Translate this page into:
Sexual dysfunctions in alcohol-dependent men: A study from north India
Reprint requests: Dr Sandeep Grover, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh 160 012, India e-mail: drsandeepg2002@yahoo.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution NonCommercial ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Sexual dysfunctions have been reported in alcohol-dependent men. Most of the studies conducted had limitation of using non-validated measures of sexual dysfunction and sampling design. This study was, therefore, conducted to determine the typology, demographic and clinical correlates of sexual dysfunction in alcohol-dependent men.
Methods:
One hundred and one patients with alcohol dependence (AD) attending the Drug De-addiction and Treatment Centre and 50 healthy controls were evaluated in this cross-sectional study. Participants in both the groups were assessed on Arizona Sexual experience scale (ASEX), Dyadic Adjustment Scale (DAS), Hamilton Depression Rating Scale (HDRS) and State-Trait Anxiety Inventory (STAI). In addition, patients with AD were assessed on Severity of Alcohol Dependence Questionnaire (SADQ) for severity of AD and revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar) to ensure that no participant was in active alcohol withdrawal state.
Results:
Overall, 58.4 per cent of patients in the AD group had sexual dysfunction. Among the domains, the highest frequency was seen for dysfunction for arousal (57.4%), followed by problems in desire (54.4%), erection (36.6%), satisfaction with orgasm (34.6%) and ability to reach orgasm was least affected (12.87%). The patient and control groups differed significantly in overall dyadic adjustment, in the domains of dyadic satisfaction and affective expression.
Interpretation & conclusions:
The finding of this study showed that a significant proportion of patients with AD has sexual dysfunction. Longitudinal studies using validated assessment tools should be done to confirm these findings.
Keywords
Alcohol dependence
dyadic adjustment
men
sexual dysfunction
Alcohol abuse/dependence is known to lead to sexual dysfunction1. In clinical populations, the relationship between alcohol and sexual dysfunction has been studied from the following points of view: prevalence and correlates of sexual dysfunction in patients seeking treatment for alcohol problems, prevalence of alcohol use/abuse/dependence in patients seeking treatment for sexual dysfunction and effect of alcohol on various mechanisms involved in sexual functioning. Sexual dysfunction has been reported in 40-95.2 per cent of alcohol-dependent patients, the rates being consistently higher than in the healthy controls or social drinkers1. The common sexual dysfunctions reported are erectile dysfunction, followed by premature ejaculation, retarded ejaculation and decreased sexual desire among men and dyspareunia and vaginal dryness among women1. A review of clinical and experimental studies concluded that in male alcoholics, greater quantity, frequency and duration of drinking were associated with erectile dysfunction, inhibited libido and retarded ejaculation2. Another consistent correlate of sexual dysfunction reported in alcohol-dependent patients is advancing age1. However, a major limitation of these data has been the lack of usage of standard instruments to assess sexual dysfunction. Some investigators345 have used standard scales such as International Index of Erectile Function (IIEF), of which two used the full form of IIEF to assess sexual dysfunction.
Some of the studies have refuted the link between sexual dysfunction and alcohol678. A meta-analysis of population-based cross-sectional studies to assess the association of alcohol consumption and erectile dysfunction yielded a protective association of alcohol on ED9. Other studies have reported a variable percentage of alcohol use in patients presenting with sexual dysfunction1011.
One of the major limitations of the existing data is the way in which sexual dysfunction has been assessed. In some studies sexual dysfunction has been assessed using spontaneous reporting or open questions which may be interpreted differently by different patients, and hence the findings may not be reliable. Others have used inconsistent and non-validated measures of sexual dysfunction. Further, some investigators have taken mixed groups of patients (i.e., single and married patients) or have not evaluated for other contextual factors which could contribute to sexual dysfunction. Most of the studies lack matched controls. Thus, the present study was aimed to assess the typology, demographic and clinical correlates of sexual dysfunction in alcohol-dependent men.
Material & Methods
The study was carried out during July 2011 to June 2012 at the Drug De-addiction and Treatment Centre (DDTC) of the Department of Psychiatry at the Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India. The study protocol was approved by the institutional ethical committee, and all the participants were recruited after obtaining a written informed consent.
