Translate this page into:
Prospective analysis of factors predicting feasibility & success of longitudinal intussusception vasoepididymostomy in men with idiopathic obstructive azoospermia
For correspondence: Dr Rajeev Kumar, Department of Urology, All India Institute of Medical Sciences, New Delhi 110 029, India e-mail: rajeev.urology@aiims.edu; rajeev02@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Microsurgical reconstruction for idiopathic obstructive azoospermia is a challenging procedure, and selection of appropriate patients is important for successful outcomes. This prospective study was done to evaluate the ability of scrotal ultrasound measurements to predict the surgical feasibility and determine factors that could predict a patent anastomosis following vaso-epididymal anastomosis (VE) in men with idiopathic obstructive azoospermia.
Methods:
In this prospective study, men diagnosed with idiopathic obstructive azoospermia, scheduled for a longitudinal intussusception VE, underwent a scrotal ultrasound measurement of testicular and epididymal dimensions. During surgery, site and type of anastomosis, presence of sperms in the epididymal fluid and technical satisfaction with the anastomosis were recorded. All men where VE could be performed were followed up for appearance of sperms in the ejaculate. Ultrasound parameters were compared between men who had a VE versus those with negative exploration. Predictive factors were compared between men with or without a patent anastomosis.
Results:
Thirty four patients were included in the study conducted between September 2014 and August 2016 and a VE was possible in only 19 (55%) patients. Of these 19 patients, six had a patent anastomosis with one pregnancy. Preoperative ultrasound measurements could not identify patients where a VE could not be performed. Motile sperm in the epididymal fluid was the only significant predictor of a successful anastomosis.
Interpretation & conclusion:
Forty five per cent of men planned for a VE for idiopathic obstructive azoospermia could not undergo a reconstruction. Ultrasound assessment of testicular and epididymal dimensions could not predict the feasibility of performing a VE. The presence of motile sperms in the epididymal fluid was the only significant predictor of a patent VE in our study.
Keywords
Azoospermia
idiopathic
infertility
obstruction
vasoepididymostomy
Azoospermia, defined as complete absence of sperms in the ejaculate, is present in less than one per cent of men and in 10-15 per cent of men with infertility1. About 40 per cent of men with azoospermia have an obstruction in the ductal system, at a point between the rete testis and the ejaculatory ducts2. While vasectomy is the most common cause of obstruction in regions where this is a favoured option for sterilization, the aetiology of obstruction is presumptive in over 80 per cent of patients in other regions34. Diagnosing obstructive azoospermia is clinically relevant as this is one of the surgically treatable causes of infertility, particularly with a vaso-epididymal anastomosis (VE) for a vaso-epididymal junction obstruction.
Surgery is usually successful only for discrete obstructions, and patients with diffuse obstruction within the epididymis, possibly due to an undiagnosed previous inflammation, cannot undergo a VE56. Genital inflammations, including those caused by filariasis and tuberculosis in endemic areas, often leave no diagnostic clinical signs or abnormal laboratory parameters, and a diagnosis of exclusion is made only on a negative surgical exploration for reconstruction67. While diagnosis and treating a burnt-out infection may not be necessary, identifying surrogate markers that could predict a reconstructable obstruction would be important in counselling patients and possibly reducing negative explorations.
One of the consequences of vasal obstruction is proximal tubular dilatation including that of the epididymis. Epididymal distension has been found to be associated with a diagnosis of obstructive azoospermia and a predictor of outcome following VE89. Ultrasound-based assessment of epididymal dimensions has previously been used as a predictor of obstructive azoospermia10. We hypothesized that discrete obstructions that could be reconstructed would lead to a dilated epididymis while inflammation involving the entire epididymis would prevent epididymal dilatation. The present study was, therefore, performed to evaluate the ability of an ultrasound examination to determine reconstructable obstructions. In addition, all parameters that could predict a successful outcome after a VE for idiopathic obstructive azoospermia were also evaluated.
