use and stress, sleep disturbances, and symptoms of depression among young adults –A prospective cohort study. BMC Public Health. 2011;11:66.
- [Google Scholar]
- Occupational electromagnetic field exposures associated with sleep quality:A cross-sectional study. PLoS One. 2014;9:e110825.
- [Google Scholar]
- The association between use of mobile phones after lights out and sleep disturbances among Japanese adolescents:A nationwide cross-sectional survey. Sleep. 2011;34:1013-20.
- [Google Scholar]
- The Pittsburgh Sleep Quality Index:A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193-213.
- [Google Scholar]
- Rules for scoring respiratory events in sleep:Update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8:597-619.
- [Google Scholar]
- Sleepless in adolescence:Prospective data on sleep deprivation, health and functioning. J Adolesc. 2009;32:1045-57.
- [Google Scholar]
- Effect of sleep deprivation on the human metabolome. Proc Natl Acad Sci U S A. 2014;111:10761-6.
- [Google Scholar]
- Sleep deprivation and circadian disruption:Stress, allostasis, and allostatic load. Sleep Med Clin. 2015;10:1-10.
- [Google Scholar]
- Sleep deprivation increases formation of false memory. J Sleep Res. 2016;25:673-82.
- [Google Scholar]
- The relationship between media use in the bedroom, sleep habits and symptoms of insomnia. J Sleep Res. 2011;20:569-75.
- [Google Scholar]
- The effect of smartphone usage at bedtime on sleep quality among Saudi non- medical staff at King Saud University Medical City. J Family Med Prim Care. 2019;8:1953-7.
- [Google Scholar]
- Effects of VDT tasks with a bright display at night on melatonin, core temperature, heart rate, and sleepiness. J Appl Physiol. 2003;94:1773-6.
- [Google Scholar]
- Evaluation of mobile phone addiction level and sleep quality in university students. Pak J Med Sci. 2013;29:913-8.
- [Google Scholar]
- A study of mobile phone usage on sleep disturbance, stress and academic performance among medical students in Tamil Nadu. Int J Community Med Public Health. 2017;5:365-8.
- [Google Scholar]
- Impact of smartphone use on quality of sleep among medical students. Int J Community Med Public Health. 2017;5:101-9.
- [Google Scholar]
- Comparing the self-report and measured smartphone usage of college students:A pilot study. Psychiatry Investig. 2017;14:198-204.
- [Google Scholar]
- The effects of recall errors and of selection bias in epidemiologic studies of mobile phone use and cancer risk. J Expo Sci Environ Epidemiol. 2006;16:371-84.
- [Google Scholar]
- Educational differences in the validity of self-reported physical activity. BMC Public Health. 2015;15:1299.
- [Google Scholar]
- Understanding student self-reports of academic performance and course-taking behavior. AERA Open. 2017;3:1-14.
- [Google Scholar]
- The association of sleep and late-night cell phone use among adolescents. J Pediatr (Rio J). 2017;93:560-7.
- [Google Scholar]
- Sleep and use of electronic devices in adolescence:Results from a large population-based study. BMJ Open. 2015;5:e006748.
- [Google Scholar]
- Clinical neurology for psychiatrists (6th ed). Philadelphia: Saunders; 2007.
- Broadband sound administration improves sleep onset latency in healthy subjects in a model of transient insomnia. Front Neurol. 2017;8:718.
- [Google Scholar]
- First night effect for polysomnographic data in children and adolescents with suspected sleep disordered breathing. Arch Dis Child. 2006;91:233-7.
- [Google Scholar]