A cross-sectional design was used. The patients were assessed only once at the time of intake into the study. The study sample consisted of two groups of men: those with AD as per Diagnostic and Statistical Manual of Mental Disorders-4th Edition (DSM-IV) [confirmed by a structured Mini International Neuropsychiatric Interview (MINI12)] for at least one year (AD group, n = 101) and healthy controls, i.e., those not dependent on any substance except tobacco (HC group, n = 50).
Instruments: MINI12 is a brief structured interview for diagnosis of psychiatric disorders. It was used to confirm the diagnosis of AD and to rule out psychiatric comorbidities and other substance dependence/abuse. Revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar)13 was used to quantify the severity of the alcohol withdrawal syndrome. Arizona Sexual Experience Scale (ASEX)14 is a five-item self-report inventory using a six-point Likert scale method. It evaluates sexual function in men and women, regardless of sexual orientation or relationship with a partner. It measures the quality of functioning in terms of five questions, each representing one domain: drive, arousal, penile erection/vaginal lubrication, ability to reach orgasm and satisfaction from orgasm. These were selected as the domains because these were consistent with domains of sexual function described in the DSM-IV, International Classification of Diseases-10 (ICD-10)15 and currently used inventories of sexual function. ASEX is interpreted based on a total score and/or assessment of scores on individual items with lower scores indicating better sexual functioning. A total score >19 on ASEX or a score >5 on any one item or a score >4 on any three items is associated with clinical sexual dysfunction. Reliability coefficients for internal consistency and test-retest forms are excellent, and initial favourable test results of concurrent, convergent and discriminative validity have been reported. The sensitivity of ASEX was found to be 80.8 per cent and specificity as 88.1 per cent16. In the current study, a Hindi translated version of ASEX was used.
Dyadic Adjustment Scale (DAS)17 is a self-administered scale for measuring the marital adjustment. It has 32 items with four empirically verified components: dyadic consensus, dyadic cohesion, affectional expression and dyadic satisfaction. Dyadic consensus refers to the degree of making major decisions. Dyadic cohesion refers to how often a couple engages in companionate activities. Affectional expression concerns how often a couple expresses love for each other. Dyadic satisfaction examines the degree of happiness in the relationship, plus the frequency of the conflicts experienced in the relationship. The scale has a scoring of 0-5 for most of the items except for items number 23 and 24 (0-4); item number 29 and 30 (0-1) and item number 31 (0-6), with a higher score, indicating better adjustment. It has high reliability and validity. This study used the Hindi translated version18, which has been used in a previous study from our centre.
Hamilton Depression Rating Scale (HDRS)19 is a clinician-rated scale, with 17-item version being the most commonly used. Items are rated from 0 to 4 or 0 to 2, according to intensity and frequency of symptoms in the past one week. It is a valid instrument with an intraclass correlation coefficient of 0.86, indicating adequate interobserver agreement. This was used to evaluate any subsyndromal depressive symptoms.
State-Trait Anxiety Inventory (STAI)20 provides reliable, relatively brief, self-report measure of state (A-state) and trait (A-trait) anxiety20. A standardized Hindi translation was used21. Section A-state consists of 20 statements on how people feel at a particular moment in time and section A-Trait consists of 20 statements on how people feel generally. The items are rated on a four-point Likert scale. The scale measures the individual differences in anxiety proneness, their disposition to respond to stress with a difference of A-state. The internal consistency and reliability of the STAI A-trait and A-state scales are high. The test-retest reliability of STAI A-trait scale suggests that it is stable over time, whereas scores on the STAI A-state scale increase as a function of stress and decrease in response to relaxation training.
Severity of AD Questionnaire (SADQ)22 consists of 20 questions to measure the severity of AD. With four items in each, there are five subscales: physical withdrawal, affective withdrawal, withdrawal relief drinking, alcohol consumption and rapidity of reinstatement. The maximum score is 60 and scores greater than 30 correlates with the clinician's rating of severe AD. The test-retest reliability is 0.85 and content, criterion and constructs validity are well established.
Intake procedure: The AD men were recruited from the inpatients or outpatients attending the DDTC if they met the specified inclusion and exclusion criteria. One of the inclusion criteria was at least one week of abstinence from alcohol, which was confirmed from the relatives as well. Furthermore, the inclusion into the study was determined by purposive random sampling i.e., 50 per cent of the eligible patients were included into the study using a predetermined randomization table.