Material & Methods
This prospective study was performed in the departments of Urology and Radiodiagnosis, All India Institute of Medical Sciences (AIIMS), New Delhi, India, with a dedicated male infertility clinic over a two-year period beginning September 2014. The study was approved by the institutional ethics committee. All patients provided written informed consent for inclusion in the study. Consecutive infertile men below 40 yr of age, diagnosed with idiopathic obstructive azoospermia, who opted to undergo scrotal exploration for possible VE, were invited for inclusion. All men had normal volume azoospermia confirmed on at least two semen analysis, at least one palpable vas deferens, normal testis volume (>15 ml by Prader orchidometer), normal serum follicle-stimulating hormone (FSH) levels (<10 mIU/ml) and normal spermatogenesis on testicular histology. Men with a history of vasectomy, inguinal or scrotal surgery, varicoceles, history of genital inflammations or other known causes of infertility were excluded.
Scrotal ultrasound: All individuals underwent a scrotal ultrasound using a 12 MHz, linear-array transducer; a grey scale sonogram was obtained in the transverse and longitudinal planes to evaluate the testicular volume and diameters of the caput and the corpus of the epididymis of each side. Bilateral testicular volume was calculated using the formula, length×breadth×depth×π/6, assuming that the testis is ellipsoid. Caput epididymis size (in mm) was measured on longitudinal plane where the caput appears pyramidal above the upper pole of testis.
Surgery: Scrotal exploration was performed under general anaesthesia as per our previously described technique1112. Briefly, the testis was exposed through a longitudinal scrotal incision; the vas deferens was isolated and divided at the junction of its convoluted and straight parts. Vasal patency was verified using saline irrigation and vasoepididymal junction obstruction was diagnosed if there was free flow of saline into the vas deferens, but no fluid or sperms were seen emanating from the proximal end. The epididymis was inspected under an operating microscope, beginning from the tail to the head, to identify the most appropriate site for anastomosis. The most distal site showing dilated tubules was preferred and recorded as cauda, body or caput, and the epididymis was subjectively graded as distended, normal or collapsed. The end of the vas was fixed to the epididymis using 8-0 nylon sutures. After placing the 10-0 nylon anastomotic sutures for a longitudinal, intussusception VE in the epididymal tubule, the tubule was incised and the fluid was inspected under a light microscope for sperms. Light microscopy findings were labelled as motile sperms, non-motile sperms or no sperms. The anastomosis was with a single tubule if the tubules were dilated and had fluid. If there was no fluid or the tubules appeared very small, the 10-0 nylon sutures were taken through multiple adjacent tubules and the incision was placed across all such tubules, which was termed a ’multi-tubule’ anastomosis. If the epididymis was completely cicatrized or totally flaccid, the procedure was abandoned. The surgeon's subjective satisfaction with the anastomosis was graded from 1 to 3 (3 being most satisfactory)13. All surgeries were unilateral.
Follow up: After surgery, patients who underwent an anastomosis were advised abstinence for six weeks and a semen analysis was performed at that time. Repeat analyses were performed at three months and every three months thereafter for one year or till the appearance of sperms in the ejaculate. If no anastomosis was performed, the patients were advised assisted reproduction.
Outcome measures: The appearance of sperms in the ejaculate after surgery was considered a patent anastomosis or successful surgery. Pre-operative ultrasound findings were assessed for their ability to predict the feasibility of performing a VE by comparing values between patients who had a VE versus those where surgery was not feasible. Subsequently, ultrasound, clinical and intraoperative findings were compared between patients who had successful surgery (patent anastomosis) versus those who failed. A per-protocol analysis was performed.
Statistical analysis: Student's t test, Fisher's exact test and Chi-square test were used for comparing groups using STATA® 14 (STATA Corporation Texas, USA) software.
