Translate this page into:
Diagnostic value of LungPoint navigation combined with EBUS-GS & ROSE in peripheral pulmonary nodules
For correspondence: Dr Xiao-Ju Zhang, Department of Respiratory & Critical Care Medicine, Zhengzhou University People’s Hospital, Zhengzhou, Henan, China e-mail: zcc_0813@163.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Recently, there has been a surge to develop new devices and techniques for the diagnosis of peripheral pulmonary lesions such as the combination of LungPoint navigation and endobronchial ultrasound with a guide sheath (EBUS-GS). The present study aimed to explore the diagnostic value of LungPoint navigation in combination with EBUS-GS and rapid on-site evaluation (ROSE) particularly for peripheral pulmonary nodules.
Methods:
Patients (n=108) with pulmonary nodules (10 mm ≤ nodal diameter ≤30 mm) presenting to Henan Provincial People’s Hospital were detected using chest computed tomographic (CT) scanning and bronchoscopy. All patients were evaluated using LungPoint navigation, EBUS-GS and ROSE techniques to evaluate the positive rate of combined diagnosis using the three methods.
Results:
A total of 108 patients participated in this study and successfully underwent all the three procedures. Of these, 82 patients were accurately diagnosed, making the overall diagnostic rate of 75.9 per cent for combined LungPoint navigation, EBUS-GS, and ROSE analyses. Further subgroup analysis of the diagnostic rate of the three combined techniques were conducted based on the size of the nodules which showed a diagnostic rate of 65.3 per cent for 10 mm ≤ nodule diameter ≤20 mm and 85.7 per cent for 20 mm ≤ nodal diameter ≤30 mm. Of the 108 patients, 85 had solid nodules and 23 had ground-glass nodules; the positive rate of diagnosis of solid nodules was the highest. The patients ultimately were diagnosed with lung cancer with a positive rate of 83.5 per cent. The sensitivity, specificity and positive and negative predicted values for ROSE were 90.3, 78.3, 84.8 and 83.6 per cent, respectively.
Interpretation & conclusions:
The combined use of the three techniques can effectively shorten the duration of the total diagnosis period and improve the safety of diagnosis without affecting the detection rate.
Keywords
EBUS-GS
LungPoint
peripheral pulmonary nodules
ROSE
There are many methods available for the diagnosis of pulmonary nodules. Computed tomography (CT)guided lung biopsy is one of the most used methods, since it has a high positive diagnostic rate and is simple and easy to operate1. Peripheral pulmonary nodules are commonly diagnosed by computed tomography (CT) guided lung biopsy; however, it is often associated with certain complications such as haemorrhages pneumothorax and tumour implantation. Approximately 13 per cent of bleeding complications and 8-15 per cent of pneumothorax complications attributed to CT-guided lung biopsy procedures have also been reported in literature2. In recent years, however, several new bronchoscopic techniques have been developed for the diagnosis of peripheral lung nodules, including virtual bronchoscopic navigation (VBN) combined with endobronchial ultrasound with a guide sheath (EBUS-GS)3. Using VBN alone, pulmonologists are unable to determine whether the guided bronchoscope has reached the navigation area; VBN is vulnerable to the technical limitations of the operator4. Although an electromagnetic navigation bronchoscope system can provide a relatively accurate guidance, it is difficult to use extensively because of the associated expensive consumables5. This study was aimed to evaluate the diagnostic value and safety of LungPoint navigation technology combined with EBUS-GS and ROSE technology for peripheral pulmonary nodules.
Material & Methods
Study design and population: This study was a retrospective analysis of the bronchoscopic procedures performed in the bronchoscopy suite of Henan Provincial People’s Hospital, China, between January 5, 2017 to December 1, 2018. A total of 108 patients were evaluated using the LungPoint navigation system in conjunction with EBUS-GS and ROSE. The study was approved by the Institutional Review Board and informed consent was obtained from all the patients recruited in the study.
Augmented reality navigation (LungPoint) system: The augmented reality navigation (LungPoint) system (Broncus Technologies, Inc., Mountain View, CA, USA) was used to evaluate lung nodules. The Lung Point system is based on computed tomography (CT) data reconstruction technology with ≤1.25 mm layer thickness. Each patient underwent CT examination at the end of deep inhalation to ensure bronchioles were maximally extended6.
