Translate this page into:
Eradicating successfully yaws from India: The strategy & global lessons
Reprint requests: Dr Jai Prakash Narain, National Centre for Disease Control 22, Sham Nath Marg, Delhi 110 054, India e-mail: narainjp88@gmail.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Yaws, a non-venereal treponematosis, affecting primarily the tribal populations, has been considered historically as one of the most neglected tropical diseases in the world. In 1996, India piloted an initiative to eradicate yaws based on a strategy consisting of active case finding through house-to-house search and treatment of cases and their contacts with long acting penicillin. Thereafter, the campaign implemented in all 51 endemic districts in 10 States of the country led to the achievement of a yaws-free status in 2004. In the post-elimination phase, surveillance activities accompanied by serological surveys were continued in the erstwhile endemic districts. These surveys carried out among children between the age of 1-5 yr, further confirmed the absence of community transmission in the country. The experience of India demonstrates that yaws can be eradicated in all endemic countries of Africa and Asia, provided that political commitment can be mobilized and community level activities sustained until the goal is achieved.
Keywords
Eradication
India
strategy
yaws
Yaws, a disfiguring and debilitating disease caused by Treponema pallidum subspecies pertenue, is one of the most neglected tropical diseases in the world. Primarily a disease of tribal populations living in remote rural areas, yaws affects those on the fringes of the society who inhabit areas where health services are virtually non-existent12. Historically, the presence of yaws has been considered a sign of backwardness. Like the saying goes “where the road ends, yaws begins”.
Not a fatal disease, yaws causes disabilities and visible deformities of the face and extremities contributing to stigma and discrimination, thus keeping the afflicted from participating in normal family or community life. It affects mostly young children, who end up disabled, stigmatized and unable to complete even primary school3. As a result, they have poor intellectual development and reduced work and income opportunities in their adult life. However, the disease can be cured and prevented by a single injection of long-acting penicillin.
Presently, yaws is reported from 14 countries spread across three regions of WHO namely Africa, South-East Asia and Western Pacific regions; 21 to 42 million people live in endemic areas4 (Fig. 1). Until recently, India also reported yaws from some localized areas; in 1996, it reported 3571 cases from 51 districts in 10 States, with nearly 90 per cent cases occurring in three states of Odisha, Chattisgarh and Andhra Pradesh56 (Fig. 2).
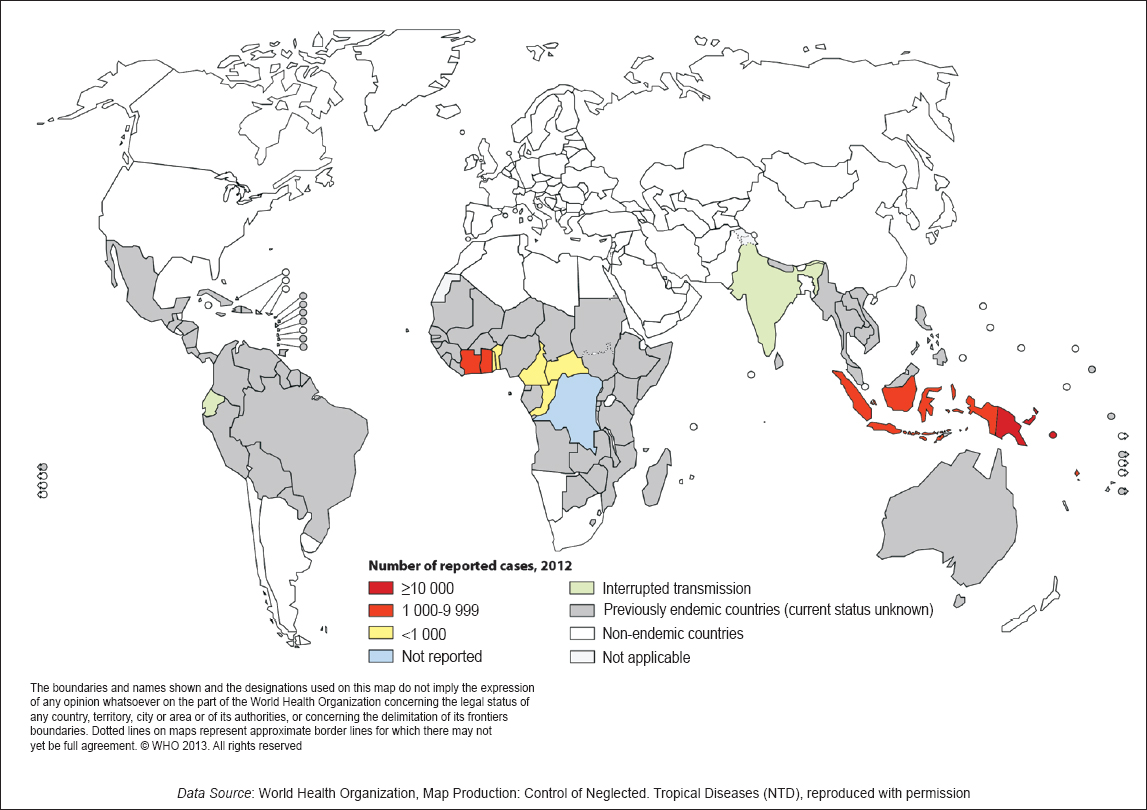
- Distribution of yaws, worldwide, 2012.
