Translate this page into:
A preliminary study of natural history of mild traumatic brain injury by using multidimensional approach
Reprint requests: Dr. Bhagavatula Indira Devi, Department of Neurosurgery, National Institute of Mental Health & Neurosciences, Bengaluru 560 029, Karnataka, India e-mail: drindiradb@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Spectrum of post-traumatic symptoms is frequent among mild traumatic brain injury (mTBI) patients. They account for symptoms in 30-80 per cent of patients during 3-4 months and 20-30 per cent of patients six months post-injury. There are no studies from India in this area. The present longitudinal study was conducted to evaluate the natural recovery of post-traumatic symptoms in mTBI patients.
Methods:
Twenty five mTBI patients presenting with initial Glasgow coma scale score of 15 were recruited initially 2-3 wk post-injury. All patients were followed up twice, after 3-4 and 6-7 months. The patients were evaluated with neuropsychological test, post-traumatic symptoms and quality of life after injury.
Results:
Sustained attention and sensory registration were first to improve. Memory and executive domains improved partially until three months and then after complete recovery. However, a few facets of learning/memory did not improve even at six months. The post-traumatic symptoms decreased since baseline from 76 to 52 per cent at 3-4 months and further to 28 per cent at 6-7 months. The quality of life improved partially from baseline till 3-4 months and much more by 6-7 months.
Interpretation & conclusions:
The study findings showed the course of changes in cognition, traumatic symptoms and quality of life since the time of injury till 6-7 months post-injury. Though majority of post-traumatic symptoms recovered after mTBI without any intervention, but residuals were not uncommon.
Keywords
mild traumatic brain injury
natural recovery
neuropsychological test scores
post-traumatic symptoms
quality of life after injury
Traumatic brain injuries (TBIs) are a major public health problem in India. Mild TBI (mTBI) accounts for nearly 80-90 per cent of total brain injuries, and the requirement of neurosurgical intervention is <1 per cent123. The mTBI group of patients manifests symptoms in multi spectrum such as cognitive, somatic, psychosocial, behavioral and emotional. These manifestations are more evident during acute stages in about 30-80 per cent of patients and resolves within a few days to weeks among majority of them, and in about 20-26 per cent of patient, the symptoms persist for longer duration456. The mTBI patient group manifesting with post-traumatic symptoms may or may not have any abnormal lesions on conventional imaging. These patients are only treated for troubling somatic symptoms. Over-time, the post-traumatic symptoms resolve without any intrusions. The natural course of post-traumatic symptoms recovery is well documented in many developed countries45. In India, neurological disability is 3rd epidemic among which brain injury is a major cause7. However, despite the increase in TBI burden, the research in post-traumatic symptoms recovery of mTBI area is less known, emphasizing the need for detailed research. There are no studies from India that have focused on exploring the natural way of post-traumatic symptoms recovery in mTBI patients. The aim of the current longitudinal study was to investigate the natural history of post-traumatic symptoms in mTBI patients.
Material & Methods
This study was conducted in the departments of Clinical Neurosciences and Neurosurgery, and Clinical Psychology, National Institute of Mental Health & Neurosciences (NIMHANS), Bengaluru, India, during December 2011 to December 2013. The patients were selected from Neurotrauma Emergency Centre, NIMHANS. All patients gave written informed consent and study was approved by the institutional Ethics Committee.
The operational definition8 of mTBI was patients with neurotrauma manifesting with loss of consciousness (LOC) <30 min, post-traumatic amnesia less than 24 h and Glasgow coma scale (GCS) score of 15 and with normal computed tomography (CT) scan findings. The inclusion criteria were patients satisfying mentioned operational definition, between 18 and 40 yr of age group, minimum of high school education qualification and patients willing for three follow ups. The exclusion criteria included prior neuropsychiatric illness/symptoms, alcohol or drug dependence, previous history of brain injury, existing or any previous neurological illness and contraindication to undergo magnetic resonance imaging. No neurorehabilitation was suggested for these patients except for medical treatment.
The neuropsychological test (NPT) assessment was digit symbol substitution test (DSST) and digit vigilance test (DVT) for attention; Rey's auditory verbal learning test (RAVLT) and Rey's complex figure test (CFT) for memory and animal naming test (ANT), spatial span test, verbal n back test and Stroop test for executive function. The test scores were compared with standard population scores that are widely used for standard Indian population developed by the department of Clinical Psychology9. The post-traumatic symptoms were assessed with the Rivermead post-concussion symptoms questionnaire10. Patients having more than four symptoms in Rivermead scale had post-traumatic symptoms10. The quality of life was assessed for thinking abilities, emotional view and independent in daily function, social relationship, bothered about feelings and physical problem. It was assessed using quality of life after brain injury (QOLIBRI) scale11. The average scores of all the domains of QOLIBRI are calculated expected between the range of 0 and 100, higher the scores better and lower the scores worst the quality of life.