Endobronchial ultrasound with a guide sheath (EBUSGS): The Olympus ultrasonic probe (UM-s20-17s 20MHz, Olympus America Inc., Houston, TX, USA) was used, along with the Olympus guide sheath with an external diameter of 1.95 mm. The endotracheal examination was performed by bronchoscopy (P260F, 4.0 mm external diameter, Olympus, Tokyo, Japan). At the location of the diseased bronchus, the ultrasonic probe was used to determine the location and the orientation of the nodules and bronchus. A biopsy was performed via the indwelling guide sheath and a rapid on-site evaluation (ROSE) was used to conduct the specimen evaluation.
Rapid on-site evaluation (ROSE): DiffQuik stain (Beijing Solarbio Science & Technology Co. Ltd, China) was used for rapid staining of the cytological film bases7. The cytological film base was stained within 1-2 min after a biopsy was taken from the target site and transferred to the special microscope for interpretation. Cytological evaluation was conducted by an experienced cytotechnologist, and ROSE analysis revealed cells positive for malignancy.
Operation methods: CT data of the patients with pulmonary nodules were imported into the LungPoint navigation system (Brandies Technologies) and then matched with the bronchoscope to guide the bronchus to the location of the lesion. EBUS-GS was used to conduct a guided biopsy. Based on the ROSE results of the biopsy sample, the patient’s nodules were diagnosed according to the pathological diagnosis. In the event of a doubtful diagnosis, surgical resection was suggested. After six months of follow up, if no changes were found in the nodules, these were considered to be benign.
Statistical analysis: EpiData3.0 (EpiData, Buenos Aires, Argentina) was used to establish a database, which was input independently by two trained researchers. SPSS version 17.0 (IBM Corp, Armonk, NY, USA) statistical software was used for the data analysis. Kolmogorov–Simonov test was applied to determine the normality of data. The data were expressed as mean (standard deviation) and median (range), respectively. The categorical data such as patient sex and smoking status were presented as number and per cent. For each subgroup, the diagnostic rate was calculated as the number of diagnosed patients divided by the total number of patients in the subgroup. The receiver operating characteristic (ROC) curve was used to calculate the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and other indicators to assess diagnostic value of LungPoint and EBUS-GS or ROSE for the detection of benign and malignant disease.
Results
A total of 108 participants were selected in this study to evaluate the diagnostic value of LungPoint, EBUS-GS and ROSE (Figure). The combined use of LungPoint, EBUS-GS and ROSE confirmed the correct diagnosis in 82 participants, of which 53 had malignant tumours [adenocarcinoma (n=38), squamous cell carcinoma (n=8), small cell carcinoma (n=5), non-small cell lung cancer (n=1) and large cell lung cancer (n=1)] and 29 had benign disease [tuberculosis (n=9), bacterial pneumonia (n=8), organizing pneumonia (n=6), non-tuberculous pulmonary mycobacteriosis (n=3), fungal infection (n=2) and inflammatory pseudotumour (n=1)]. Among the 26 patients without a definite diagnosis, 13 participants were evaluated with CT-guided lung biopsy, of which 10 were definitively diagnosed, while three were not. In six of them, the endotracheal examination (combined LungPoint+EBUS-GS+ROSE) was repeated, after which the diagnosis was clear in three participants but not in the other three. Surgical resection was performed in seven patients with a definitive diagnosis.
