Translate this page into:
The need for targeted behavioural HIV-related interventions for transgender women in India: A scoping review
For correspondence: Dr Katie B. Biello, Departments of Behavioral & Social Sciences and Epidemiology, Brown University School of Public Health, 121 South Main Street, Providence, RI 02912, USA e-mail: katie_biello@brown.edu
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Transgender women (TGW) in India are at high risk of HIV infection. Despite behavioural interventions aimed at reducing HIV risk, no literature synthesis exists so far to evaluate their potential for reducing HIV incidence in India This review was aimed to identify and evaluate HIV-focussed behaviour change interventions for TGW in India.
Methods:
Literature from three databases were reviewed up to June 2, 2021, for studies describing behavioural interventions for HIV prevention among TGW in India. The inclusion criteria were studies that included TGW and reported intervention effects on HIV prevention-related behaviour. Data were analyzed descriptively.
Results:
Of the 146 articles screened, only three met the inclusion criteria. All three interventions were at the open pilot trial stage and included other high-risk groups (e.g. men who have sex with men). The interventions used behavioural counselling, increased sexually transmitted infection screening and sexual healthcare visits and leveraged community-based organizations to improve the outcomes. All these interventions showed modest improvements in health-seeking behaviour and access to services. However, none specifically targeted TGW.
Interpretation & conclusions:
The scoping review highlights the need for behavioural interventions for HIV prevention tailored to TGW in India. This study emphasizes the need for research to move to the next stage of intervention development and testing utilizing more rigorous evaluation methods, such as a randomized controlled trial.
Keywords
Behavioural interventions
HIV prevention
transgender women
The Indian HIV epidemic is the third largest in the world, and transgender women (TGW) have been affected disproportionately, with a combined HIV prevalence of three per cent, which is significantly higher than the national average of 0.2 per cent1. The prevalence of HIV among TGW varies across different regions of India, with those residing in major cities such as New Delhi, Kolkata, Hyderabad and Mumbai reporting rates as high as 11 per cent2.
The National AIDS Control Programme (NACO) aims to implement targeted interventions led by the key population groups such as female sex workers (FSWs), men who have sex with men (MSM), hijras/transgender individuals, injecting drug users and bridge populations (i.e. migrants and truckers). These initiatives have been successful in increasing condom use, HIV/sexually transmitted infection (STI) testing and linkage to care for TGW3. However, there is a lack of empirical evidence on which strategies best work to improve HIV-related services for TGW in India.
We conducted this scoping review to investigate the current state of the science regarding HIV-related behavioural interventions specific to TGW in India to evaluate, although narratively, behavioural interventions that take into account the unique experiences of TGW in India. TGW in India (also referred to as Hijra, Thirunangai and Jogti hijra – terms that are not completely interchangeable) have been revered in the Hindu culture for centuries4,5. However, while being revered, they are marginalized in modern day India6. TGW in India experiences high rates of violence and stigma, including familial rejection, due to their gender identity7-9. The gender minority stress experienced by TGW increases their vulnerability to depression and drug and alcohol use to cope with the adversities faced9-13.
Moreover, social marginalization often leads to economic marginalization due to difficulty in employment and safe housing. In turn, this marginalization can result in engagement in transactional sex to support themselves9-12. These contextual and psychosocial challenges faced by TGW in India have been shown to be associated with condomless sex, multiple sex partners, lack of utilization of HIV prevention services and delays in healthcare13-16. Despite their marginalized status and elevated HIV risk, studies on HIV risk of TGW in India are scarce10,14,17. Many efficacious HIV prevention and treatment interventions address issues around all key populations in India; however, interventions specific to TGW are limited18-24.
To garner a comprehensive perspective on HIV-related interventions that can improve HIV outcomes for TGW in India, this study aimed to (i) describe the extent of the efforts and strategies that have been employed for HIV prevention and care among TGW in India, and (ii) determine intervention components and theoretical frameworks associated with meaningful behaviour change.
