Translate this page into:
Declining HIV seropositivity: Ten years experience from a tertiatary care hospital in central India
* For correspondence: meenarishika@yahoo.co.in
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
The testing for HIV, early diagnosis and access to treatment are important factors for controlling the HIV/AIDS epidemic1. The theme of “Getting to Zero” adopted by UNAIDS for the period 2011-2015 clearly reflected optimism regarding global response to HIV2. The impact of various interventions under the National AIDS Control Programme (NACP) can be seen from an overall reduction of 57 per cent in the annual new HIV infections among adult population from 2.74 lakh in 2000 to 1.16 lakh in 20113. After the encouraging results of NACP Phase III, the NACP Phase-IV (2012-2017) aims to accelerate the process of reversal and further strengthen the HIV epidemic response in India4.
To understand the HIV/AIDS epidemiology in a particular region with reference to various socio-demographic factors, awareness, high risk behaviour, etc. The HIV reporting trends in the Integrated Counselling and Testing Centres (ICTC) provide an important clue to assess the effectiveness of the preventive strategies undertaken5. Therefore, a retrospective analysis of data from available records of all individuals who attended ICTC of Government Medical College, Nagpur, Maharashtra, India, between January 2004 and December 2013 was carried out. The present study included 60,181 ICTC attendees. The NACO guidelines of pre-test counselling, written informed consent and post-test counselling was followed6. The Strategy III of National HIV testing algorithm was followed7. Prior clearance was obtained from the Ethical Committee of the institution. The statistical analysis was done using STATA (version 10.4, 2009, STATA Corp, Texas, USA) and Epi Info 7 (version 7.1.06, 2012, CDC, Atlanta, USA). Chi-square test for linear trend (Extended Mantel Haenszel) and Student t test were used for data analysis.
A total of 60,181 individuals (37,077 male, 23,104 female) were tested for the detection of HIV antibodies. Of the 10,089 HIV seropositive cases, 6537 (17.63%) were males while 3552 (15.37%) were females. It was observed that though the maximum total per cent positivity was 33.26 per cent in 2005 and 2006, there was a steady decline in the per cent positivity from 2007onwards and it was remarkably reduced to 6.01 per cent in 2013 (Table I).
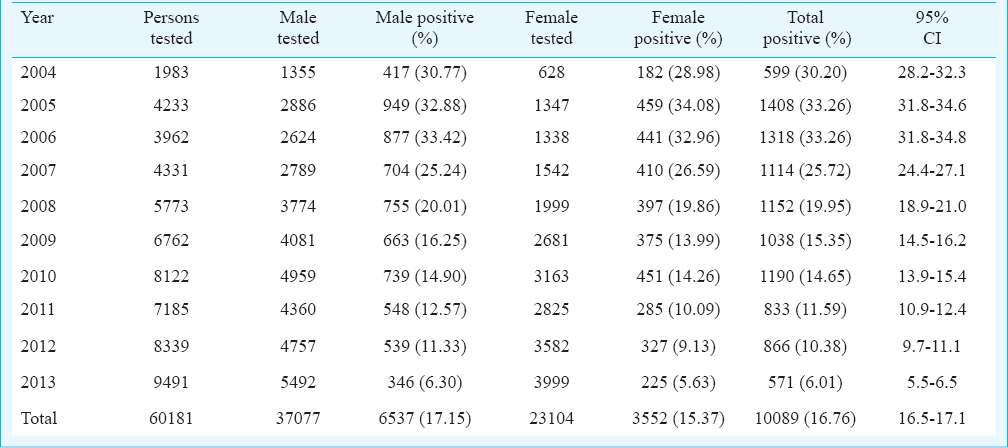
The seroprevalence in males was highest (33.42%) in 2006 which gradually declined to 6.30 per cent in 2013. The seroprevalence in the females was highest in 2005 (34.08%) which declined to 5.63 per cent in 2013. There was a significant (P<0.001) declining trend in seropositivity over the 10 years period. A similar decline in seroprevalence from 10.4 per cent in 2008 to 6.1 per cent in 2010 was observed in Andhra Pradesh8. In comparison, lower prevalence of 1.44 per cent were observed in Rajasthan9, 4.8 per cent in Ahmedabad, Gujarat10, 5.1 per cent in Andhra Pradesh8, and 5.6 per cent in Kwara, Nigeria11. A declining trend in adult HIV prevalence has been reported in high-prevalence States12. In the present study, the HIV seropositivity amongst males was 64.79 per cent and amongst females was 35.21 per cent. Similar estimates have been reported by Sekar et al1 (45.5% males and 54.5% were females) in southern India, Dash et al13 (62% males & 38% females) in Odisha and Gupta et al14 (61 and 39%) in Udupi. The last six year data (2008-2013) showed that HIV-2 seropositive cases were only 5, 8, 4, 2, 4 and 2, respectively, while combined HIV-1 and -2 cases were 29, 57, 18, 18, 13 and 9 during these years. A very low seroprevalence of combined HIV-1 & -2 and only HIV-2 was observed in our study from the data available since 2009-2013. Similar finding has been reported by Kannangai et al15.