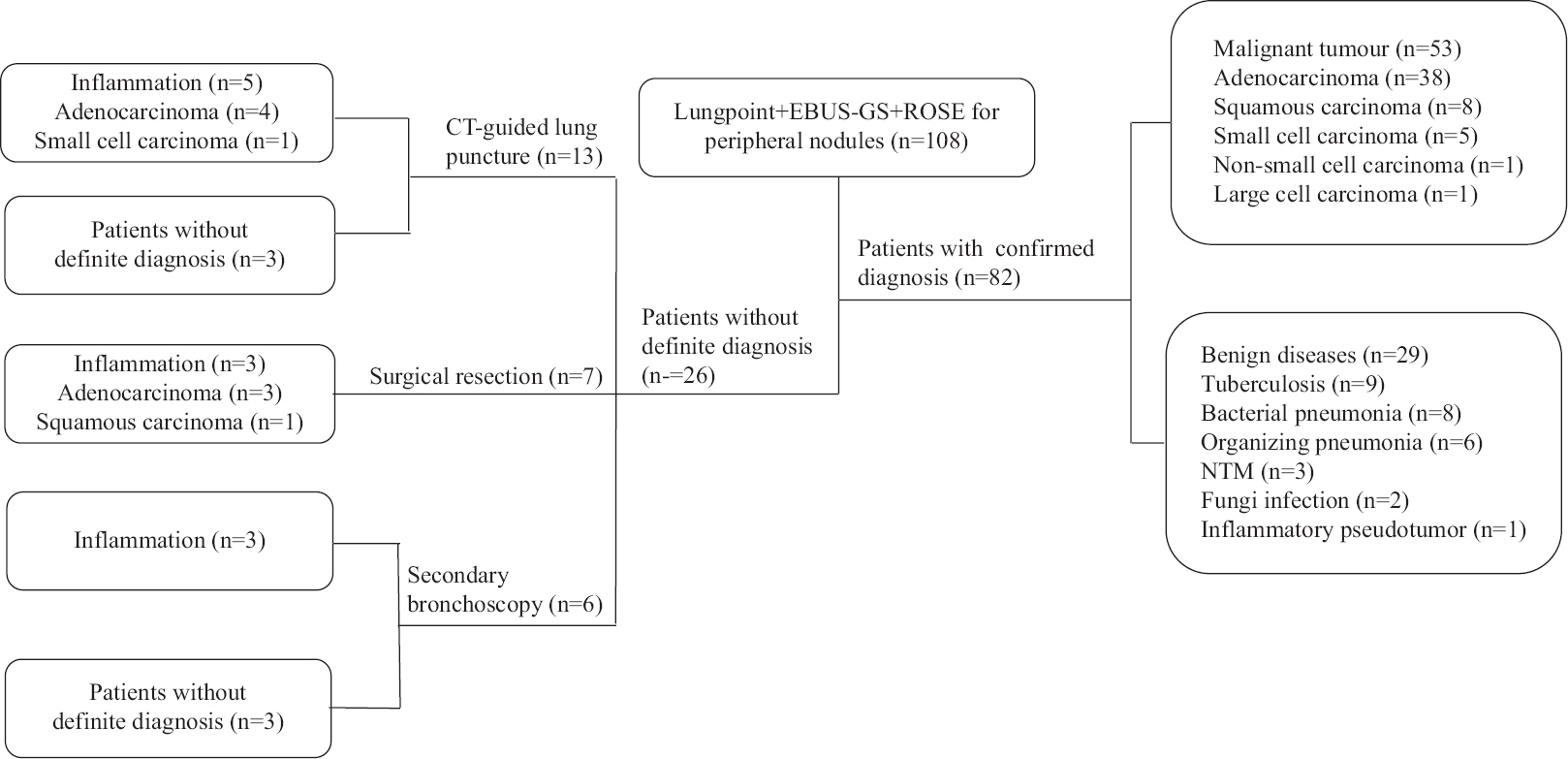
- Schematic diagram of the diagnoses of the study participants. Patients without definitive diagnosis were followed up for one year. NTM, non-tuberculous mycobacteriosis; CT, computed tomography; EBUS-GS, endobronchial ultrasound with a guide sheath; ROSE, rapid on-site evaluation.