Results
During the study, of the 37 eligible patients, 34 were included in the final analysis as two patients refused consent and one was found unfit for surgery. The mean age of patients was 30.1 yr (range 22-38 yr) with median period of infertility of four years (range 1-13 yr). The mean follow up period was 11±4 months in patients who underwent a VE. The mean FSH was 3.37±1.65 mIU/ml. VE was possible in only 19 (55.8%) of the 34 patients who underwent surgery while 15 procedures were abandoned; 73 per cent (11/15) of the patients in the negative exploration group were from a filariasis endemic zone. Table I lists the ultrasound findings in these two groups. The dimensions measured on ultrasound were similar in both groups, and none of the parameters was able to predict the ability to perform a VE.
| Parameter | Exploration only (n=15) | VE performed (n=19) |
|---|---|---|
| Right testis | ||
| Volume (ml) | 14.4±2.5 | 16.4±3.2 |
| Caput epididymis length (mm) | 9.5±2.6 | 9.8±1.4 |
| Corpus epididymis length (mm) | 2.6±0.6 | 2.6±0.4 |
| Left testis | ||
| Volume (ml) | 14.5±2.4 | 15.0±4.3 |
| Caput epididymis length (mm) | 8.8±1.5 | 9.6±1.8 |
| Corpus epididymis length (mm) | 2.6±0.6 | 2.7±0.6 |
Of the 19 patients where a VE was possible, six had successful (patent) anastomosis with appearance of sperms between three and six months after surgery and one pregnancy at four months after surgery. The presence of motile sperms in the epididymal fluid was the only factor that could predict a successful VE (Table II). All six men with a patent anastomosis had sperms on intraoperative examination of epididymal fluid, and this was significantly different from surgical failures (P<0.01). None of the patients with absence of sperms in the fluid had a successful VE.
| Parameter | Failure (n=13) | Success (n=6) |
|---|---|---|
| Mean age (yr, range) | 30.8 (22-38) | 31.0 (23-37) |
| FSH (mIU/ml, mean±SD) | 3.8±1.1 | 3.33±1.7 |
| Right testis | ||
| Volume (ml) | 15.0±1.2 | 17.1±3.6 |
| Caput epididymis length (mm) | 9.7±1.1 | 9.8±1.6 |
| Corpus epididymis length (mm) | 2.8±0.5 | 2.5±0.4 |
| Left testis | ||
| Volume (ml) | 14.0±1.7 | 15.5±5.1 |
| Caput epididymis length (mm) | 10.5±2.7 | 9.4±2.1 |
| Corpus epididymis length (mm) | 2.7±0.6 | 2.7±0.7 |
| Sperm motility in epididymal fluid†† | ||
| Motile spermatozoa | 1 | 5 |
| Non-motile spermatozoa | 5 | 1 |
| Absent spermatozoa | 7 | 0 |
| Epididymal distension on inspection | ||
| Distended | 4 | 2 |
| Normal | 9 | 4 |
| Collapsed | 0 | 0 |
| Site of anastomosis* | ||
| Caput epididymis | 11 | 2 |
| Corpus epididymis | 2 | 3 |
| Surgeon’s satisfaction with anastomosis | ||
| High (3/3) | 7 | 5 |
| Moderate (2/3) | 6 | 1 |
| Low (1/3) | 0 | 0 |
| Anastomosis technique | ||
| Single tubule | 8 | 5 |
| Multiple tubule | 5 | 1 |
††P<0.01 between the two groups. *Data not available for one patient in success group. FSH, follicle-stimulating hormone; SD, standard deviation
Of 19 anastomoses, 13 were at the head of the epididymis and none at the tail. During surgery, sub-tunical areas of a bluish hue at the head were often found, suggesting ruptured tubules underneath (Figure). A non-planned analysis of estimation of testicular size by Prader orchidometer versus ultrasound showed significant differences between the two modalities, with ultrasound showing significantly smaller volumes (right testis: 18.03±2.7 vs. 15.62±3.1 ml, P=0.001; left testis: 17.72±3.3 vs. 14.8±3.6 ml, P=0.001).
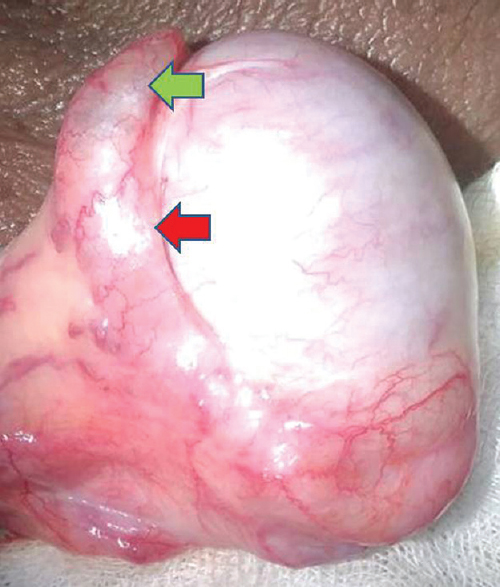
- Epididymis (×8) showing blue hue at the caput (green arrow) suggesting an underlying tubule rupture and flaccid body and tail (red arrow).