Material & Methods
A scoping review format was used over a systematic review because it allowed us to describe broad themes and analyze current evidence on HIV-related behavioural interventions for TGW25. This is important given the expected heterogeneity in study design, sample size, study setting and study period25.
Three electronic databases, namely Global Health, Web of Science and PubMed were searched. All studies published before June 2, 2021 were retrieved. Search terms for behavioural HIV intervention combined with TGW terms, including subgroups for Hijras were used. Search terms were derived and adapted from a similar review in south-east Asia26. A full search strategy is provided in Appendix.
Inclusion/exclusion criteria: Following the PICO framework27, a study was included if the population comprised TGW or Hijras (also known as Thirunangai and Jogti hijra) from India; if any HIV-related behavioural intervention was included; any study design aimed to assess change in the outcome, including but not limited to randomized controlled, quasi-randomized controlled or, non-randomized controlled studies designed with a comparison group, pre-post without control, quasi-experimental and programme evaluation; and if the study: reported any HIV-related outcome [i.e. increase HIV knowledge, reduction in condomless sex, reduction in the number of sexual partners, improving antiretroviral therapy (ART) adherence and reducing STI/STI symptoms].
The following criteria were used to exclude studies from the review: (i) studies that did not focus exclusively on TGW or did not include gender stratification; (ii) studies that were not original research (e.g. comments, reviews and editorials); and (iii) studies that were not published in English.
Selection of articles for review: The screening process was conducted using the systematic review software, Covidence28, which imported the titles and abstracts of the studies. Two reviewers conducted the screening in two phases. The first phase involved reviewing the title and abstract and examining the full papers. The reviewers independently extracted data from the full text of each study and recorded it in a summary table. The extracted information was then compared and verified to reach a consensus between the two reviewers.
Data extraction: Each article that met the selection criteria was reviewed using a standardized data extraction template, which included study and population characteristics, location, setting, study design, study period, target population, inclusion criteria, overall sample and the number of TGW (Table I). Data were summarized across studies for each pre-determined field.
| Author, year | Study location | Setting | Study design | Study period (in months) | Target population | Inclusion criteria | Total number of participants | Total number of TGW participants |
|---|---|---|---|---|---|---|---|---|
| Selvaraj et al31, 2020 | Tamil Nadu | Clinics | Non-randomized experimental study | 3 | PLWHA (newly diagnosed) | Newly diagnosed with HIV | 100 | 3 |
| Gurung et al29, 2011 | Andhra Pradesh, Tamil Nadu, Maharashtra, Karnataka, Manipur and Nagaland | Clinics | Clinical monitoring/programme evaluation | 59 | High-risk groups (i.e. FSW, MSM, IDU, TW) | Utilization of the clinic for STI-related services | 431,434 | 7328 |
| Shaikh et al30, 2016 | Andhra Pradesh and Telangana, Karnataka, Maharashtra, Tamil Nadu, Uttar Pradesh and West Bengal | CBO/NGO | Cross-sectional study | 58 | MSM and TGW | Registered in the programme for at least six months, were willing to provide written consent to participate voluntarily, had anal sex with a male partner in the last three months and were over 18 yr of age | 433,000 | 268 |
FSW, female sex worker; MSM, men who have sex with men; IDU, injecting drug user; TGW, transgender women; STI, sexually transmitted infection; PLWHA, people living with HIV/AIDS; CBO, community-based organization; NGO, non-governmental organization; N/A, not available
Results
The initial search yielded 146 articles, including 92 unique studies. After screening the titles and abstracts of each article and excluding studies that did not meet the inclusion criteria, 13 studies were read in full to assess eligibility. Ten studies were excluded for the following reasons: three reported results of a larger study that did not include intervention results, two had no TGW in the study, two had no behavioural outcome, two were commentaries and one was a duplicate. Three studies met the final inclusion criteria. The screening process is summarized in the Figure.