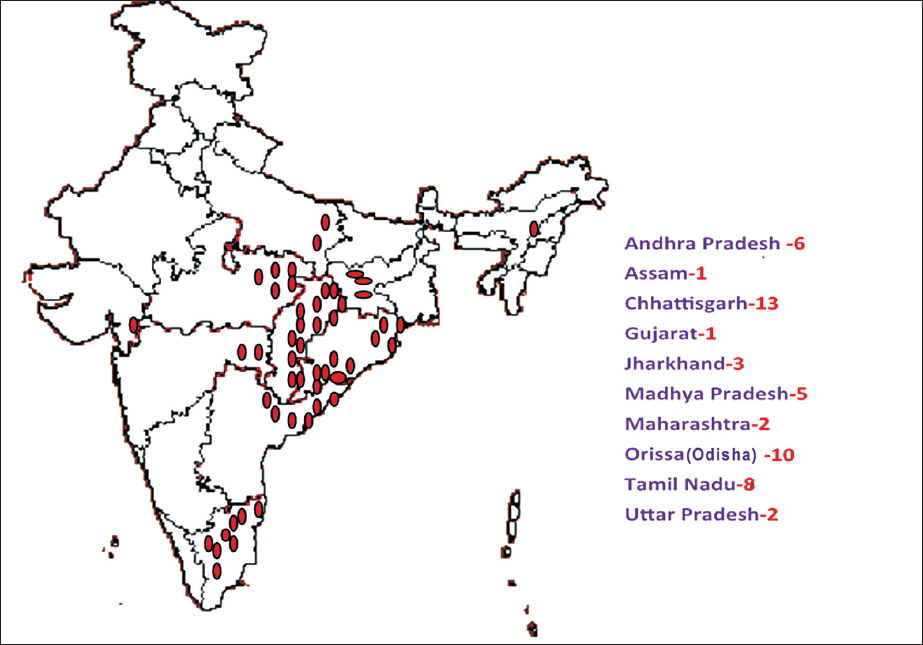
- Yaws endemic States (10) and districts (51) in India. Source: Ref. 6
Tragically, yaws for years was considered neither a global priority nor a regional priority, and remained neglected both from policy as well as programme point of view. However, since it primarily affects populations which are poorest of the poor and the most marginalized in the society, controlling or eliminating the disease is not only a social responsibility but also an ethical imperative for the national governments7.
Policy rationale
Keeping this in view, during the mid-1980s the Government of India decided to assess the extent of yaws problem in the country8. Based on the data so obtained, the government took the initiative to renew its efforts to eradicate yaws based on the premise that yaws eradication can not only alleviate the suffering of the tribal populations but also assist in bringing them out of economic deprivation9. Moreover, since women and children are at particularly high risk, the disease has a negative impact on reproductive and general health and on nutritional status as well.
Several other factors helped India decide to launch the eradication programme, including - (i) epidemiological: there is no extra-human reservoir of infection and the disease is endemic only in limited albeit difficult and hard to reach areas; (ii) technological: simple diagnostic tests and effective low cost treatments are available; the use of a single intra-muscular injection of long-acting benzathine penicillin to cases and their contacts can cure the disease and interrupt transmission; (iii) historical: the disease was almost eradicated during the 1950s; and (iv) perhaps most importantly, the Government of India was convinced that eradication of yaws was an attainable goal and was committed to achieve the goal10.
