Translate this page into:
Avian influenza A H7N9 virus infections not evident among high-risk groups in India
*For correspondence: mscniv@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
An emergence of a novel avian-origin reassortant influenza A (H7N9) virus in Eastern China has caused an alarming situation due to severe lower respiratory tract infections in humans. As of January 2015, a total of 486 humans infections of H7N9 (resulting in 185 deaths) have been reported. Human infections of H7N9 virus have been associated with poultry exposures in live bird markets although H7N9 virus is not easily transmitted to humans1. In the scenario of emerging avian influenza (AI) viruses in Asia, it is necessary to monitor high-risk population groups such as poultry workers for human infections. In India, the outbreaks of highly pathogenic AI H5N1 virus were first reported in February 2006 in poultry at Navapur, Maharashtra, and then, several outbreaks have been reported in north-eastern India23. Considering the proximity of north-eastern regions of India with China and likelihood of introduction of this virus, the present study was conducted to detect AI H7N9 virus infections among poultry workers as a high-risk group in western and north-eastern India during 2014.
The surveillance of AI H7N9 virus infections among poultry workers working at live poultry markets and farms in Pune (Western India), West Bengal and Assam (north-eastern India) was planned and executed with the approval and support of the local Municipal and State Health Departments. The study was also approved by the Institutional Human Ethics Committee of the ICMR-National Institute of Virology at Pune, as per the guidelines laid down by the Indian Council of Medical Research for research on human subjects4. Written informed consent was obtained from individual study participants. The study participants were interviewed for pre-existing co-morbid diseases, health conditions or illnesses in the recent past (last six month), current or routine nature of work and any other work assignments of similar or related nature.
An assumption of <5 per cent antibody prevalence against AI H7N9 virus was made based on the similar studies performed outside India567. The sample size calculations were performed using online OpenEpi software8. The estimated sample size was 500 assuming 5 per cent prevalence, 95 per cent confidence and precision of 0.02 per cent by 2-sided test with finite population correction for population size of 5000 for the study area. Following this, the prospective clinical surveillance of acute respiratory illness (ARI) or influenza-like illness (ILI) was also undertaken in Pune and Assam among surveyed poultry workers9. The follow up of the poultry workers for any ARI/ILI episodes was carried out from January to July 2014.
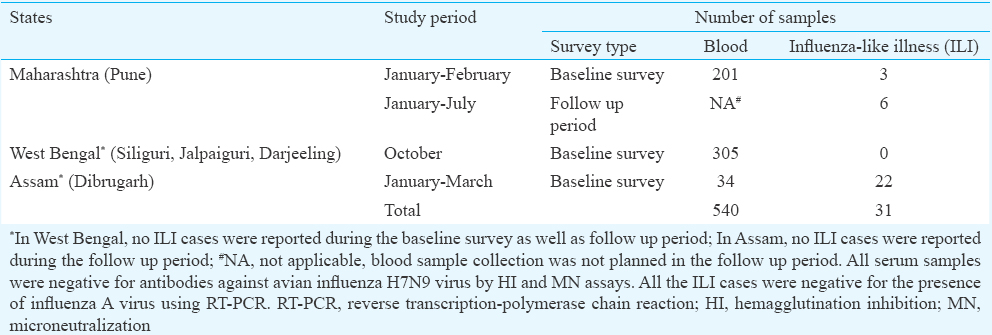
A total of 540 poultry workers were enrolled in the study during January to November 2014. The samples were collected from Pimpri-Chinchwad Municipal Corporation and Pune Municipal Corporation areas in Pune; Siliguri, Alipurduar, Dhupguri-Jalpaiguri, Kalimpong-Darjeeling, West Bengal and Dibrugarh, Assam. Blood samples (3-5 ml) were collected from 540 poultry workers by venipuncture, and serum was separated and stored at -20°C until tested (Table). The serum samples were tested by the hemagglutination inhibition (HI) and microneutralization (MN) assays as per the WHO recommended protocols for the detection of antibodies against H7N9 virus1011. HI assay was performed using 1 per cent horse red blood cells. The reference H7N9 virus A/Shanghai/2/13 (H7N9)-PR8, V-VIE2 ID-CDC-RG-32A from CDC, Atlanta, USA, was used in the study. A total of 31 throat and nasal swab samples were collected from individuals with ILI and tested for the presence of influenza A virus using real-time reverse transcription polymerase chain reaction (qRT-PCR) as per the protocol recommended by the CDC, USA12. RNase P and RNA from known positive sample served as positive controls. Nuclease-free water served as a negative control.
The poultry workers were individuals involved in handling, transport, cleaning and slaughter of poultry in live poultry markets, shops or farms. The age group of poultry workers ranged from 15-79 yr with the median of 30 yr (mean 32, standard deviation 11.86). The male to female ratio was 14. Only 6.5 per cent were females as poultry workers were predominantly males.
Clusters of severe ARI (SARI) or individual SARI cases were not reported. A total of 31 poultry workers reported ILI during the study; however, all samples were negative for the presence of influenza A virus by real-time RT-PCR. All serum samples were negative for the presence of antibodies against H7N9 virus by both HI and MN assays using ≥80 titre13. No symptomatic or asymptomatic H7N9 human infections were detected among occupational high-risk groups of poultry workers employed at live poultry markets and farms.