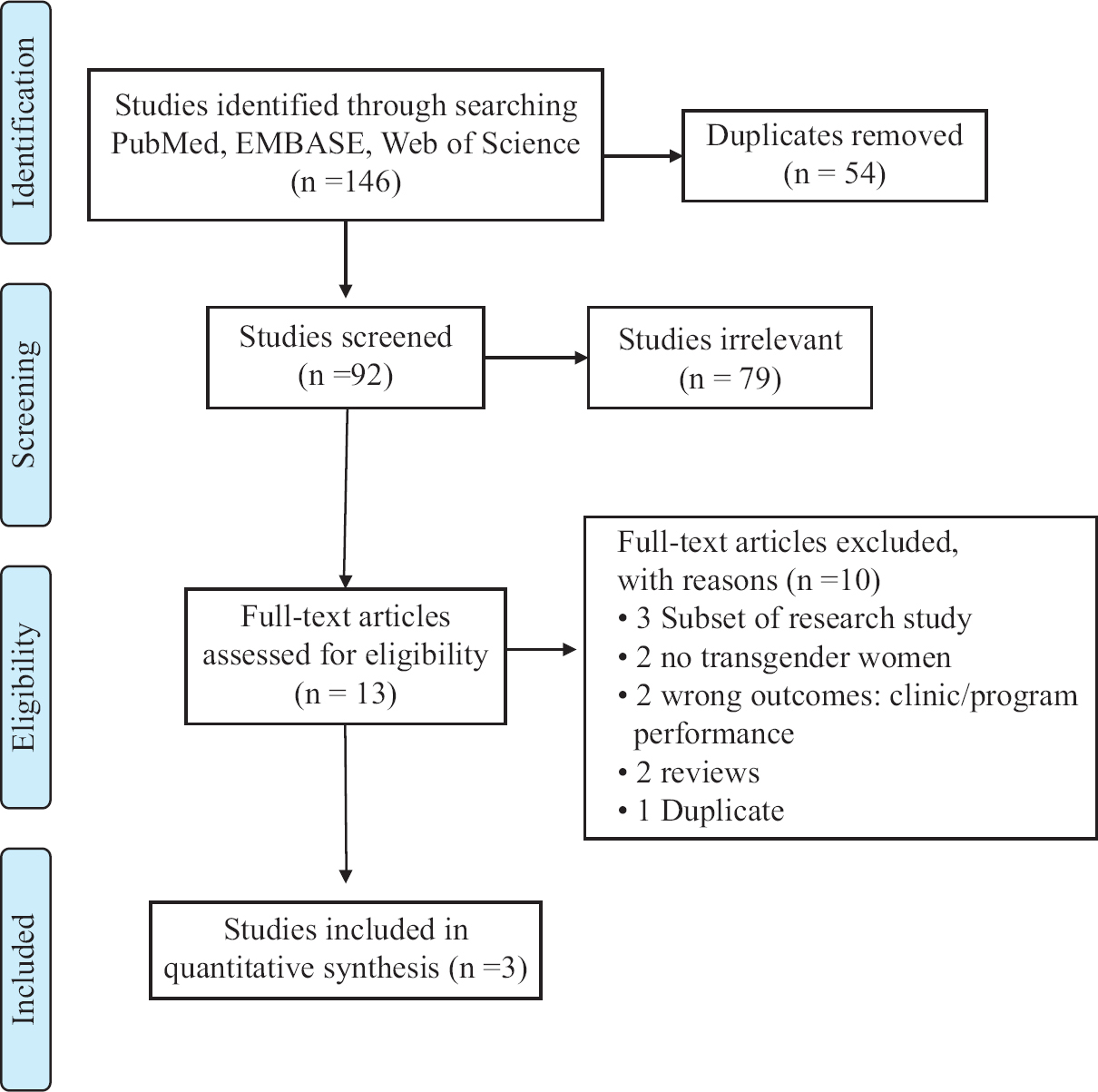
- Flow diagram of included and excluded studies.