Table I shows the clinical data of the study participants, with a mean age of 65.2±12.5 yr. The proportion of male participants two times higher than the female patients; the median size of the nodules was 23.8 mm, and the median of distance between the centre of the nodules and the pleura was 32.5 mm. The number of participants with nodules located in the upper, middle and lower lobe were 59, 9 and 40, respectively, which indicated that most of the lesions were located in the upper lobe. The median operative time for combined LungPoint+EBUS-GS+ROSE was 25.0 min, including the time required for planning the approach toward the lesion and EBUS-GS examination. Samples were taken from each area for 5-8 times, or alternatively, ROSE was performed to get the diagnosis.
| Characteristic | Data, n (%) |
|---|---|
| Age (yr; mean±SD) | 65.2±12.5 |
| Sex | |
| Male | 74 (68.5) |
| Female | 34 (31.5) |
| Smoking | |
| Yes | 68 (31.5) |
| No | 40 (37.0) |
| Nodule size (mm)§ | 23.8 (8-30) |
| The distance from the center of the nodule to the pleura (mm)§ | 32.5 (12.5-43.6) |
| Location of nodules | |
| The right upper lobe | 30 (27.8) |
| The middle lobe | 9 (8.33) |
| The right lower lobe | 19 (17.6) |
| The left upper lobe | 25 (23.1) |
| The left lung ligule | 4 (3.7) |
| Left lower lobe | 21 (19.4) |
| Operation time (min)§ | 25.0 (15.2-42.2) |
§Data presented in median (range). SD, standard deviation
Further subgroup analysis was performed according to the size of the nodules, the position in relation to the ultrasonic probe, the nature of the nodules (solid or ground-glass nodules) and their distance from the pleura (Table II). The positive rate of the ultrasonic probe was 91.9 per cent inside the nodules, 62.2 per cent near the nodules and 22.2 per cent outside the nodules. Among the 108 study participants, 85 had solid nodules, of 71 whom had a definitive diagnosis (diagnostic rate: 83.5%). There were 23 participants with ground-glass nodules, of these 11 had a definitive diagnosis (diagnostic rate: 47.8%), indicating that the positive rate for diagnosing solid nodules was higher than that of ground-glass opacities. The number of patients with nodules of 10-20 mm or 20-30 mm in diameter was 42 and 56, respectively, and their corresponding positive rate was 65.3 and 85.7 per cent. It was this concluded that the larger the nodules, the higher the positive rate. The nodular distance from the pleura >40, 20-40 and <20 mm were 13, 60 and 35 mm, respectively, and the corresponding numbers of participants with a clear diagnosis were 11, 49 and 22, respectively.
| Contribution of clinical factors available before bronchoscopy to diagnostic rate | Diagnostic rate, % (n/N) |
|---|---|
| The total mean diagnostic rate | 75.9 (82/108) |
| The position of probe with the nodule | |
| Within | 91.9 (57/62) |
| Adjacent to | 62.2 (23/37) |
| Not visualized | 22.2 (2/9) |
| Feature | |
| Solid nodule | 83.5 (71/85) |
| GGO | 47.8 (11/23) |
| Lesion size (mm) | |
| 10-20 | 65.3 (34/52) |
| 20-30 | 85.7 (48/56) |
| Distance from pleura (mm) | |
| <20 | 62.9 (22/35) |
| 20-40 | 81.7 (49/60) |
| >40 | 84.6 (11/13) |
| Final diagnosis | |
| Malignant | 85.5 (53/62) |
| Benign | 72.5 (29/40) |
| Following up | 5.6 (6/108) |
| Compliant | |
| Bleeding | 12.0 (13/108) |
| Pneumothorax | 4.6 (5/108) |
GGO, ground-glass opacity
Using LungPoint, EBUS-GS and ROSE in combination, 82 patients were definitively diagnosed with a diagnostic rate of 75.9 per cent. A total of 13 patients had a small amount of intraoperative bleeding, which was treated with suction and local haemostatic drugs. Furthermore, a small pneumothorax occurred in five patients without the need for a drainage-tube treatment; these patients recovered spontaneously.