Discussion
Forty five per cent of patients planned for VE in this study had a negative exploration, and the procedure had to be abandoned. The primary objective of our study was to assess ultrasound as a predictor of such negative explorations, but it was found it to be non-contributory. In addition, it was found that motile sperms in the epididymal fluid were the only predictors of a successful anastomosis.
Thirty to seventy per cent of cases of obstructive azoospermia have obstruction at the epididymal level, and most of these are in the cauda with only 15 per cent being at the intratesticular level that precludes reconstruction214. If sperm production is normal and there is no intratesticular obstruction, the epididymis is expected to distend. In 12 patients of azoospermia, Kolettis8 found epididymal fullness in 33 per cent and physical examination could suggest obstruction with a 100 per cent positive and 83 per cent negative predictive values. He concluded that although a full epididymis was predictive of obstruction, a normal epididymis did not rule it out. These findings were supported by Peng et al9, who showed clinically distended epididymis as one of the predictors of success of VE. Pezzella et al10 used ultrasound-based measurement of the caput size to differentiate between obstructive and non-obstructive azoospermia and found the caput diameter to be significantly larger in obstructive azoospermia.
Our findings were contrary to these in that the ultrasound was found to have no predictive ability. This may be due to the aetiology of obstruction in our patients. While most existing data relate to post-vasectomy VE, all our patients had idiopathic obstruction. The cause of obstruction may affect the degree of epididymal dilatation. In vasectomy, the epididymis is not inflamed and hydrostatic pressure may cause dilatation proximal to the vasectomy site. In our patients, the aetiology of obstruction was previously undiagnosed inflammation. Filariasis and tuberculosis were important causes of infertility in our patients, a suspicion supported by the fact that the majority of these men were from an endemic zone5715. These conditions often have minimal symptoms at the time of infection and are rarely diagnosed in retrospect5. However, inflammation caused by these can involve the entire epididymis, preventing its dilatation. This assumption was supported by the fact that none of our anastomosis was made at the tail of the epididymis, the favoured site for a VE as it has the most dilated tubules9. Two-thirds were at the caput-epididymis, the least favoured site with the smallest tubules, because that was the only site where tubules were distinct. Inflammatory adhesions replacing the entire epididymis was also seen in many cases. Perhaps in these patients, the entire epididymis was obstructed and a few islands that escaped cicatrization were used for an anastomosis. Because these small islands cannot be identified on the ultrasound, the findings would be similar in both groups.
Among factors that could predict success, only the presence of motile sperms was found to be significant. It is expected that a patent anastomosis would depend on the presence of sperms at the site proximal to the anastomosis, distal patency and a technically sound anastomotic technique. In our patients, while the other two parameters were constant, it was the presence of sperms that determined success. This finding was consistent with an earlier report10. However, contrary to that report, surgeon's satisfaction did not impact outcomes.
Our patency rate of 31.5 per cent (6/19) was similar to previous data, including our own, on idiopathic obstructions but lower than those for post-vasectomy VEs912141617. The success rate was 50 per cent (6/12) if patients in whom sperms were not present in epididymal fluid were excluded because none of the seven patients with absent sperms were successful. Another reason for lower patency rate in the present study could be the unilateral anastomosis which has poorer success rate in comparison to bilateral VE91216. The unilateral surgery was performed to preserve the contralateral side for a percutaneous epididymal sperm aspiration if required for in vitro fertilization.