Characteristics of study populations: Table I describes the detailed characteristics of the selected studies. Two of the studies were conducted in multiple States, with historically the highest prevalence of HIV, and were representative of the target population29,30. Two studies occurred in clinical settings29,31, and one was through a community-based organization30. While each study had a different study design – including a non-randomized experimental study31, programme evaluation29 and cross-sectional study30; none was a randomized trial. Two of the studies were retrospective cohort studies, examining end-line questionnaires and the number of visits per year to assess intervention impact on the targeted population29,30, and the remaining study was a non-randomized experimental study with a pre and post-questionnaire31. For all three studies, all participants who received the intervention were analyzed. The study period varied from three months to 59 months. None of the studies were specific to TGW; instead, they broadly targeted people living with HIV31, FSW29, MSM29,31 and people who inject drugs29 but also included TGW. Notably, separate analyses specific to TGW were reported in only one study30. One study in this review reports a low number of transwomen enrolled (n=3); however, it was retained and reported here as the intervention criteria included transwomen, which is consistent with the inclusion criteria for this review31.
Characteristics of interventions: Of the three studies, two studies used a theoretical or conceptual framework to ground the intervention, including knowledge, attitude, behaviour and practice31 and a rights-based empowerment framework30; the other study did not mention any theoretical or conceptual framework29. One study targeted multiple levels of behavioural influence – both individual and interpersonal30, while the other two studies were structural29 and individual-level interventions, respectively29,31. Two studies applied provider-patient counselling sessions that targeted TGW and people living with HIV30,31, while one provided increased testing and health-care visits29. All the studies assessed individual-level indicators (Table II), including condom use30,31, disclosure of HIV status to partners31, social support31, mental health status31, access to care29,31, HIV/STI diagnoses29,30, experiences of stigma and discrimination30, awareness of Indian Penal Code Section 37730, instances of abuse and/or intimate partner violence30, awareness of services30 and self-efficacy30. Two assessed the individual outcomes retrospectively using programme data and surveys29,30, and the other surveyed participants every month for three months to assess the behaviour change31. Two studies used programmatic data29,30, and all three used surveys to assess the impact of the intervention. As noted previously, none of the studies recruited samples solely of transwomen; however, two studies conducted an analysis that specifically assessed intervention effects on TGW29,30. One of the studies included three TGW in the results and therefore could not conduct a sub-analysis31. None of the studies reported differences between groups before the intervention. One study reported adjusting for age and subpopulation group in the analysis29. None of the studies reported the acceptability or feasibility of intervention.
| Author, year | Intervention name | Intervention components | Theory/conceptual framework | Outcome measures | Key findings |
|---|---|---|---|---|---|
| Selvaraj et al31, 2020 | N/A | Pre-post-intervention questionnaire (28 questions), Counselling, Follow up every month for three months | KABP | Condom use, revealing HIV status to a spouse, social support/acceptance and mental health status | Increase condom use Low previous HIV awareness Decreased alcohol use No difference in mental health |
| Gurung et al29, 2011 | Avahan program | Syndromic management of symptomatic infections as per the Indian national guidelines Presumptive treatment for gonorrhoea and chlamydia, Quarterly STI check-ups Six monthly syphilis screening. IDUs were provided services for symptomatic STIs and injected-related infections | None | Number of visits per year, STIs diagnosed | Increased health-seeking behaviour, internal examination, regular STI check-ups,-treatment-seeking behaviour with anorectal discharge -treatment-seeking behaviour with anorectal discharge |
| Shaikh et al30, 2016 | Pehchan programme | To improve the organizational capacity of CBOs Support for linkage to care and community-based interventions and creation of a supportive environment for transcommunity | Rights-based empowerment approach, self-efficacy framework | The end-line questionnaire focussed on the sociodemographic characteristics of respondents, their sexual behaviour, including condom use patterns, access and results of HIV testing services, experiences of stigma and discrimination, awareness of Indian Penal Code Section 377, instances of abuse, community and police violence or harassment, collective action and efficacy, exposure to the Pehchan programme, awareness and access of intervention services and biological feminization | Increased access to sexual and reproductive health services Increased HIV testing Increased access to legal, emergency and psychological services |
KABP, Knowledge, Attitude, Behaviour and Practice; IDUs, injecting drug users; STI, sexually transmitted infection; N/A, not available; CBOs, community-based organizations
Discussion
The present review aimed to identify HIV-focussed behaviour change interventions specific to TGW in India. Three studies met our inclusion criteria of having studied the HIV-prevention behavioural interventions that included TGW; however, no studies were identified that specifically targeted TGW. Due to the limited number of studies, it is difficult to generalize the findings to provide a holistic picture of HIV-related interventions for TGW in India. However, it highlights the need for more rigorous interventions that address the barriers specific to TGW (e.g. transphobia, substance use, mental health conditions), which impact condom use, HIV/STI testing, and linkage to care. Nevertheless, the review showed significant improvement in HIV prevention-focussed behaviourar changes, and two studies even included a sub-analysis of TGW and demonstrated the targeted change within this key group.
