Translate this page into:
Healthcare associated infections in Paediatric Intensive Care Unit of a tertiary care hospital in India: Hospital stay & extra costs
Reprint requests: Dr Sidhartha Satpathy, Department of Hospital Administration, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110 029, India e-mail: sidharthasatpathyresearch@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Healthcare associated infections (HAIs) increase the length of stay in the hospital and consequently costs as reported from studies done in developed countries. The current study was undertaken to evaluate the impact of HAIs on length of stay and costs of health care in children admitted to Paediatric Intensive Care Unit (PICU) of a tertiary care hospital in north India.
Methods:
This prospective study was done in the seven bedded PICU of a large multi-specialty tertiary care hospital in New Delhi, India. A total of 20 children with HAI (cases) and 35 children without HAI (controls), admitted to the PICU during the study period (January 2012 to June 2012), were matched for gender, age, and average severity of illness score. Each patient's length of stay was obtained prospectively. Costs of healthcare were estimated according to traditional and time driven activity based costing methods approach.
Results:
The median extra length of PICU stay for children with HAI (cases), compared with children with no HAI (controls), was seven days (IQR 3-16). The mean total costs of patients with and without HAI were  2,04,787 (US$ 3,413) and
2,04,787 (US$ 3,413) and  56,587 (US$ 943), respectively and the mean difference in the total cost between cases and controls was
56,587 (US$ 943), respectively and the mean difference in the total cost between cases and controls was  1,48,200 (95% CI 55,716 to 2,40,685, P<0.01).
1,48,200 (95% CI 55,716 to 2,40,685, P<0.01).
Interpretation & conclusions:
This study highlights the effect of HAI on costs for PICU patients, especially costs due to prolongation of hospital stay, and suggests the need to develop effective strategies for prevention of HAI to reduce costs of health care.
Keywords
Central line associated blood stream infection
healthcare associated infection
hospital stay
Paediatric Intensive Care Unit (PICU)
ventilator associated pneumonia
Healthcare associated infections (HAIs) in the Paediatric Intensive Care Units (PICUs) are a major clinico-managerial problem resulting in prolonged length of hospital stay, increased medical costs, and increased morbidity and mortality1-6. Only a few studies, based on prospective, patient-based surveillance have estimated the burden of HAI in the paediatric age group7-10. Children, hospitalized in ICUs, are unique population with regards to their specific risk factors for HAIs. Majority of HAIs which occur in intensive care units are associated with the use of invasive devices such as a central line (CL) or mechanical ventilator11. The length of stay (LOS) and costs attributable to Central Line Associated Blood Stream Infection (CLABSI), the most common HAI in PICU, were 14.6 days and US$ 46,133, respectively12. There is no information available on costing of HAI in PICU from hospitals in India. In order to enable hospital administrators to identify the most convenient strategies for reducing the impact of HAIs, it is important to have reliable data on the costs borne by the hospital for HAIs and on the cost opportunity to implement an innovative technology aimed at reducing the burden. The information related to cost per case of HAI can guide decision making regarding the prevention of HAI by indirectly providing the expected cost saving from extra infection control13. The objective of this study was to evaluate the impact of Hais on length of hospital stay and cost of health care in the children admitted to PICU in a tertiary care hospital in north India, to estimate the potential effect of infection control measures.
Material & Methods
This prospective study was conducted from January to June 2012 at the Paediatric Intensive Care Unit (PICU) of All India Institute of Medical Sciences (AIIMS), a tertiary care hospital in New Delhi, India. The PICU has facility of seven beds for intensive care and admits approximately 220 children annually. The study protocol was approved by the Institutional ethics committee. Informed written consent was taken from the family member/guardian of the child.