Table III shows that the results between combined LungPoint, EBUS-GS and ROSE diagnostic and the pathological methods had a high degree of consistency [kappa=0.83, 95% confidence interval (CI), 0.65-1.00]. The diagnostic sensitivity, specificity, PPV and NPV were 85.5 per cent (95% CI, 76.7-94.3%), 100 per cent (95% CI, 100-100%), 100 per cent (95% CI, 100-100%) and 83.6 per cent (95% CI, 73.9-93.4%), respectively. Table IV shows that the results from ROSE and the final pathological results had a good degree of consistency (kappa=0.69, 95% CI, 0.51-0.88). The diagnostic sensitivity, specificity, PPV and NPV were 90.3 (95% CI, 83.0-97.7%), 78.3 (95% CI, 66.3-90.1%), 84.8 (95% CI, 76.2-93.5%) and 83.6 per cent (95% CI, 75.1-96.3%), respectively.
| Diagnosis of LungPoint + EBUS-GS + ROSE | Final diagnosis malignant | Final diagnosis benign | Total |
|---|---|---|---|
| Malignant | 53 | 0 | 53 |
| Benign | 9 | 46 | 55 |
| Total | 62 | 46 | 108 |
The sensitivity: 85.5 per cent (95% CI, 76.7-94.3%); Specificity: 100 per cent (95% CI, 100-100%); Positive predictive value: 100 per cent (95% CI, 100-100%); Negative predictive value: 83.6 per cent (95% CI, 73.9-93.4%); Kappa=0.83 (95% CI, 0.65-1.00); Accuracy rate: 91.7 per cent. EBUS-GS, endobronchial ultrasound with a guide sheath; ROSE, rapid on-site evaluation; CI, confidence interval
| ROSE | The final diagnosis malignant | The final diagnosis benign | Total |
|---|---|---|---|
| Malignant | 56 | 10 | 66 |
| Benign | 6 | 36 | 42 |
| Total | 62 | 46 | 108 |
The sensitivity: 90.3 per cent (95% CI, 83.0-97.7%); Specificity: 78.3 per cent (95% CI, 66.3-90.1%); Positive predictive value: 84.8 per cent (95% CI, 76.2-93.5%); Negative predictive value: 83.6 per cent (95% CI, 75.1-96.3%); Kappa=0.69 per cent (95% CI, 0.51-0.88); Accuracy rate: 85.2 per cent
Discussion
EBUS-GS is widely used in the diagnosis of pulmonary nodules. For lung evaluations, a 20 MHz ultrasonic probe is commonly used and displays the fine structure of pulmonary nodules. EBUS-GS in conjunction with LungPoint is considered as one of great significance in the diagnosis of peripheral pulmonary nodules. In 2010, Eberhardt et al6 reported on augmented reality navigation (LungPoint) for the diagnosis of peripheral pulmonary nodules. The greatest advantage of LungPoint VBN technology is that the approach incorporated the matched virtual image by using the endoscopic examination to guide the endoscopy towards the location of the lesion in relative real time. The results of this report showed that 20 of the 25 patients were diagnosed by LungPoint (the detection rate: 80%). Although the sample size is less, it is worth noting that the mean planning time was five minutes, the mean examination time was 15 min, and ultimately, the mean total time was 23 min. These findings were consistent with the results from a Japanese study, which reported that the positive diagnostic rate was 77.9 per cent for peripheral pulmonary nodules by using LungPoint navigation technology combined with EBUS-GS8. In an article in 2019, scholars analyzed the positivity rate of EBUS-GS alone and in combination with LungPoint navigation in the diagnosis rate of peripheral pulmonary nodules, the positivity rate of complications and the duration of diagnosis. The positivity rate of EBUS-GS group was similar to that of EBUS-GS combined with LungPoint (72.3 and 74.3%, respectively). In terms of duration of diagnosis, the results suggested that LungPoint can effectively shorten the time of planning the approach (7.96 vs. 11.92 min) but has little effect on the operation time (28.34 and 29.06 min, respectively). Although LungPoint VBN cannot further improve the diagnostic sensitivity of EBUS-GS, it can guide the operator to reach the target bronchus faster and more accurately, thus reducing the pain of patients, shortening the examination time and without the use of X-ray positioning. In this study, a total of 108 participants with pulmonary nodules were evaluated using combined LungPoint, EBUS-GS and ROSE technologies, and 82 patients were diagnosed clearly, with a positivity rate of 75.9 per cent. These findings are similar to the positive diagnosis rate of LungPoint combined with EBUS as reported earlier.