Although the findings from the reviewed studies are promising, only one intervention programme utilized a behaviour change theory specific to transgender persons, and none specifically targeted TGW. Behavioural change and transgender-specific theoretical approaches are critical to reducing HIV risk32. Studies have shown that interventions that use additional behavioural, social and structural approaches grounded in behavioural theory to target the unique realities of TGW have been shown to be efficacious in reducing HIV risk32,33. Moreover, none of the study designs used a randomized design, which is the gold standard for assessing intervention efficacy. Given this lack of rigour, it is evident that there is a major dearth of research on best practices in HIV prevention and treatment interventions, which poses a challenge to HIV prevention efforts in India since transgender people have one of the highest prevalences of HIV in India34.
Targeted rigorous HIV prevention and treatment interventions for TGW are essential to address the individual, interpersonal, and structural barriers that the TGW experience, which differ from other groups at increased risk of HIV acquisition, including MSM. Although India has recognized that gender is not a binary construct in policy and socio-religious contexts, stigma and discrimination continue to make HIV prevention and treatment efforts for this population difficult35. More work needs to be done to reduce trans-related stigma in this population. Discrimination and familial rejection related to transgender identity are associated with a high prevalence of depression in this population. Internalized stigma has contributed to increased sexual risk-taking, mediated by depression36,37. While there are limited data on which psychosocial issues are related to sexual risk-taking among TGW in India, tailoring behaviour change counselling to this population’s specific needs may reduce HIV incidence13,14. Interventions aimed at increasing cultural humility and knowledge of the healthcare needs of transwomen may attenuate barriers to access care for TGW in India. Structural changes that advance human rights protection and increase safety for TGW are necessary to achieve health equity.
This scoping review highlights that the interventions improved HIV-related behavioural outcomes regardless of methodological quality, behavioural change and transgender-specific theoretical approaches. Most of the studies were evaluations of programmes implemented and reported the effectiveness of the intervention. These studies suggest that the programme’s effectiveness at the population level could be refined in efficacy studies for special populations, given TGW’s psychosocial and contextual differences. This scoping review reveals the lack of interventions specific to TGW and highlights the need for developing interventions that examine the impact of social determinants of health, such as discrimination and stigma, on the HIV-related health outcomes of TGW.
While we aimed to conduct a rigorous review and explore various aspects of HIV interventions among TGW, it is important to note the limitations of this review. The first limitation is that the study elements and intervention components were extracted solely from the papers published in peer-reviewed journals. This means that some relevant information or interventions specific to each State may not have been included in this review. Second, although EMBASE, PubMed and Web of Science catalogue peer-reviewed research across multiple medical and social journals, it does not characterize all available research, specifically grey literature. Third, we used broad inclusion and exclusion criteria to explore behavioural interventions targeted to TGW and their outcomes in India. Because of this, we could not standardize the assessment of the quality of published articles as was possible in a systematic review. Finally, the studies included were non-randomized, which makes it difficult to conclude regarding the effect of behavioural interventions on various HIV-related outcomes. Given the variation of the studies, this review emphasizes the need for further research with larger and more representative samples and with study designs that allow for more robust inferences to be drawn. Although limitations, this scoping review provides a narrative of the current state of interventions with TGW in peer-reviewed research to further future research and interventions.