The HC participants were non-blood related caregivers/visitors of patients attending the PGIMER, who were not more than twice a week users of psychoactive substances except tobacco. This history was obtained from the participants and confirmed by one of their relatives.
The inclusion criteria (for either group) were men aged 21-50 yr who were married or having a stable heterosexual sexual partner. Patients with AD who had acute intoxication or were in an acute withdrawal state were excluded from the study. Those with a chronic comorbid medical illness which can cause sexual dysfunction [hypertension, diabetes mellitus, thyroid dysfunction, cardiovascular disorders (angina and myocardial infarction), renal dysfunctions and neurological disorders (stroke, spinal cord lesions and peripheral neuropathy)] were also excluded from the study. The medical illnesses were ruled out by the history, physical examination and investigations. Further, those with a history of sexual dysfunction before the onset of substance use (confirmed by retrospective application of IIEF), history of trauma or surgery in the pelvic area, organic brain syndrome, intellectual disability and co-morbid axis-1 psychiatric disorders (as per MINI)12 were also excluded. Those using any substance regularly except for nicotine and those taking benzodiazepines, naltrexone, acamprosate, baclofen or disulfiram continuously for more than two weeks before the assessment for the study were also excluded. Those regularly using any medication which could improve/decrease the desire or the level of sexual functioning (e.g., phosphodiesterase inhibitors) were not considered for the study.
Both groups were assessed on MINI, ASEX, DAS, HDRS and STAI. AD group was also assessed on SADQ, DAS and CIWA-Ar.
Statistical analysis: Data were analyzed using SPSS 14 (SPSS for Windows, Version 14.0. SPSS Inc. Chicago, USA). Frequency and percentages were calculated for the categorical variables and mean and standard deviation (SD) were determined for the continuous variable. Comparisons were done using Chi-square test, t test, Mann–Whitney U-test and Fisher's exact test.
Results
For this study, 222 patients diagnosed with AD were approached by convenient sampling method to participate in the study. Of these patients, two refused to participate and 20 were excluded by the use of MINI; the reasons for exclusion being use of illicit substance along with alcohol independent pattern of other substances (n = 15), presence of other axis-I psychiatric diagnosis [psychosis NOS, generalized anxiety disorder and bipolar affective disorder (n = 1 each)] and not having constant sexual partner/divorced and age more than 50 yr (n = 1 each). Of the remaining 200 patients, based on the randomization number table drawn before the beginning of recruitment of patients, 101 patients were selected, who formed the study sample.
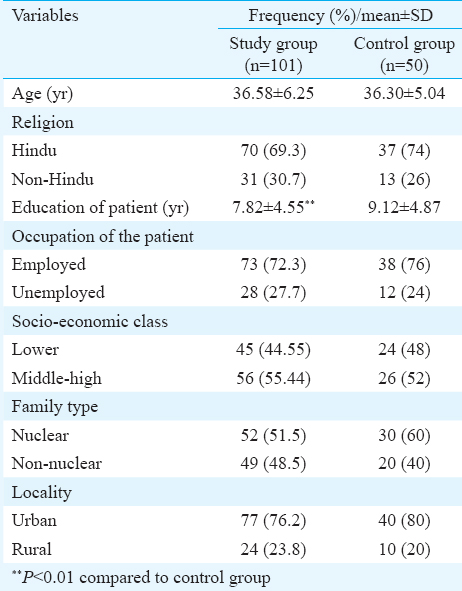
The sociodemographic profiles of the AD group and healthy control group are shown in Table I. The two groups had a similar sociodemographic profile except that the AD group was significantly less educated.