Patient eligibility and assessment: All children admitted in PICU from January to June 2012 were screened for HAI. The incidence rate or crude infection rate (CIR) of HAIs was taken using CDC National Noscomial Infections Surveillance (NNIS) protocols14. For CIRs, the denominator was the number of patients with a specific device for greater than or equal to 48 h. This was to define as HAIs as per CDC guidelines14. Children who stayed for greater than or equal to 48 h in PICU and were diagnosed with HAI during their stay, as per the CDC criteria for site-specific infections were enrolled in the study. Children who were admitted in PICU for less than 48 h were excluded. Children who had been diagnosed with HAI prior to admission to the PICU were also excluded.
Children, who developed HAI in PICU during the study period, were classified as “cases” while children who did not develop HAI anytime during their stay in PICU were eligible to serve as “controls”. For multiple admissions and/or multiple infections, only the first PICU admission and/or HAI episode was considered.
Case identification and case-control matching: Case identification was based on the following criteria: (i) Clinical: based on the review of information in the patient's charts, (ii) Laboratory: based on results of blood cultures, bronchoalveolar lavage (BAL) cultures, and (iii) Supportive evidence: derived from diagnostic tests and results of X-rays. HAIs was suspected based on the CDC criteria. For example, ventilator associated pneumonia (VAP)was suspected in a mechanically ventilated child after 48 h of PICU stay if the child had fever, or increased respiratory tract secretions or increased requirement of ventilator support. The clinical team suspected and investigated for HAIs as per protocol. The team also considered urinary tract infection (UTI)/catheter associated urinary tract infection (CAUTI) as one of the HAIs. Cases were matched to the controls on the basis of the following three variables: (i) Age (in months) + 60 months; (ii) Gender; (iii) Average severity of illness score; paediatric index of mortality 2 (PIM 2 score). Patients had to match exactly on all the three variables to become controls.
Sample size estimation: The study was conducted over a period of six months during which approximately 100 children were likely to be admitted in the PICU. The sample size estimation was done on the basis of detection rate of HAI in accordance with studies on similar subject from developed countries1516. In absence of any systematic data available on costing of HAI from PICU in India, the sample size estimation was done taking the basis of incidence rate from results of a study by Gupta et al17 regarding the incidence of nosocomial infections in the same PICU of AIIMS, where approximately 36 of the 187 patients developed HAI. Using this assumption, a total sample size of 101 was calculated to detect a 20 per cent HAI in the admitted children over a period of six months.
Resource consumption and cost estimation: Once the cases and controls were identified, data on each patient's length of stay in PICU were obtained prospectively on daily basis. Costing heads considered were material, machine, manpower and money. Cost per unit was calculated for different facilities and services of the hospital related to PICU. Fixed and variable costs were enlisted; fixed costs were the costs that did not vary with the production volume (e.g. Cost of facility, cost of equipment) while variable costs were the costs that varied directly and proportionately with the production volume (e.g. Cost of consumables). Resources were classified as direct, if the consumption was entirely attributable to the patient's hospital stay; indirect, if it was difficult to trace the consumption to the patient (e.g. Air-conditioning, electricity); and overhead, if it was impossible to attribute the consumption to any specific patient (e.g. Building cost). Direct costs were evaluated in monetary terms through a traditional costing approach, where quantities and unit costs were first estimated and then multiplied. Indirect costs and overheads were calculated at the PICU level and allocated on the basis of per bed per day. Data on consumption of resources were collected through record inspection and review and quantitative information provided by the “key informants”. The key informants included all the relevant personnel dealing in their specific domains of hospital operation. For example, data pertaining to salary of manpower for different categories of staff of PICU was taken from the hospital accounts department. The cost of facility was deduced with the help of dimensions of PICU (in sqm) taken from the engineering department. Cost of consumables was ascertained with help of their unit costs taken from the stores personnel. Consumables included medicinal, surgical, crystalloids, stationary, and linen and general items. Consumption of these items was studied for a period of six months concurrently when the data were being collected for cases and controls. Indirect costs included cost of facility, cost of equipment, fixtures and fittings, cost of air-conditioning, cost of electricity, cost of laundry, dietary, manifold, central sterile supply department, blood bank, etc. All these indirect costs were calculated and deduced to the cost of PICU bed per day. Cost of facility was calculated on the basis of the area of PICU (in sqm) which was taken from the engineering department. Cost of construction per sqm for the hospital building was calculated as per Central Public Works Department (CPWD) manual 2007 and the present rate was calculated after adjusting with the cost inflation index (CII). For cost of PICU equipment, a list of the equipment was generated with the help of in-charges of the department and the cost was gathered from the department (if the same had been provided by the department) or stores as per the source of procurement. Cost of air-conditioning equipment was calculated with the help of air conditioning division of engineering department. The total electricity consumption at the PICU level, on central air-conditioning was determined based on the energy consumption rate of the equipment. Time driven activity based costing method (TDABC)18 was used to compute the cost of electricity consumed by the various equipment, fixtures and fittings used in PICU. Wattage of these equipment, fixtures was taken in consultation with the engineering department. The number of hours of their usage was taken from the PICU staff. The total number of units consumed in 24 h by all the equipment and fixtures in a PICU was calculated and multiplied with the charge per unit. All the direct and indirect costs entailed were converted into cost of PICU bed per day.