Statistical analysis: The data followed normal distribution and variances were equal on comparing with post-period values with the basal values, therefore, parametric test was applied. The mean scores of all NPTs, Rivermead concussion symptoms and QOLIBRI were compared between early, first and second time interval for any significant changes using repeated measures of analysis of variance (ANOVA). Greenhouse-Geisser correction was applied when sphericity was violated. The post-injury symptoms scores were correlated with corresponding quality of life scores using Pearson correlation test.
Results
A total of 25 patients (20 men) underwent baseline neuropsychological assessment with follow ups on 3-4 and 6-7 months. Road traffic accident (RTA) was major cause of injury contributing to 16 (64%), followed by falls (n=7, 28%) and assault (n=2, 8%) with mean age of 26.32±4.91 yr and mean education of 12.44±2.66 yr. The mean duration for early assessment was 12.71 days; first assessment was 105.88 days; second assessment was 226.18 days. All patients had LOC with mean duration of 11.24±10.19 min; less than five minutes was seen in 16 (64%), 6-15 min was seen in four (16%) and 16-30 min was seen in five (20%); 12 (48%) patients had 1-2 episodes of vomiting; 24 per cent (n=6) patients had post-traumatic amnesia lasting for 6-24 h; only 2 (8%) patients had seizures <36 h since injury.
The results on cognitive scores at baseline showed that the initial NPT scores were lower than that of normal population scores. Over time the improvement was as follows: sustained attention (DSST) and sensory registration (verbal n back) improved completely during two weeks to three months. Response speed (DVT), response inhibition (Stroop test), visuo spatial memory (spatial span) and visuoconstructive ability (CFT), immediate and delayed recall improved partially from baseline till three months, complete recovery within 3 to 6 months. Encoding and retrieval (RAVLT) portion of learning/memory and category fluency (ANT) improved during 3-6 months (Table). Patients with traumatic amnesia and seizures also improved.
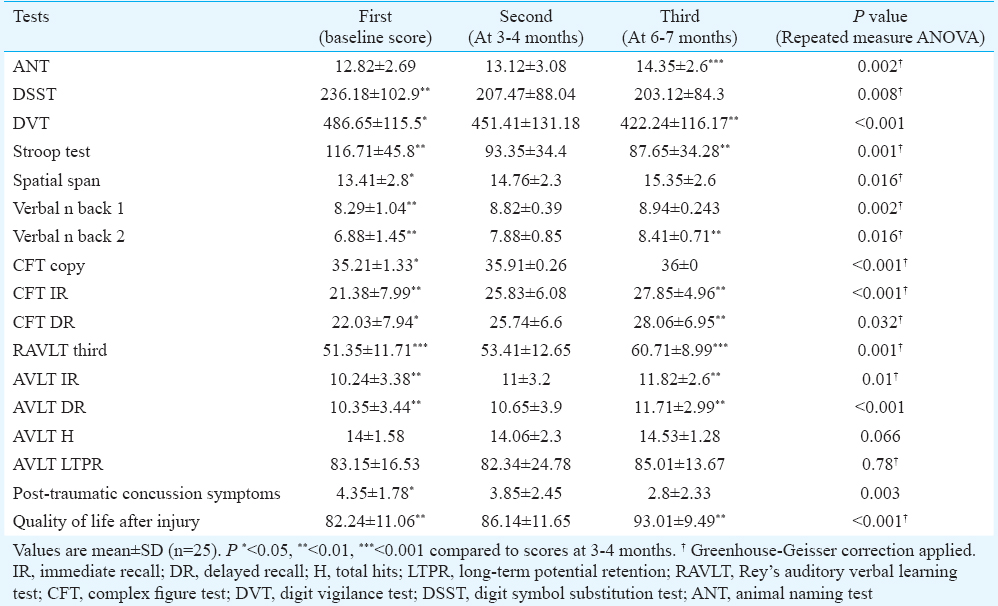
During 2-3 wk 76 per cent, 3-4 months 52 per cent and 6-7 months 28 per cent of mTBI patients manifested with post-traumatic symptoms. Common symptoms that were present from baseline till 6-7 months were headache, fatigue, sleep disturbance, irritability, poor concentration, and longer time to think. All quality of life spheres improved partially from baseline till 3-4 months and to some more extent during 6-7 months. Symptoms at three time points post-injury showed significant negative correlation with corresponding quality of life scores (P<0.001), indicating that the decrease in post-injury symptoms was associated with increase in quality of life scores. In addition, the differences between first and third interval's quality of life scores and with corresponding post-injury symptom scores were significant with negative correlation (P=0.009).