Clinical profile of the AD group: The mean age at onset of alcohol use in the study group was 24.2 ± 3.7 years. At the time of assessment, the mean duration of alcohol use was 12.35 ± 6.26 years and the duration of AD was 8.65 ± 5.01 years. The mean amount of alcohol consumed before the current abstinence was 516 ± 351.6 ml/day, with slightly more than one-third (37.6%) of the patients reporting consuming more than 360 ml/day. All the patients were consuming Indian-made foreign liquor (IMFL), with 43 also consuming country-made liquor (volume/volume alcohol content of both 42.7%). At the time of assessment, the mean duration of abstinence was 9.69 ± 3 days; the CIWA-Ar mean score was 3.52 ± 1.41, with all the cases scoring less than seven and SADQ mean score was 23.43 ± 3.39, and three patients had an SADQ score of more than 30 indicating severe AD. Majority of the patients (n = 85) were using tobacco along with alcohol: the most common mode being chewable form (n = 43), followed by both in chewable and smoking forms (n = 23) and smoking form only (n = 19). Very few patients (n = 8) had a comorbid personality disorder (dissocial - 6, anxious avoidant - 2).
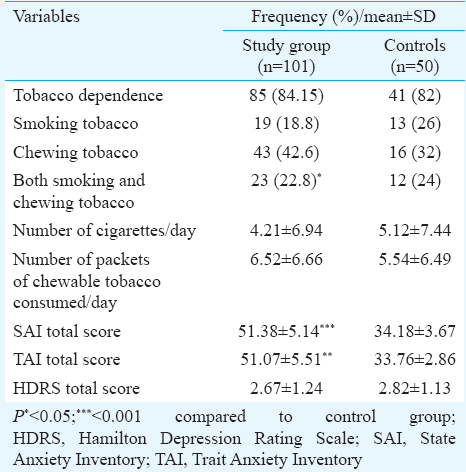
Comparison of tobacco use profile of the two groups revealed no significant difference for the presence of tobacco use, type of tobacco used and the amount of tobacco used per day except for slightly more tobacco dependence in the study group. Compared to the healthy controls, the alcohol-dependent group had a higher level of state and trait anxiety; however, the two groups did not differ in the level of depression as assessed by the HDRS (Table II).
Sexual dysfunction and dyadic adjustment: ASEX defined sexual dysfunction was seen in 58.4 per cent patients in the AD group. With a cut-off score of four used to define sexual dysfunction, among the domains, the highest frequency was seen for dysfunction for arousal (57.4%), followed by problems in desire (54.4%), erection (36.6%), satisfaction with orgasm (34.6%) and ability to reach orgasm was least affected (12.87%). In contrast, none of the control group participants fulfilled the overall definition of sexual dysfunction, while the prevalence of sexual dysfunction in each domain was also significantly less than that seen in AD group except for the domain of ejaculation/ability to reach orgasm. Dyadic adjustment of those with AD was poorer compared to the control group in the domains of dyadic satisfaction, affective expression and overall dyadic adjustment (Table III).
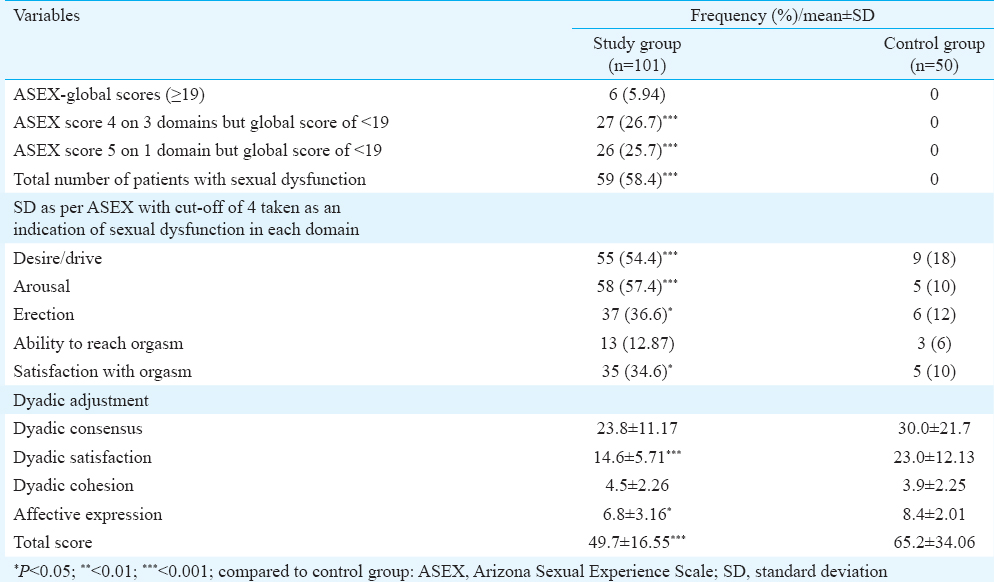
Factors associated with sexual dysfunction alcohol dependence group: Alcohol-dependent patients with or without sexual dysfunction showed no significant difference across any of the sociodemographic and clinical variables, as also the HDRS and STAI scores. However, those with sexual dysfunction recorded lower dyadic satisfaction (P<0.05) and expression (P<0.05).