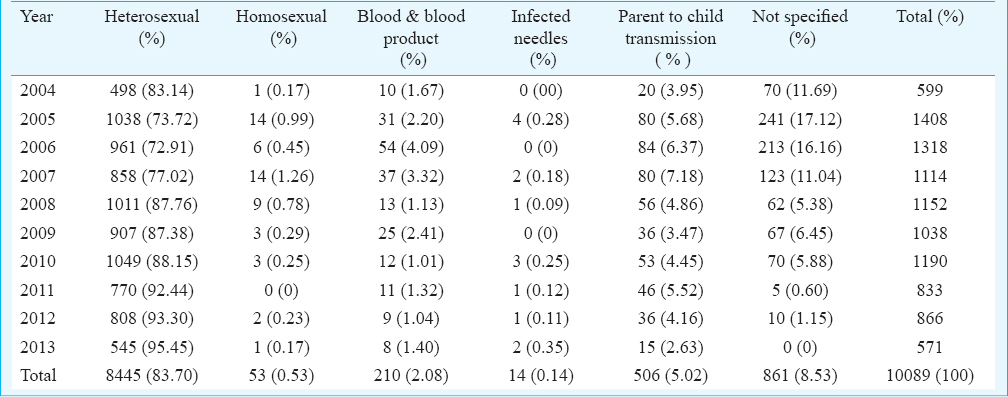
The age-wise distribution of total seropositive cases showed the maximum seropositivity (4420, 43.81%) in 25-34 yr age group. The age-wise distribution in seropositive males was 303 (4.63%), 290 (4.44%), 2787 (42.63%), 2487 (38.04%) and 670 (10.25%) and in seropositive females was 313 (8.81%), 420 (11.82%), 1633 (45.97%), 970 (27.31%) and 216 (6.08%) in the age groups 0-14, 15-24, 25-34, 35-49 and ≥ 50 yr, respectively. Thus, the maximum seropositivity was seen in the same age group in both the sexes. In the seropositive cases, the commonest route of transmission was heterosexual seen in 83.70 per cent cases (Table II). Chi square test for linear trend (Extended Mantel Haenszel) indicated a significant association (P<0.05) between the route of transmission and prevalence of HIV. In our study, the parent-to-child transmission of HIV was 5.02 per cent which was similar to earlier studies; (5.6 to 12%)5, (5.8%)13 and (4.16%)16. There was a reduction in positive cases over the recent years especially from 2007 with 7.18 to 2.63 per cent in 2013. Transmission by other modes like homosexual transmission (0.53%), blood transfusion (2.08%), and infected needles (0.14%) was low similar to that reported earlier816.
Our study had some limitations. The results were based on data collected from the persons attending the ICTC setup only. The data on HIV-2 prevalence before 2009 were not available. The strength of the study was that the data presented useful epidemiological information about the HIV epidemic and the steady decline in HIV prevalence indicated the effectiveness of the present interventions of NACP III and the ongoing NACP IV programme. This needs to be strengthened further.
Acknowledgment
Authors thank Maharashtra State AIDS Control Society and NACO for providing the kits for HIV testing and to the technical staff and counsellors of ICTC for their assistance.
Conflicts of Interest: None.
References
- Recent trends in HIV prevalence in a remote setting of southern India: Insights into arranging HIV control policies. J Infect Dev Ctries. 2013;7:838-43.
- [Google Scholar]
- ‘Getting to Zero’: are there grounds for optimism in the global fight against HIV? Indian J Med Res. 2012;136:895-8.
- [Google Scholar]
- Annual Report 2013-2014. Government of India: National AIDS Control Organization (NACO). Available from: http://www.naco.gov.in
- National AIDS Control Program Phase IV (2012-2017). Department of AIDS Control, Ministry of Health & Family Welfare, Government of India. Available from: http://www.naco.gov.in
- Prevalence of HIV/AIDS and prediction of future trends in north-west region of India: A six-year ICTC-based study. Indian J Community Med. 2009;34:212-7.
- [Google Scholar]
- National guidelines for HIV testing manual - July 2015. Ministry of Health & Family Welfare, Government of India: National AIDS Control Organization (NACO). Available from: http://www.naco.gov.in
- Laboratory testing for the diagnosis of HIV infection: Updated Recommendations. Centers for Disease Control and Prevention (CDC) 2014. Available from: http://stacks.cdc.gov/view/cdc/23447
- Profile of HIV positive clients in an ICTC of a private medical college, Andhra Pradesh: A situational analysis. Natl J Integr Res Med. 2012;3:36-40.
- [Google Scholar]
- Profile of patients who attended the HIV integrated counseling and testing centre in a teaching hospital of Rajasthan, India. J Clin Diagn Res. 2012;6:195-7.
- [Google Scholar]
- Profile of attendee for voluntary counseling and testing in the ICTC, Ahmedabad. Indian J Sex Transm Dis. 2009;30:31-6.
- [Google Scholar]
- India HIV estimations 2015. Technical Report. NACO & National Institute of Medical Statistics, ICMR. Ministry of Health & Family Welfare, Government of India. Available from: http://www.naco.gov.in
- HIV counseling and testing in a tertiary care hospital in Ganjam district, Odisha, India. J Postgrad Med. 2013;59:110-4.
- [Google Scholar]
- Profile of clients tested HIV positive in a voluntary counseling and testing center of a District Hospital, Udupi. Indian J Community Med. 2009;34:223-6.
- [Google Scholar]
- Frequency of HIV type 2 infections among blood donor population from India: A 10-year experience. Indian J Med Microbiol. 2010;28:111-3.
- [Google Scholar]
- Socio-demographic profile of clients enrolled at the ICTC of a teaching institute in Kolhapur, India. Online Int Interdiscipl Res J. 2013;3:343-51.
- [Google Scholar]