India launched an anti-yaws campaign in 1952 with assistance from WHO and UNICEF. From 1952 to 1964, the campaign detected and treated about 200 thousand cases in four States, namely Orissa (now Odisha), Andhra Pradesh, Maharashtra and Madhya Pradesh5. The prevalence of yaws declined from 14.4 to 1.1 per cent in Odisha, from 5.6 to 0.3 per cent in Andhra Pradesh, and 5.5 to 1.4 per cent in the Bastar district of Madhya Pradesh. However, after the remarkable initial success, complacency set in. The active yaws eradication efforts were gradually abandoned in the country and the strategy changed from active case finding and treatment to passive surveillance as part of general health services.
It is ironic that yaws control was left for general health services to take care of, in the very areas where there were virtually no health care services existing in the first place. Unsurprisingly, as a result the disease began to re-emerge in the late 1970s11.
Eradication strategy and its implementation
In 1986, the National Institute of Communicable Diseases (NICD), encouraged by the success of smallpox eradication during the 1970s and progress being made in eradication of guinea worm disease in the country during the early 1980s, organized a meeting to develop a strategy for yaws eradication9. The strategy agreed to in the consultation consisted of (i) active search for and treatment of infectious cases, and (ii) health education and social mobilization in the community. Cases were to be treated with long-acting benzathine penicillin, thereby rendering them non-infectious; simultaneously, the family contacts given penicillin shots as prophylaxis. In cases sensitive to penicillin, tetracycline or erythromycin was recommended for a period of 15 days. More recently, studies have shown the efficacy of single-dose azithromycin for treatment of yaws in children12.
The strategy was first piloted in Koraput district in Odisha during 1996-1997 to ascertain the feasibility of its implementation as a part of the programme. Subsequently, based on positive feedback from the pilot studies, the national programme was extended to four more States, namely Andhra Pradesh, Gujarat, Madhya Pradesh and Maharashtra. By 1999, the programme was expanded to all 51 districts in 10 States where yaws cases were reported in the past (Fig. 2).
In the field, active case search operations were carried out by multipurpose workers and community level functionaries, who visited house-to-house carrying a coloured disease recognition card and other health education materials looking for yaws cases. The treatment consisted of penicillin injections (1.2 million units for those above 10 years and 0.6 million units for children below 10 yr), preceded by testing for sensitivity to penicillin. The health care workers were trained and logistics arranged prior to the field operations. Health promotion campaigns were launched to sensitize the community and to seek their participation. The active search and treatment operations were carried out at 6-monthly intervals—before and after monsoon seasons. In addition to active search, cases which were routinely diagnosed at health centres were also treated and their contacts given prophylaxis.
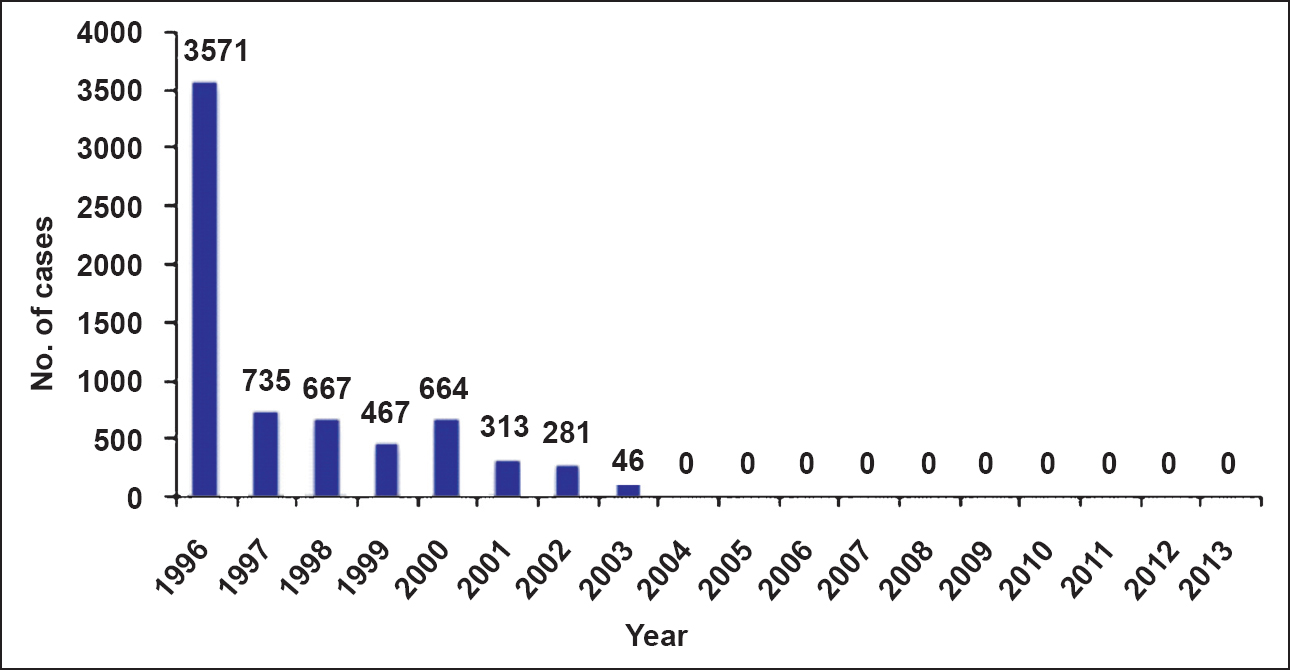
Through active case search and routine reporting, the programme detected and treated about 7000 infectious cases and their contacts. The strategy was highly effective, as the number of yaws cases detected in the country started declining rapidly; from 3571 cases in 1996 to 664 in 2000 (a reduction of more than 80%) and only 46 three years later6. The last case was diagnosed and treated in Mayurbhanj district, Odisha in 2003613 (Fig. 3), thereby achieving the interim goal of yaws elimination set by the programme (no yaws case status) in 200414. At the recommendation of the task force, the Government of India on September 19, 2006 formally declared having achieved yaws elimination6.