The findings of a seroepidemiological study on AI H5, H7 and H9 viruses have been reported by Xiong et al5 in the urban general population in China. The authors estimated the previous or transient asymptomatic and mild infections of AI viruses in the general population. HI assay was used for determining antibody levels in human serum samples. The study reported the absence of antibodies against H5N1 virus and low levels of antibodies to H7N9 virus. The earlier studies from China have shown low levels of antibodies to H5 and H7 viruses in high-risk groups67. Yin et al13 have reported lack of evidence of human infection with the H7N9 virus in veterinarians in China, using HA-specific ELISA and HI assays.
Our earlier study on retrospectively analyzed samples from poultry workers and general population in Pune has shown no evidence of H7N9 virus14. The present study has also confirmed the absence of exposure to H7N9 virus among the high-risk human populations in western and north-eastern India. The limitation of the present study was that the study was conducted over a limited period of time. Considering the ongoing transmission of H7N9 virus in Asia, it has been recommended to monitor and investigate clusters of SARI or individual cases of SARI among travellers from affected countries15. Strengths of the present study were inclusion of high-risk people by profession, clinical surveillance along with serological surveillance and employment of MN assays. The study population demographic characteristics were similar. However, the study group represented the higher risk of infections than the veterinarians because of work environment and practices of poultry workers.
In conclusion, an emergence of a novel avian-origin influenza A H7N9 virus in China has caused concern in the neighbouring countries. However, the limited surveillance of H7N9 virus conducted among poultry workers as a high-risk group in western and north-eastern India revealed the absence of H7N9 virus infections during 2014.
Acknowledgment
Authors thank Dr D.T. Mourya, Director, ICMR-National Institute of Virology, Pune, for support; Dr Ruben Donis, Influenza Division, CDC, Atlanta, USA, for providing H7N9 virus; Dr A.R. Deoshatawar, R.H. Jagtap, NIV, Pune; Drs Swarup Bakshi, Shweta Mandal, Rajheswar Singh, M.K. Golder, ARD Department for field work; Dr Biswa Ranjan Satpathi, Director, Dr Kamalakanti Pati, Jt. Director, Health Services and State Health Officials, Government of West Bengal; Health Officials, Pune, and Pimpri-Chichwad Municipal Corporation for permission and support. The study was partially funded by the Indian Council of Medical Research, Government of India and Supplemental Funding from CDC, Atlanta, USA, under the Cooperative Agreement No. 5U51IP000333CDC.
Conflicts of Interest: None.
References
- 2014. World Health Organization (WHO). WHO risk assessment human infections with avian influenza A (H7N9) virus. 02 October. Available from: http://www.who.int/influenza/human_animal_interface/influenza_h7n9/riskassessment_h7n9_2Oct14.pdf?ua=1
- Phylogenetic analysis revealed genetic similarity of the H5N1 avian influenza viruses isolated from HPAI outbreaks in chickens in Maharashtra, India with those isolated from swan in Italy and Iran in 2006. Curr Sci. 2006;91:77-81.
- [Google Scholar]
- Characterization of the influenza A H5N1 viruses of the 2008-2009 outbreaks in India reveals a third introduction and possible endemicity. PLoS One. 2009;4:e7846.
- [Google Scholar]
- 2006. Indian Council of Medical Research (ICMR). Ethical guidelines for biomedical research on human participants. October. Available from: http://www.icmr.nic.in/ethical_guidelines.pdf
- Serological study of antibodies to influenza A viruses among general population in Wuhan city China. J Clin Virol. 2014;61:178-9.
- [Google Scholar]
- Serologic study for influenza A (H7N9) among high-risk groups in China. N Engl J Med. 2013;368:2339-40.
- [Google Scholar]
- A serological survey of antibodies to H5, H7 and H9 avian influenza viruses amongst the duck-related workers in Beijing, China. PLoS One. 2012;7:e50770.
- [Google Scholar]
- 2014. Open Source Epidemiologic Statistics for Public Health (Open Epi). Available from: http://www.openepi.com/Menu/OE_Menu.htm
- 2014. World Health Organization. WHO surveillance case definitions for ILI and SARI. January. Available from: http://www.who.int/influenza/surveillance_monitoring/ili_sari_surveillance_case_definition/en
- 2002. World Health Organization. WHO manual on animal influenza diagnosis and surveillance. May. Available from: http://www.wpro.who.int/emerging_diseases/documents/docs/manualonanimalaidiagnosisandsurveillance.pdf
- Detection of antibody to avian influenza A (H5N1) virus in human serum by using a combination of serologic assays. J Clin Microbiol. 1999;37:937-43.
- [Google Scholar]
- 2009. World Health Organization. CDC protocol of real time RTPCR for influenza A (H1N1). 6 October. Available from: http://www.who.int/csr/resources/publications/swineflu/CDCReal-timeRT-PCR_SwineH1Assay-2009_20090430.pdf
- Antibodies against influenza A (H7N9) virus among veterinarians in China before 2013. Influenza Other Respir Viruses. 2015;9:38-9.
- [Google Scholar]
- Immunity status against influenza A subtype H7N9 and other avian influenza viruses in a high-risk group and the general population in India. J Infect Dis. 2014;210:160-1.
- [Google Scholar]
- 2013. World Health Organization (WHO). Interim WHO surveillance recommendations for human infection with avian influenza A (H7N9) virus. Available from: http://www.who.int/influenza/human_animal_interface/influenza_h7n9/InterimSurveillanceRecH7N9_10May13.pdf