The findings of this scoping review reveal a concerning lack of targeted HIV prevention and treatment interventions for TGW in India. The review highlights the urgent need for further research to understand the barriers and facilitators to accessing HIV services among TGWs. Such research should consider the multilevel barriers (individual, interpersonal and structural) that TGW face across different States, cities and regions, recognizing the heterogeneity among TGW and their diverse regional identities, such as hijras or other trans identities. It is crucial to acknowledge the unique needs of TGW and not to group them with other high-risk populations, such as MSM when developing HIV interventions.
Future directions: The findings of this scoping review reveal a significant gap in the availability of targeted HIV prevention and treatment interventions for TGW in India. To address this, the following recommendations are made for future HIV-related interventions for TGW: (i) providing culturally sensitive education and resources to promote HIV testing and awareness among TGW; (ii) engaging TGW in HIV prevention and treatment initiatives should be a priority, which can be achieved through deliberate outreach that involves building trust and establishing relationships with TGW communities; and (iii) developing and evaluating interventions that address stigma and discrimination faced by TGW in accessing HIV prevention and treatment services. These interventions should be based on relevant theories, such as Social Identity Theory and Minority Stress Theory, which could inform intervention design and evaluation. Tailored interventions that meet the specific needs of TGW are crucial in promoting their engagement and retention in HIV prevention and care services, including ART, treatment as prevention and pre-exposure prophylaxis. This includes considering the barriers that TGW faces when accessing services and to determine the collective efficacy of these interventions, it may hence be necessary to conduct efficacy trials rather than relying solely on programme evaluations.
Financial support & sponsorship: None.
Conflicts of Interest: Author (LKF) is currently employed at Johnson & Johnson Global Public Health.
References
- Global epidemiology of HIV infection and related syndemics affecting transgender people. J Acquir Immune Defic Syndr. 2016;72(Suppl 3):S210-9.
- [Google Scholar]
- National AIDS Control Organization. HIV sentinel surveillance 2016-17: Technical brief. Available from: http://naco.gov.in/sites/default/files/HIV%20SENTINEL%20SURVEILLANCE_06_12_2017_0.pdf
- National AIDS Control Organization. Prevention progress update 2020-21. New Delhi: NACO; 2021.
- United Nations Development Programme. Hijras/transgender women in India: HIV, human rights and social exclusion. India: UNDP; 2010.
- Negotiating violence: Everyday queer experiences of the law. Violence Gend. 2020;7:141-9.
- [Google Scholar]
- Not this, not that: The Hijras of India and the cultural politics of sexuality. In: Social text, No. 61; Out front: Lesbians, gays, and the struggle for workplace rights. Durham, NC: Duke University Press; 1999. p. :119-40.
- [Google Scholar]
- Barriers to free antiretroviral treatment access among kothi-identified men who have sex with men and aravanis (transgender women) in Chennai, India. AIDS Care. 2011;23:1687-94.
- [Google Scholar]
- Factors associated with sexual violence against men who have sex with men and transgendered individuals in Karnataka, India. PLoS One. 2012;7:e31705.
- [Google Scholar]
- Victimization and human immunodeficiency virus-related risk among transgender women in India: A latent profile analysis. Violence Gend. 2017;4:121-9.
- [Google Scholar]
- Syndemics of depression, alcohol use, and victimisation, and their association with HIV-related sexual risk among men who have sex with men and transgender women in India. Glob Public Health. 2017;12:250-65.