Discussion
The study demonstrated that the attention was the first cognitive function that improved early followed by executive function that got better slowly and the memory was the last higher mental function. During 2-3 wk post-injury nearly three-fourth of patients had post-traumatic symptoms, which on 3-4 months reduced to half of the total patients. During 6-7 months, 28 per cent of patients had persistent symptoms. The thinking capabilities, feeling emotional, independence in daily function, social relationship, bothered about feelings and physical problem improved significantly (P<0.001) from 82.24 to a score of 93.01. Improvement in quality of life was associated with a decrease in post-traumatic symptoms.
For comparison of variables with seizures and amnesia our sample was too small, but on observational basis, the present study that specifically focused on GCS 15 showed that patients with amnesia and seizures also recovered similar to patients without any neurological symptoms during injury. Even though the recovery was expected to be good in this group the persistence of post-traumatic symptoms percentages was slightly more than literature12131415 (that constitutes GCS score of 13, 14 and 15).
The cognitive disturbance has been studied based on CT image finding in mTBI patients. The patients were categorized into uncomplicated (normal CT findings) and complicated groups (abnormal CT findings). In one study, each group had 14 patients assessed within 40 days of injury with age- and gender-matching healthy volunteers. The cognitive impairment was greater in complicated as compared to uncomplicated patients, but the uncomplicated group showed significant impairment compared to a control group6. In another study constituting paediatric mTBI patients, there was no difference existed on attention and memory domains between these two groups at seven years post-injury16. In the present study, all patients had normal CT findings (uncomplicated) and improvement was noted in attention, executive function and memory domains in descending order by 6-7 months.
There are reports of sports-related studies on concussion injury which evaluated neuropsychological functioning from very acute period (<24 h) till one month post-injury with serial evaluation in between. The results reveal that the majority of cognitive impairment resolves in 5-10 days durations1213. Forty mTBI patients injured by various modes were evaluated during 48 h and one month. Patients with LOC presented with improvements in directed attention scores and distractibility, but had not reached to normal values by one month14.
Tellier et al17 showed that regardless of traumatic amnesia at presentation cognitive scores were virtually at normative levels at one month post-injury. In the present study, one-fourth of patients with amnesia improved in cognitive domains similar to other patients who had no amnesia, but the duration required for improvement was longer. In another study cognitive testing was performed at 24 h and three months post-injury in mTBI patients. The cognitive impairment was reported by 44 per cent of the patients on the first day and by 26 per cent at three months post-injury15. In our study patients with sustained attention (DSST), sensory registration (Verbal n Back) improved completely in 3-4 months after injury. The response speed (DVT) and inhibition (Stroop test), visuo-spatial (spatial span) and constructive ability (CFT) improved partially.
Norrie et al4 evaluated serial cognitive test in 37 mTBI patients. During the first week of assessment, the deficits were evident in verbal learning and speed of processing. At 3 and 6 months, the scores improved but with some deficits on verbal learning. In the present study, encoding and retrieval on RAVLT and category fluency (ANT) improved completely during 3-7 months after injury. Response speed (DVT), response inhibition (Stroop test), visuo-spatial (spatial span) and constructive ability (CFT) improved markedly. The study showed that the long-term potential retention and total hits of RAVLT did not improve completely at 6-7 months post-injury.
Twenty to thirty per cent of mTBI patients manifest with irritability and concentration problem at one month of post-injury14. The mTBI patients did things more slowly, fatiguing quickly and had poor balance compared with controls at three months18. Fatigue, forgetfulness and sleep disturbance were most commonly reported at three months19. Headache, fatigue and sleep disturbance were most commonly reported at six months19. The post-traumatic symptoms reported in literature are 84-67.3 per cent at first week, 29-41 per cent at third month and 14-26.4 per cent at sixth month4520. In the current study, post-traumatic symptoms declined in mTBI patients from 76 per cent at baseline to 52 per cent at 3-4 months and further to 28 per cent at 6-7 months. Possible reasons in this study for higher per cent of post-traumatic symptoms could be as follows: (i) The patient's pre morbid status was not known, because normal healthy individuals also manifest with higher percentage of post-traumatic symptoms21. (ii) Patients’ perceptions of their illness that their symptoms have serious negative consequences on their lives may be a risk factor for their persistence of traumatic symptoms22. (iii) mTBI due to motor vehicle collisions, falls and assault have a higher chances of persistent symptoms that may be related to traumatic experience itself, where the trauma is often unexpected, may cause emotionally charged or associated with multiple factors23. However, the exact reason for this is not known.