Moving from elimination to eradication
To move from yaws elimination to eradication, defined by the programme as absence of new cases for a continuous period of three years, supported by data indicating absence of transmission through serological surveys among children, a road map was developed based on consensus building among yaws experts in the country10. The road map consisted of three new activities: (i) serological surveys among children between one and five years of age to assess cessation of community transmission of yaws, (ii) rumour reporting and verification, and (iii) institution of cash reward for anyone reporting a yaws case, in addition to the information and communication activities and active search for cases which were continued on yearly basis.
Many rumours of possible yaws cases were verified as non-yaws over the next five years. And, no one came forward to receive the cash award. During the 2009-2011 period, serological surveys were carried out among randomly selected children using rapid plasma reagin (RPR) test with treponema pallidum haemagglutination Assay (TPHA) for confirmation. Of the 18,217 children surveyed in the erstwhile yaws villages, no serological evidence of yaws infection was found (Jain SK, personal communication). Simulteneously, for comparison purposes, 39319 children in non-yaws villages were tested and none were found positive, collectively indicating cessation of yaws transmission in the community and in the country as a whole (Jain SK, personal communication).
While the overall programme was planned, implemented and coordinated by NICD (now called National Centre for Disease Control or NCDC), the programme performance at the field level was evaluated by an independent set of experts through appraisal missions. At the highest level, the programme was monitored by a task force under the chairmanship of the Director General of Health Services, Government of India. The independent appraisal missions also reported back to the Task Force. Since 2000, six such independent appraisal missions were fielded; the last and sixth mission consisting of 16 teams was undertaken during May and June 2014 and visited 16 districts in 10 States (Jain SK, personal communication).
Lessons learnt
Yaws eradication was a singular achievement for public health in India. The single key factor responsible for the success was the sustained effort of health care workers on the frontline, supported by programme staff, working under trying field conditions, in the affected areas. Several important lessons were learnt during the campaign. The most important among those were as follows:
First, yaws is immensely amenable to eradication due to a number of favourable factors-there is no animal reservoir; only a few localized foci of infection remain; a single intra-muscular injection of long-acting penicillin completely cures the disease; and the diagnosis of yaws can be done clinically with minimum training of staff and through community education. However, efforts must be continued until the last case is diagnosed, treated, and cured.
Second, to achieve the goal of yaws eradication, not only is a high level of political commitment needed but must be sustained over time so that the programme achieves its ultimate goal of eradication. For the field operations, human resources and logistic support were provided by the State governments while the Government of India, besides policy support, ensured funding support for supplies, training, search operations, and for monitoring missions and feedback.