- [Google Scholar]
- Stigma, violence and HIV vulnerability among transgender persons in sex work in Maharashtra, India. Cult Health Sex. 2017;19:903-17.
- [Google Scholar]
- Descriptive epidemiology of factors associated with HIV infections among men and transgender women who have sex with men in South India. LGBT Health. 2016;3:292-9.
- [Google Scholar]
- Understanding how sexual and gender minority stigmas influence depression among trans women and men who have sex with men in India. LGBT Health. 2017;4:217-26.
- [Google Scholar]
- Syndemic classes, stigma, and sexual risk among transgender women in India. AIDS Behav. 2019;23:1518-29.
- [Google Scholar]
- HIV status disclosure and condom use among HIV-positive men who have sex with men and Hijras (Male-to-Female Transgender People) in India: Implications for prevention. J HIV AIDS Soc Serv. 2015;14:26-44.
- [Google Scholar]
- Antiretroviral treatment uptake and adherence among men who have sex with men and transgender women with HIV in Mumbai, India: A cross-sectional study. J Assoc Nurses AIDS Care. 2018;29:310-6.
- [Google Scholar]
- National AIDS Control Organization. Annual report 2012-13. New Delhi: NACO; 2014.
- Association between alcohol use and HIV-related sexual risk behaviors among men who have sex with men (MSM): Findings from a multi-site bio-behavioral survey in India. AIDS Behav. 2014;18:1330-8.
- [Google Scholar]
- A randomized clinical efficacy trial of a psychosocial intervention to strengthen self-acceptance and reduce HIV risk for MSM in India: Study protocol. BMC Public Health. 2018;18:890.
- [Google Scholar]
- Development and open pilot trial of an HIV-prevention intervention integrating mobile-phone technology for male sex workers in Chennai, India. Arch Sex Behav. 2017;46:1035-46.
- [Google Scholar]
- Unseen and unheard: Predictors of sexual risk behavior and HIV infection among men who have sex with men in Chennai, India. AIDS Educ Prev. 2009;21:372-83.
- [Google Scholar]
- A pilot RCT of an intervention to reduce HIV sexual risk and increase self-acceptance among MSM in Chennai, India. AIDS Behav. 2014;18:1904-12.
- [Google Scholar]
- Sexual health promotion in Chennai, India: Key role of communication among social networks. Health Promot Int. 2005;20:327-33.
- [Google Scholar]
- An integrated structural intervention to reduce vulnerability to HIV and sexually transmitted infections among female sex workers in Karnataka state, south India. BMC Public Health. 2011;11:755.
- [Google Scholar]
- Systematic review or scoping review?Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:143.
- [Google Scholar]
- Behavioral interventions to reduce HIV risk behavior for MSM and transwomen in Southeast Asia: A systematic review. AIDS Care. 2017;29:98-104.
- [Google Scholar]
- PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. 2014;14:579.
- [Google Scholar]
- Covidence Systematic Review Software. Veritas Health Innovation, Melbourne, Australia. Available from: https://www.covidence.org
- Large-scale STI services in Avahan improve utilization and treatment seeking behaviour amongst high-risk groups in India: An analysis of clinical records from six states. BMC Public Health. 2011;11(Suppl 6):S10.
- [Google Scholar]
- Empowering communities and strengthening systems to improve transgender health: Outcomes from the Pehchan programme in India. J Int AIDS Soc. 2016;19:20809.
- [Google Scholar]
- Pre- and post-HIV test knowledge, attitude, behavior, and practice of people living with HIV and AIDS by questionnaire pattern. Indian J Sex Transm Dis AIDS. 2020;41:53-7.
- [Google Scholar]
- Behavioral interventions to prevent HIV transmission and acquisition for transgender women: A critical review. J Acquir Immune Defic Syndr. 2016;72(Suppl 3):S220-5.
- [Google Scholar]
- Efficacy of an empowerment-based, group-delivered HIV prevention intervention for young transgender women: The Project LifeSkills Randomized Clinical Trial. JAMA Pediatr. 2018;172:916-23.