The site of anastomosis may also impact the surgical outcomes. While Kim et al18 reported 100 per cent patency rate after anastomosis at the head of epididymis and 73 per cent patency after anastomosis at body, Zhang et al19 reported low success rate after anastomosis at the head (62.2%) in comparison to body (72.2%) in bilateral VE. Although the data are variable, most studies show higher pregnancy rate after distal anastomosis181920. The majority of our surgeries were performed at the head of the epididymis, potentially impacting the outcomes. In a non-planned analysis, the testicular volume measured by the Prader orchidometer was found to be different from that measured by the ultrasound. Similar discrepancies have been previously reported21. This may be related to the formulae or techniques used for the ultrasound measurements.
Our study had several limitations. Most important was the lack of aetiological diagnosis for the obstruction. It was not possible to determine any method of diagnosing inflammatory causes that might have occurred many years ago in the past. An epididymal biopsy might have confirmed inflammatory changes or fibrosis but that was unlikely to impact diagnosis or management. The number of cases studied was small and predictive factors could have become significant with larger sample size.
In conclusion, nearly half of all patients planned for a VE for idiopathic obstructive azoospermia were found to be unsuitable for reconstruction. Ultrasound measurements of the testis and epididymis could not identify patients likely to fail. Among patients who underwent VE, the finding of motile sperm in the epididymis at the site of anastomosis was the most important predictor of a successful outcome. Further study with a large sample size needs to be performed to confirm these findings.
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- Microsurgical repair of iatrogenic injury to the vas deferens. J Urol. 1998;159:139-41.
- [Google Scholar]
- Surgery for azoospermia in the Indian patient: Why is it different? Indian J Urol. 2011;27:98-101.
- [Google Scholar]
- Reproductive tract tuberculosis and male infertility. Indian J Urol. 2008;24:392-5.
- [Google Scholar]
- Genital tuberculosis in Indian infertility patients. Int J Gynaecol Obstet. 2007;97:135-8.
- [Google Scholar]
- Filarial orchitis: A cause of male infertility in the tropics – Case report from Nigeria. Cent Afr J Med. 1989;35:456-60.
- [Google Scholar]
- Is physical examination useful in predicting epididymal obstruction? Urology. 2001;57:1138-40.
- [Google Scholar]
- Patency rates of microsurgical vasoepididymostomy for patients with idiopathic obstructive azoospermia: A prospective analysis of factors associated with patency - Single-center experience. Urology. 2012;79:119-22.
- [Google Scholar]
- Ultrasonographic determination of caput epididymis diameter is strongly predictive of obstruction in the genital tract in azoospermic men with normal serum FSH. Andrology. 2013;1:133-8.
- [Google Scholar]
- Intussusception vasoepididymostomy with longitudinal suture placement for idiopathic obstructive azoospermia. J Urol. 2010;183:1489-92.
- [Google Scholar]
- Early patency rates after the two-suture invagination technique of vaso-epididymal anastomosis for idiopathic obstruction. BJU Int. 2006;97:575-7.
- [Google Scholar]
- Predictors of patency after two-stitch invagination vaso-epididymal anastomosis for idiopathic obstructive azoospermia. Indian J Urol. 2005;21:112-5.
- [Google Scholar]
- Causes of suspected epididymal obstruction in Chinese men. Urology. 2012;80:1258-61.
- [Google Scholar]
- Lymphatic filariasis in India: Epidemiology and control measures. J Postgrad Med. 2010;56:232-8.
- [Google Scholar]
- Contemporary outcomes of seminal tract re-anastomoses for obstructive azoospermia: A Nationwide Japanese Survey. Int J Urol. 2015;22:213-8.
- [Google Scholar]
- Vasoepididymostomy for vasectomy reversal: A critical assessment in the era of intracytoplasmic sperm injection. J Urol. 1997;158:467-70.
- [Google Scholar]
- Pathological epididymal obstruction unrelated to vasectomy: Results with microsurgical reconstruction. J Urol. 1998;160:2078-80.
- [Google Scholar]
- Microsurgical treatment of obstructive azoospermia: A report of 76 cases. Zhonghua Nan Ke Xue. 2015;21:239-44.
- [Google Scholar]
- Prospective analysis of outcomes after microsurgical intussusception vasoepididymostomy. BJU Int. 2005;96:598-601.
- [Google Scholar]
- Testicular volume: Comparison of orchidometer and US measurements in dogs. Radiology. 2002;222:114-9.
- [Google Scholar]