The ROSE technology uses the principle of cell pathology to deal with the biopsy samples (needle aspiration biopsy, clamp biopsy specimens, etc.) into pathological specimens to determine the nature of lesions after observation under the microscope9. The most important feature is that it takes no more than two minutes from the preparation to the reading of the film so that the degree of the specimen and the type of the lesion can be determined quickly in the midst of a procedure such as transbronchial biopsy. ROSE is widely used for tissue diagnosis during tracheoscopy procedures because of its simplicity, rapidity and real-time evaluation of the samples6, especially for the diagnosis of peripheral nodules. In our study, the combined use of EBUS-GS, LungPoint and ROSE technologies resulted in an average operation time of 20.5±18.5 min (including the time for planning lesion approach and EBUS-GS examination). Compared with the report in 20197 mentioned above, the combined use of the three technologies effectively shortened the diagnosis duration.
The diagnostic sensitivity of LungPoint combined with EBUS-GS and ROSE was comparable to other methods in the diagnosis of peripheral nodules. However, in terms of the incidence and severity of the complications, the combination of the three techniques may reduce the incidence of complications and reduce the symptoms. Only 12 participants out of 108 had a small amount of bleeding, which stopped after local administration of chilled saline and haemostatic drugs, and five participants had a small amount of bleeding due to pneumothorax. All pneumothoraxes were small and resolved spontaneously without the need for chest tube placement. Therefore, LungPoint combined with EBUS-GS and ROSE is a relatively safe technique for the diagnosis of pulmonary nodules. Compared with the report in 2019, there were no patients who needed interventional treatment for pneumothorax or haemorrhage. The reason of insufficient sample size was not ruled out, and further research is needed.
All patients in this study underwent ROSE, and its sensitivity, specificity, PPV and NPV were 90.3, 78.3, 84.8 and 83.6 per cent, respectively, compared with the final pathological results. The findings of this study suggest that ROSE had a high sensitivity in the diagnosis of malignant tumours, but there were also false negatives in some cases, which need to be further confirmed in a larger sample of randomized controlled studies.
Overall, this retrospective study suggests that the diagnostic duration of LungPoint combined with EBUS-GS and ROSE was shorter than that of LungPoint combined with EBUS-GS. Their diagnostic accuracy is similar, but the combination of the three techniques may improve the safety of diagnosis.
Financial support & sponsorship: The study was funded by The Medical Science and Technology Foundation of Henan Province (201602240 and 2018020404) and The Science and Technology Foundation of Henan Province (20161430).
Conflicts of Interest: None.
References
- Diagnostic feasibility and safety of CT-guided core biopsy for lung nodules less than or equal to 8 mm:A single-institution experience. Eur Radiol. 2018;28:796-806.
- [Google Scholar]
- CT-guided localization of small pulmonary nodules using adjacent microcoil implantation prior to video-assisted thoracoscopic surgical resection. Eur Radiol. 2015;25:2627-33.
- [Google Scholar]
- Radial endobronchial ultrasound for the diagnosis of peripheral pulmonary lesions:A systematic review and meta-analysis. Respirology. 2017;22:443-53.
- [Google Scholar]
- Electromagnetic navigational bronchoscopy versus CT-guided percutaneous sampling of peripheral indeterminate pulmonary nodules: A cohort study. Radiology. 2018;286:1052-61.
- [Google Scholar]
- An update on the role of advanced diagnostic bronchoscopy in the evaluation and staging of lung cancer. Ther Adv Respir Dis. 2017;11:211-21.
- [Google Scholar]
- Rapid on-site cytologic evaluation during endobronchial ultrasound-guided transbronchial needle aspiration for diagnosing lung cancer A randomized study. Respiration. 2013;85:486-92.
- [Google Scholar]
- Diagnostic yield of combined bronchoscopy and endobronchial ultrasonography, under LungPoint guidance for small peripheral pulmonary lesions. Respirology. 2013;18:834-9.
- [Google Scholar]
- Impact of rapid on-site cytologic evaluation during transbronchial needle aspiration. Chest. 2005;128:869-75.
- [Google Scholar]