- [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. UNAIDS data 2018. Available from: https://www.unaids.org/sites/default/files/media_asset/unaids-data-2018_en.pdf
- Barriers to accessing sexual health services for transgender and male sex workers: A systematic qualitative meta-summary. AIDS Behav. 2020;24:682-96.
- [Google Scholar]
- Sexual behaviour and HIV infection risks in Indian homosexual men: A cross-cultural comparison. Int J STD AIDS. 1991;2:442-4.
- [Google Scholar]
- Internalized homophobia, intimacy, and sexual behavior among gay and bisexual men. In: Stigma and sexual orientation: Understanding prejudice against lesbians, gay men, and bisexuals. Thousand Oaks, California, USA: SAGE Publications, Inc; 1998. p. :160-86.
- [Google Scholar]
Appendix
Search terms used
PubMed
(( “Transgender Persons”[mh] OR transgender*[tiab] OR transsexual* [tiab] OR “hijras” [tiab] OR “aravani” [tiab] AND (sex[tiab] OR sexual[tiab] OR intercourse*[tiab])))) AND ((“Behavior therapy”[mh] OR “Sexual Behavior”[mh:noexp] OR “Safe Sex”[mh] OR “Health education”[mh] OR “Behavior control”[mh]OR “Health behavior”[mh] OR “Health promotion”[mh] OR “Sex education”[mh] OR ((behavior*[tiab] OR behavior* [tiab] OR social*[tiab] OR sociocult*[tiab] OR cultur*[tiab] OR communit*[tiab] OR communicat*[tiab] OR education* [tiab] OR informat*[tiab] OR aware*[tiab] OR network* [tiab] OR guidan*[tiab] OR prevent*[tiab] OR control[tiab] OR controls[tiab] OR condition*[tiab] OR health[tiab] OR healthy[tiab]) AND (therapy[tiab] OR therapeut*[tiab] OR therapies[tiab] OR treat[tiab] OR treated[tiab] OR treatment [tiab] OR treating[tiab] OR interven*[tiab] OR strateg*[tiab] OR modif*[tiab] OR program*[tiab] OR promot*[tiab] OR campaign*[tiab] OR market*[tiab] OR train*[tiab] OR improve*[tiab] OR change*[tiab])) OR ((intervent*[tiab] OR treatment*[tiab] OR train*) AND (program*[tiab] OR strateg*[ tiab])))) AND (“India”[mh])
Web of science
TS = (( trans* OR “hijras” OR “aravani”)) NEAR/3 (sex* OR intercourse*)))) AND ((((behav* OR communit* OR soci* OR sociocult* OR cultur* OR health*) NEAR/3 (therap* OR treatment* OR intervention* OR modif* OR prevent* OR program* OR pro- mot* OR control* OR train* OR improv* OR campaign* OR change*)) OR ((intervention* OR treatment* OR therap* OR promot* OR communicat* OR education* OR improv*) NEAR/3 (program* OR strateg*)))) AND (India*)
Embase
(transgender* OR transsexual*) NEAR/3 (sex* OR intercourse*))):ab,ti) AND (“beha- vior therapy”/exp OR “health education”/de OR “health pro- motion”/de OR “social marketing”/de OR “sexual behavior”/ de OR “safe sex”/de OR “behavior control”/de OR “health behavior”/de OR “sexual education”/de OR “behavior change”/de OR (((behav* OR communit* OR soci* OR socio- cult* OR cultur* OR health*) NEAR/3 (therap* OR treatment* OR intervention* OR modif* OR prevent* OR program* OR promot* OR control* OR train* OR improv* OR campaign* OR change*)) OR ((intervention* OR treatment* OR therap* OR promot* OR communicat* OR education* OR improv*) NEAR/3 (program* OR strateg*))):ab,ti) AND (“Southeast Asia”/exp OR ((Southeast* OR “south east” OR “south eastern”) NEAR/3 (India*)