Cost of HAI: Cost of one HAI was calculated as the difference in costs between children who developed HAI (cases) and those who did not get HAI (controls), after matching for selected variables defined above.
Data management and statistical analysis: All statistical analyses were performed using the software STATA 9.0 (Stata Corp., College Station, TX, USA). Means with standard deviations were used to describe continuous variables, while medians were calculated for non-normal distributed continuous variables. Clinical and demographic differences between the two groups (cases and controls) were analyzed by performing Student t test. Difference in the length of stay between the two groups was compared with the Mann-Whitney U test and the difference between costs for the two groups was compared by using the Student t test.
Results
A total of 119 children admitted in the PICU from January to June 2012 were screened, of whom 20 (16.8%) eligible children who developed HAI were enrolled as cases and 35 (29.4%) eligible children who did not develop HAI were enrolled as controls. Of the 20 cases who met the study criteria, seven (35%) died during their hospital stay. The remaining 13 cases were included in the final analysis. After matching of cases with controls, 13 controls were selected out of 35 for comparison. Amongst enrolled children there were 10 males (76.92%) and 3 females (23.08%) in each group.
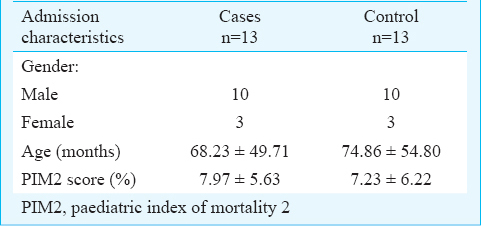
The PICU children with HAI and those without HAI were comparable for admission characteristics (Table I). The mean severity of illness as determined from PIM 2 score was similar in the two groups.