The quality of life assessed by QOLIBRI scale revealed significant improvement after injury. Improvement in quality of life was associated with a decrease in post-traumatic symptoms. On rehabilitation, the quality of life improved with a decrease in severity and number of symptoms2425.
In conclusion, our study showed significant improvement in cognitive impairment, post-traumatic symptoms and quality of life between 12 and 105 days. Further improvement was seen up to 226 days after injury without any intervention. However, the improvement was not complete, and there were residual symptoms seen.
References
- Epidemiology of traumatic head injury from a major paediatric trauma centre in New South Wales, Australia. ANZ J Surg. 2014;84:424-8.
- [Google Scholar]
- Institute of Trauma and Injury Management. Classification of Head Injuries. 2014. Available from: http://www.itimnswgovau/wiki/Classification_of_head_injuries
- [Google Scholar]
- Mild traumatic brain injury and fatigue: A prospective longitudinal study. Brain Inj. 2010;24:1528-38.
- [Google Scholar]
- Postconcussive symptoms after uncomplicated mild head injury. J Head Trauma Rehabil. 1993;8:48-59.
- [Google Scholar]
- Cognitive and affective sequelae in complicated and uncomplicated mild traumatic brain injury. Brain Inj. 2003;17:189-98.
- [Google Scholar]
- Centers for Disease Control and Prevention. Traumatic Brain Injury & Concussion. Updated Mild Traumatic Brain Injury Guidelines for Adults. Available from: https://www.cdc.gov/traumaticbraininjury/mtbi_guideline.html
- [Google Scholar]
- NIMHANS neuropsychology battery-2004 manual (1st ed). Bangalore: National Institute of Mental Health and Neurosciences; 2004.
- The Rivermead Post Concussion Symptoms Questionnaire: A measure of symptoms commonly experienced after head injury and its reliability. J Neurol. 1995;242:587-92.
- [Google Scholar]
- The QOLIBRI – Towards a quality of life tool after traumatic brain injury: Current developments in Asia. Acta Neurochir Suppl. 2008;101:125-9.
- [Google Scholar]
- Neuropsychological test performance prior to and following sports-related mild traumatic brain injury. Clin J Sport Med. 2001;11:23-31.
- [Google Scholar]
- Neuropsychological functioning and recovery after mild head injury in collegiate athletes. Neurosurgery. 1996;39:510-4.
- [Google Scholar]
- Trajectories of cognitive recovery following a minor brain injury. Res Nurs Health. 2002;25:269-81.
- [Google Scholar]
- S100 and cognitive impairment after mild traumatic brain injury. J Rehabil Med. 2005;37:53-7.
- [Google Scholar]
- Long-term executive functioning outcomes for complicated and uncomplicated mild traumatic brain injury sustained in early childhood. Dev Neuropsychol. 2014;39:638-45.
- [Google Scholar]
- The heterogeneity of mild traumatic brain injury: Where do we stand? Brain Inj. 2009;23:879-87.
- [Google Scholar]
- A longitudinal, controlled study of patient complaints following treated mild traumatic brain injury. Arch Clin Neuropsychol. 2004;19:805-16.
- [Google Scholar]
- When a minor head injury results in enduring symptoms: A prospective investigation of risk factors for postconcussional syndrome after mild traumatic brain injury. J Neurol Neurosurg Psychiatry. 2012;83:217-23.
- [Google Scholar]
- Early predictors of postconcussive syndrome in a population of trauma patients with mild traumatic brain injury. J Trauma. 2009;66:289-96.
- [Google Scholar]
- Examination of “postconcussion-like” symptoms in a healthy sample. Appl Neuropsychol. 2003;10:137-44.
- [Google Scholar]
- Does brief loss of consciousness affect cognitive functioning after mild head injury? Arch Clin Neuropsychol. 2000;15:643-8.
- [Google Scholar]
- Ontario Neurotrauma Foundation. Guidelines for Concussion/Mild Traumatic Brain Injury & Persistent Symptoms, Second Edition, Module 5: General recommendations regarding management of persistent symptoms following mTBI. Toronto, Canada: Ontario Neurotrauma Foundation; 2013.
- [Google Scholar]
- Impact of chronic posttraumatic stress disorder on the quality of life of war survivors. Psychiatr Danub. 2010;22:430-5.
- [Google Scholar]
- Longitudinal analysis of the relationship between symptoms and quality of life in veterans treated for posttraumatic stress disorder. J Consult Clin Psychol. 2006;74:707-13.
- [Google Scholar]