Discussion
In this study appropriate inclusion and exclusion criteria were followed to ensure that the reported sexual dysfunctions were exclusively due to deleterious effects of alcohol on reproductive system. To further ensure that the reporting of sexual dysfunction was accurate, only married male patients who were in an active heterosexual relationship and whose spouses did not have a sexual dysfunction, were included. The sociodemographic profile of our study group matched with that reported for alcohol-dependent patients in previous studies from our center232425 and from other parts of India2627. The age of the patients reported in the present study was similar to that in some of the previous studies reporting on sexual dysfunction in alcohol-dependent patients427. The patient and the healthy control groups were comparable for sociodemography except for the latter being slightly more educated. Hence, the difference in the presence of sexual dysfunction in the two groups was not due to the sociodemographic variables.
The mean age of onset of alcohol use for our study patients was in line with the previous studies on AD from our centre2325. The mean duration of alcohol use of 12 yr and the duration of AD of 8.65 years reflected the use of alcohol for fairly long duration. The CIWA-Ar rating affirmed and self and family reported mean duration of abstinence from alcohol of 9.69 days confirmed that none of the patients was in active alcohol withdrawal; in contrast, some of the previous studies on sexual dysfunction in AD have not explicitly mentioned about the time of assessment1528.
Almost all (84.5%) of our patients being dependent on tobacco was in concordance with some of the existing data from India26 and West29. Previous studies evaluating the prevalence of sexual dysfunction have not discussed about this confounding variable1. However, no significant difference in the presence of tobacco dependence across our study and healthy control groups suggests that this covariate cannot be solely considered to be the cause of sexual dysfunction. In contrast to the studies from the West reporting higher rates of comorbid personality disorder in patients with AD30, in the present study, only a few patients had a comorbid personality disorder. None of our patients having syndromal depression as per the HDRS, and there being no difference in the prevalence of subsyndromal depressive symptoms in the study and control groups leads to a conclusion that the sexual dysfunction in different groups cannot be attributed to the presence of syndromal depression. Our study group having significantly higher level of state and trait anxiety compared to control group suggested that the difference in the prevalence of sexual dysfunction between the two groups could have been influenced by this variable.
Our finding of 58 per cent sexual dysfunction was in line with the previous study reporting rates ranging from 40-95.2 per cent1. The present study findings supported the existing findings that the most common alcohol-associated sexual dysfunction was erectile dysfunction, followed by sexual desire and premature ejaculation1.
The present study affirmed that sexual dysfunction in alcohol-dependent patients had a deleterious effect on marital functioning, especially in the domains of dyadic satisfaction and affective expression and supported others reporting marital satisfaction and sexual functioning having a reciprocal relationship31. This finding has implications for clinical practice. In cases with AD, marital discord or sexual dysfunction, the relationship between these three variables must be evaluated and managed thoroughly.
There were certain limitations of this study. The study was carried out in a small sample of clinic-based population, and hence the findings could not be generalized to other population groups. Future studies should try to overcome these limitations. In addition, future research should focus on longitudinal studies, on structured assessment of knowledge and attitude about the sex of alcohol-dependent men and on structured assessment of sexual dysfunction in partners of alcohol-dependent men.
This study showed that alcohol dependent men had poor sexual functioning. Whenever a patient presents with sexual dysfunction, a thorough history of alcohol and drug use/abuse/dependence must be obtained. If the patient has a history of alcohol and drug use/abuse/dependence, the efforts must be made to delineate the relationship of sexual dysfunction with the alcohol use and efforts must be made to achieve abstinence.
Conflicts of Interest: None.
References
- Sexual dysfunction in patients with alcohol and opioid dependence. Indian J Psychol Med. 2014;36:355-65.
- [Google Scholar]
- Alcohol and drug effects on sexual response: human experimental and clinical studies. Ann Rev Sex Res. 1991;2:119-79.