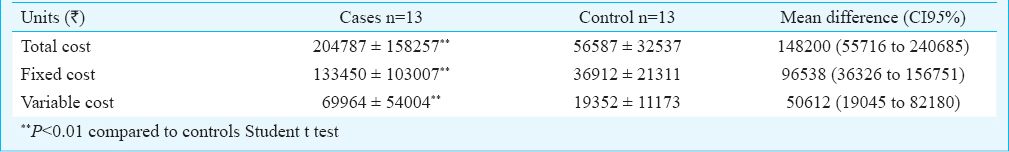
The median length of stay in cases who stayed for greater than or equal to 48 h was 14 days [interquartile range (IQR)-7, 18] while in controls it was three days (IQR 2, 5, P<0.01). Compared to controls, the median extra stay in cases was seven days (IQR 3, 16). The proportions of cases who had stayed greater than or equal to three days and less than five days were 1 (7.7%), greater than or equal to five days and less than seven days were 2 (15.4%) and greater than or equal to seven days were 7 (53.9%), respectively. The mean total costs of patients with and without HAI were  2,04,787 (US$ 3,413, 1 US$ = 60
2,04,787 (US$ 3,413, 1 US$ = 60  ) and
) and  56,587 (US$ 943), respectively and the mean difference in the total cost between a case and control was
56,587 (US$ 943), respectively and the mean difference in the total cost between a case and control was  1,48,200 (95% CI 55,716 to 2,40,685, P<0.01). The mean fixed costs were
1,48,200 (95% CI 55,716 to 2,40,685, P<0.01). The mean fixed costs were  1,33,450 (US$ 2,224) and
1,33,450 (US$ 2,224) and  36,912 (US$ 615), respectively amongst cases and controls. The mean variable costs were
36,912 (US$ 615), respectively amongst cases and controls. The mean variable costs were  69,964 (US$ 1,166) and
69,964 (US$ 1,166) and  19,352 (US$ 323), respectively amongst cases and controls (Table II). For the fixed costs the significant contributors were manpower (77%) and equipment (18%) while variable costs were largely contributed by drugs and consumables (72%). The differences in the costs for the two groups were particularly evident for utilization of manpower, drugs and consumables and equipment. In both groups, length of stay represented the most significant cost component of the overall cost for cases and controls, respectively.
19,352 (US$ 323), respectively amongst cases and controls (Table II). For the fixed costs the significant contributors were manpower (77%) and equipment (18%) while variable costs were largely contributed by drugs and consumables (72%). The differences in the costs for the two groups were particularly evident for utilization of manpower, drugs and consumables and equipment. In both groups, length of stay represented the most significant cost component of the overall cost for cases and controls, respectively.
Discussion
This study was performed to estimate the economic burden imposed by HAI occurring in the children admitted to PICU of a tertiary care hospital in India. The majority of the additional costs incurred were due to a prolonged hospital stay which was similar to that reported in most of the studies3-6. Children with HAI, on an average, incurred hospital costs that were almost 3.6 times higher than those without HAI. Previous studies from developing countries reported an average excess cost of US$ 4,888 and 11,591, respectively which were associated with bloodstream infection1920. A prospective study by Elward et al21 found out the direct cost of PICU admission attributable to nosocomial primary bloodstream infections (BSIs) to be US$ 39,219. Our results confirmed that hospital stay represented the most significant part of the overall costs in both categories of children, and primarily accounted for the difference in the incremental costs between the two groups of children in PICU.
Our study had some limitations. Firstly, the small sample size as the study was conducted for a period of six months only during which only 13 cases could be matched with the controls. Deaths were not included in the analysis as it was not possible to anticipate the actual length of stay in the cases who died in the PICU. Secondly, we compared the HAI cases with controls; so matching with respect to organism between cases and controls could not be done. Our sample size limited the ability to look at HAI organism specific costs. Thirdly, the children with HAI (cases) were matched with the children without HAI (controls) for a few baseline parameters like age, gender and average severity of illness score. It is certainly desirable to match for other factors such as co-morbidities. However, with increasing numbers of parameters to be matched, the feasibility of getting adequate number of controls is adversely impacted. It is important to underscore that the present research was conducted from the hospital perspective. Because of this, the time horizon of the analysis was limited to the hospitalization period of PICU. It is arguable, however, that HAIs impose significant burden in other settings as well. Following discharge, children who suffered a HAI might consult primary and community care services, such as general practitioners. Further analysis could, therefore, be considered to expand the perspective of this analysis. It may be noted that the cost of PICU bed calculated per day represents an average total cost and results obtained in this hospital may not be representative to the production cost function in other settings.
To conclude, our preliminary results provide information regarding the impact of HAI on costs for PICU patients, especially costs due to prolongation of hospital stay and increased hospital resources. In the absence of any systematic data available on costing of HAI from PICU in India, this can be considered as useful preliminary data which may facilitate better informed decisions about the adoption of effective strategies for prevention of HAI to reduce patient morbidity and costs associated with provision of health care.
