Translate this page into:
Allergic bronchopulmonary aspergillosis misdiagnosed & incorrectly treated as pulmonary tuberculosis
*For correspondence: sksharma.aiims2@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
A 22 yr old female† was referred to the department of Internal Medicine, All India Institute of Medical Sciences New Delhi, India, in November 2016, with a diagnosis of pulmonary tuberculosis which was not responding to treatment. On interrogation, she had a history of bronchial asthma since childhood. Chest X-ray (Figure A) and high-resolution computed tomography of the chest (Figure B) revealed bilateral upper lobe opacities (right>left) in the both lung fields. Other parameters were suggestive of allergic bronchopulmonary aspergillosis (ABPA) included absolute eosinophil count :1.86 X103/mm3 [(normal:0.02-0.50 electrical impedance; volume, conductivity, light scatter (VCS)]; Aspergillus fumigatus antibodies panel, IgG: >200 U/mL (reference range <8.0), IgM: 1.35 U/mL (reference range <8.00); A. fumigatus precipitins: 12.90 (kUA/L) (reference range <0.35) and, serum immunoglobulin IgE : 11,223.00 kUA/L (reference range <64) (FEIA). With the diagnosis of allergic bronchopulmonary aspergillosis (ABPA), she was treated with oral prednisolone 60 mg/day which was gradually tapered off over the next six months, itraconazole (200 mg twice daily) and inhalational bronchodilators (steroids and β agonists). She responded significantly to the treatment (Figure C). She was put on metered-dose inhalers and is doing well on follow up till date. In this case, ABPA was misdiagnosed and incorrectly treated as pulmonary TB.
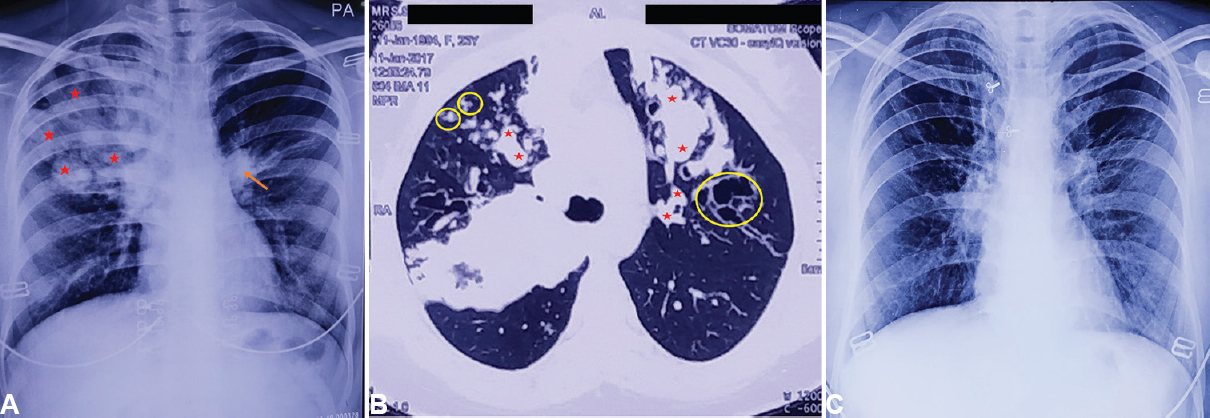
- (A) Pre-treatment chest X-ray (posteroanterior view) and (B) high-resolution computed tomography chest showing opacities (asterisks, arrows and circles) in both lung fields due to mucocoeles (right lung>left lung). (C) Post-treatment chest X-ray (posteroanterior view) showing almost clearing of opacities.
Conflicts of Interest: None.