Third, partnership among various sectors and stakeholders engaged in the programme was essential for success. Besides the Health Directorate, other sectors namely Department of Tribal Welfare and other institutions such as Panchayati Raj, Education, Forest, etc. were actively engaged in the yaws eradication effort. The programme's performance was monitored by independent appraisal missions consisting of experts. They visited the field at regular intervals for verification of the progress being made to ensure that yaws cases are no longer existing and that community transmission is interrupted, even at the risk of their personal safety and security.
Fourth, the programme was implemented through the existing health care delivery system of the State health directorates. No new staff were hired for the programme implementation. Successful programme implementation was facilitated by a target oriented campaign, provision of supportive supervision during field activities, improved communication from the field to NCDC, and regular review meetings of State programme officers to review progress and share lessons learnt.
Finally and most importantly, the success of the programme could be attributed to a technically sound strategy which proved effective in trying field conditions. The programme was primarily funded by the government out of its own resources and as a part of its national 5-year Plan, with additional technical and financial support from the WHO.
Conclusions
The achievement of yaws eradication in India is an excellent example of a triumph of public health over a disease which still afflicts many populations in remote areas in Africa and Asia. The Indian experience clearly shows that with commitment and renewed efforts, the disease can be eradicated from all those countries of the world where yaws is still prevalent. Programmes such as these can go beyond health and play a role in enhancing the socio-economic conditions of people long neglected from policy point of view15. As stated above, the eradication campaign in India was conceived with the idea of not only alleviating the suffering of the poor, predominantly tribal population, but also with a view that the programme could contribute to the economic empowerment of remote areas and work as an entry point for primary health care for people living in these areas.
The anecdotal information is available (Jain SK, personal communication) to suggest that yaws eradication has brought about considerable improvements in the lives of tribal people, and has been instrumental in stimulating productivity and economic growth in these otherwise impoverished and so-called backward areas of the country. With improvements in living conditions, sanitation, and health and nutritional levels, the eradication programme is contributing towards poverty reduction among neglected populations living in hard to reach areas.
References
- Elimination of neglected tropical diseases in the South-East Asia Region of the World Health Organization. Bull World Health Organ. 2010;88:206-10.
- [Google Scholar]
- Endemic treponematoses. In: Cohen J, Powderly SM, Opal WG, eds. Infectious diseases (3rd ed). London: Elsevier; 2010. p. :1106-9.
- [Google Scholar]
- Yaws eradication: past efforts and future perspectives. Bull World Health Organ. 2008;86:499-499A.
- [Google Scholar]
- WHO. Yaws and other endemic treponematoses: epidemiological situation. Available from: http://www.who.int/yaws/epidemiology/en/
- [Google Scholar]
- National Centre for Disease Control. Yaws Eradication Programme (YEP). Ministry of Health & Family Welfare, Government of India. Available from: http://ncdc.gov.in/index3.asp/sslid=330&subsublinkid=304
- [Google Scholar]
- Eradicating and eliminating infectious diseases: Past, present and future. Indian J Public Health. 2011;55:81-7.
- [Google Scholar]
- Yaws in India: natural history, trends and future prospects. In: Sehgal PN, Banerjee KB, Narain JP, eds. Yaws: prospects and strategies for eradication in India. Delhi: National Institute of Communicable Diseases; 1987. p. :13-21.
- [Google Scholar]
- National Institute of Communicable Disease. Yaws Elimination to Eradication. 2006. Available from: http://nicd.nic.in/index3.asp?sslid=330&subsublinkid=304
- [Google Scholar]
- Resurgence of yaws. A preliminary report from Jagdalpur, Madhya Pradesh, India. Indian J Prev Soc Med. 1976;9:41-6.
- [Google Scholar]
- Single-dose azithromycin versus benzathine benzylpenicillin for treatment of yaws in children in Papua New Guinea: an open-label, non-inferiority, randomized trial. Lancet. 2012;379:342-7.
- [Google Scholar]
- Ministry of Health and Family Welfare, Annual Report 2013-14. Available from: http://mohfw.nic.in/WriteReadData/1892s/chapter1515.pdf
- [Google Scholar]
- Yaws: a second (and maybe last?) chance for eradication. PLoS Negl Trop Dis. 2008;2:e275.
- [Google Scholar]