Acknowledgment
Authors acknowledge the cooperation of the nursing staff of PICU as well as that of the parents of the two groups, and thank Drs Nishant Verma, Deep Chand, Satish, Priyanka and Gautam for providing clinical details pertinent to children of the two groups of PICU. Authors also acknowledge the contribution of staff of hospital stores for providing the costs of consumables and thank Shri Dharmendra Sharma who significantly contributed for data management support, quality check and analysis of data.
Conflicts of Interest: None.
References
- Nosocomial infections in a pediatric intensive care unit. Crit Care Med. 1988;16:233-7.
- [Google Scholar]
- Nosocomial infection in a pediatric intensive care unit in a developing country. Braz J Infect Dis. 2003;7:375-80.
- [Google Scholar]
- One year study of bacterial and fungal nosocomial infections among patients in pediatric intensive care unit (PICU) in Alexandria. J Trop Pediatr. 2006;52:185-91.
- [Google Scholar]
- Nosocomial infections in pediatric patients: a European, multicenter prospective study. European Study Group. Infect Control Hosp Epidemiol. 2000;21:260-3.
- [Google Scholar]
- Prospective incidence study of nosocomial infections in a pediatric intensive care unit. Pediatr Infect Dis J. 2003;22:490-4.
- [Google Scholar]
- Incidence density and relative risk of nosocomial infection in Taiwan's Only Children's Hospital, 1999-2003. Infect Control Hosp Epidemiol. 2008;29:767-70.
- [Google Scholar]
- Nosocomial bloodstream infection in a pediatric intensive care unit. Indian J Pediatr. 2008;75:25-30.
- [Google Scholar]
- Nosocomial pneumonia in a pediatric intensive care unit. Indian Pediatr. 2007;44:511-8.
- [Google Scholar]
- Study of nosocomial primary bloodstream infections in a pediatric intensive care unit. J Trop Pediatr. 2007;53:87-92.
- [Google Scholar]
- Prevention of intravascular catheter-related infections. Ann Intern Med. 2000;132:391-402.
- [Google Scholar]
- The costs associated with nosocomial bloodstream infections in the pediatric intensive care unit. Pediatr Crit Care Med. 2001;2:170-4.
- [Google Scholar]
- Economic evaluation and catheter-related bloodstream infections. Emerg Infect Dis. 2007;13:815-23.
- [Google Scholar]
- Centers for Disease Control (CDC). Public health focus: surveillance, prevention, and control of nosocomial infections. MMWR Morb Mortal Wkly Rep. 1992;41:783-7.
- [Google Scholar]
- Prolongation of hospital stay and additional costs due to nosocomial bloodstream infection in an Algerian neonatal care unit. Infect Control Hosp Epidemiol. 2008;29:1066-70.
- [Google Scholar]
- A prospective study of ventilator-associated pneumonia in children. Pediatrics. 2009;123:1108-15.
- [Google Scholar]
- Burden of healthcare-associated infections in a paediatric intensive care unit of a developing country: a single centre experience using active surveillance. J Hosp Infect. 2011;78:323-6.
- [Google Scholar]
- Time-driven activity based costing. Haward Business School Working Paper. Haward, USA: Haward Business School Publishing Corporation; 2003. p. :4-45.
- [Google Scholar]
- The attributable cost, length of hospital stay, and mortality of central line-associated bloodstream infection in intensive care departments in Argentina: A prospective, matched analysis. Am J Infect Control. 2003;31:475-80.
- [Google Scholar]
- Attributable cost and length of stay for patients with central venous catheter-associated bloodstream infection in Mexico City intensive care units: a prospective, matched analysis. Infect Control Hosp Epidemiol. 2007;28:31-5.
- [Google Scholar]
- Attributable cost of nosocomial primary bloodstream infection in pediatric intensive care unit patients. Pediatrics. 2005;115:868-72.
- [Google Scholar]