- [Google Scholar]
- Sildenafil citrate in the treatment of sexual dysfunction and its effect on quality of life in alcohol dependent men: preliminary findings. Alcohol Alcohol. 2007;42:340-6.
- [Google Scholar]
- Evaluation of sexual functions in Turkish alcohol-dependent males. J Sex Med. 2011;8:3181-7.
- [Google Scholar]
- Erectile dysfunction: prevalence and relationship to depression, alcohol abuse and panic disorder. Gen Hosp Psychiatry. 2003;25:209-13.
- [Google Scholar]
- Sexual dysfunction in HIV-positive men is multi-factorial: a study of prevalence and associated factors. AIDS Care. 2007;19:955-65.
- [Google Scholar]
- Alcohol consumption and male erectile dysfunction: an unfounded reputation for risk? J Sex Med. 2009;6:1386-94.
- [Google Scholar]
- Alcohol consumption and erectile dysfunction: meta-analysis of population-based studies. Int J Impot Res. 2007;19:343-52.
- [Google Scholar]
- Risk factors for low sexual function among urban Chinese women: a hospital-based investigation. J Sex Med. 2011;8:2299-304.
- [Google Scholar]
- The Mini International Neuropsychiatric Interview (M.I.N.I.) a short diagnostic structured interview: reliability and validity according to the CIDI. Eur Psychiatry. 1997;12:224-31.
- [Google Scholar]
- Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar) Br J Addict. 1989;84:1353-7.
- [Google Scholar]
- The Arizona Sexual Experience Scale (ASEX): reliability and validity. J Sex Marital Ther. 2000;26:25-40.
- [Google Scholar]
- The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992.
- The accuracy of the Arizona Sexual Experience Scale (ASEX) to identify sexual dysfunction in patients of the schizophrenia spectrum. Rev Psiquiatr Clín. 2009;36:182-9.
- [Google Scholar]
- Measuring dyadic adjustment: new scale for assessing quality of life and similar dyads. J Marital Fam Ther. 1976;38:15-28.
- [Google Scholar]
- Distress in wives of patients with psychosexual dysfunction: an exploratory study. Indian J Psychiatry. 1999;41:24-9.
- [Google Scholar]
- Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6:278-96.
- [Google Scholar]
- Manual for the state-trait anxiety inventory. Palo Alto, CA: Consulting Psychologists Press; 1970.
- Development of the Hindi edition of the state trait anxiety inventory. Indian J Psychol. 1973;48:11-20.
- [Google Scholar]
- The severity of alcohol dependence questionnaire: its use, reliability and validity. Br J Addict. 1983;78:145-55.
- [Google Scholar]
- Psychosocial factors associated with relapse in men with alcohol or opioid dependence. Indian J Med Res. 2009;130:702-8.
- [Google Scholar]
- Prevalence & correlates of metabolic syndrome in alcohol & opioid dependent inpatients. Indian J Med Res. 2011;134:341-8.
- [Google Scholar]
- Relapse precipitants, life events and dysfunction in alcohol and opioid dependent men. Indian J Psychiatry. 2003;45:39-44.
- [Google Scholar]
- Alcohol use and implications for public health: patterns of use in four communities. Indian J Community Med. 2010;35:238-44.
- [Google Scholar]
- Prevalence of sexual dysfunction in male subjects with alcohol dependence. Indian J Psychiatry. 2007;49:109-12.
- [Google Scholar]
- Prevalence of sexual dysfunction in three psychiatric outpatient settings: a drug misuse service, an alcohol misuse service and a general adult psychiatry clinic. Sex Relat Ther. 2002;17:149-60.
- [Google Scholar]
- Hypogonadism in men with erectile dysfunction may be related to a host of chronic illnesses. Int J Impot Res. 2010;22:9-19.
- [Google Scholar]
- Attachment style, anxiety coping, and personality-styles in withdrawn alcohol addicted inpatients. Subst Abuse Treat Prev Policy. 2013;8:1.
- [Google Scholar]
- The role of illicit substance use in a conceptual model of intimate partner violence in men undergoing treatment for alcoholism. Psychol Addict Behav. 2012;26:255-64.
- [Google Scholar]






