Translate this page into:
Clinical profile & outcome of H1N1 infected pregnant women in a tertiary care teaching hospital of northern India
Reprint requests: Dr Seema Singhal, Associate Professor, Department of Obstetrics & Gynaecology VMMC & Safdarjang Hospital, New Delhi 110 029, India e-mail: drseemasinghal@gmail.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
H1N1 influenza is a recognized cause of febrile respiratory infection worldwide. There are not many studies to show its impact on pregnancy. In the present study we aimed to assess clinical characteristics, obstetric and perinatal outcome of pregnant women with H1N1 infection.
Methods:
A retrospective observational study was conducted at a tertiary care teaching hospital in New Delhi, India. A total of 24 pregnant women microbiologically positive for H1N1 were included. Maternal characteristics and outcome were recorded. Perinatal outcome which was defined as presence of any of the indicators such as abortion, preterm delivery, intrauterine death and neo natal death was noted.
Results:
The mean age of the study group was 25.2 ± 3 yr with a mean gestational age of 34.9 ± 4.6 wk. Six patients (25%) had associated co-morbidities. Nine patients (37.5%) presented within 48 h of onset of symptoms and 15 (62.5%) reported after 48 h. In 17 (70.83%) patients treatment was delayed by >48 h. ICU admission was needed in 20.8 per cent patients and mortality rates was 8.3 per cent. There were seven cases of adverse perinatal outcome.
Interpretation & conclusions:
The presenting symptoms of pregnant women with H1N1 were similar to that of general population. Acquiring infection in late trimester, late initiation of antiviral treatment and presence of co-morbid illness were high risk factors for developing critical illness. Pregnant women with suspected H1N1 influenza should be started on antiviral therapy at the earliest. This is likely to help reduce the ICU admission rates and mortalities in this group of women.
Keywords
H1N1
influenza
perinatal outcome
pregnant women
H1N1 influenza has been identified as a cause of febrile respiratory infection worldwide. In India, the highest number of cases was reported in 2009 (27,236), followed by 2010 (20,604) and 2012 (5,054 cases). The highest number of swine flu deaths took place in 2011 (1,763), followed by 2009 (981) and 2012 (405)1. However, these statistics do not estimate the overall health impact of influenza on pregnancy.
Pregnancy does not predispose women to an increased risk of acquiring influenza infection. However, pregnant women are at increased risk of morbidity and mortality as compared to women who are not pregnant234. This is due to the changes in their immune systems to accommodate the developing foetus and adaptations in body as a result of the hormonal and physical changes5. Other factors such as family commitments, lack of awareness, and gender discrimination have been identified to cause delay in seeking health care. These factors along with the physiological changes have an impact on outcome of H1N1 infected pregnant women in low income nations6.
There are not enough data in literature especially in developing countries to ascertain the load of illness during pregnancy. The present study was undertaken to assess clinical characteristics, obstetric and perinatal outcome of pregnant women with H1N1 infection.
Material & Methods
A retrospective observational study was conducted at the department of Obstetrics and Gynaecology, Vardhman Mahavir Medical College (VMMC), and Safdarjang Hospital, New Delhi. All pregnant women who had presented with fever or acute respiratory illness and subsequently were tested positive for H1N1 by a pharyngeal swab from January to March 2013 were included in the study. A total of 24 cases were included.
Maternal age, period of gestation, duration between onset of symptoms and presentation to hospital or initiation of treatment were recorded. Pregnant women who only had influenza-like symptoms without signs of respiratory distress, pathological lung sounds, and infiltrates on a chest radiograph were managed as out patient with strict instructions to report if condition deteriorates. On the other hand, women who had fever, non-productive or dry cough, tachypnoea, dyspnoea, wheezing, intercostal retraction, decreased respiratory sounds, hypoxia, acute respiratory distress, and alveolar opacities on a chest radiograph were admitted. All these patients were treated by oral Oseltamivir, 75 mg twice daily for five days. The criteria for starting treatment was either empirical or after confirmation by laboratory tests. The diagnosis was presumed in women who had presented initially with clinical features suggestive of influenza infection and were clinically suspected to be H1N1 positive and were then subjected to laboratory test, however, only confirmed cases were included for analysis in the study. A confirmed case was defined as an acute respiratory illness with laboratory confirmed H1N1 virus infection by real-time PCR. Time of starting of drug was recorded. Patients in whom treatment was started within 48 h of onset of symptoms were grouped as early treatment group and the patients who were given treatment after 48 h were grouped as late treatment group.
The clinical data of all 24 women recruited in study were analysed. The parameters considered for a critical infection were presence of mental confusion, respiratory rate >30 breaths/min, diastolic BP <60, systolic BP <90 mm of Hg, fever higher than 38°C associated with cough and dyspnoea7. Patients were investigated and treated as per the hospital protocol during their course of illness. The course of disease and outcome of five patients who were admitted to intensive care unit (ICU) were studied in detail.
Clinical complications of H1N1 infection such as admission to ICU, endotracheal intubation or death were considered as critical. In patients who delivered, parameters were recorded in the form of mode of onset, duration of labour, mode of delivery and neonatal outcome. Spontaneous abortion, preterm delivery, still birth and neonatal death were considered as indicators of adverse perinatal outcome. Presence of any of the indicators was recorded as adverse perinatal outcome.
To assess the factors associated with critical illness a comparison was made between patients who were not critically ill (Group A) and patients who developed critical illness (Group B). Maternal and perinatal outcome of early and late treatment group was then compared.
The study protocol was approved by the ethics committee of the institution and written consent was obtained from each subject.
Statistical analysis was done using two-sided Fisher's exact test (for continuous variables) and Mann-Whitney test (for non parametric variables). P<0.05 was considered significant.
Results & Discussion
There were 302 (24 pregnant and 278 general population) confirmed cases of H1N1 in the hospital during the study period. Twenty five patients during their illness were admitted in the ICU. There were 15 deaths due to H1N1 illness in the hospital during the study period. Amongst the general patients 7.2 per cent (20/278) patients needed ICU admission and mortality rate was 4.6 per cent (13/278).
Of the 302 patients, 24 were pregnant and were included in the study. Amongst the pregnant women, 20.8 per cent (5/24) were managed on outpatient basis and 79.2 per cent (19/24) required hospitalization. ICU admission was needed in 20.8 per cent (5/24) patients and mortality rate was 8.3 per cent (2/24).
The mean age of the subjects was 25.2 ± 3 yr. The mean gestational age was 34.9 ± 4.6 wk. Twenty (83.3%) patients presented in the 3rd trimester, four (16.7%) in the 2nd trimester. Six (25%) patients had associated co-morbidities like pre-eclampsia, diabetes, bronchial asthma, pulmonary tuberculosis. Nine (37.5%) patients came within 48 h of onset of symptoms, and 15 (62.5%) reported after 48 h of onset of illness. In 17 (70.83%) patients treatment was initiated after 48 h of onset of symptoms. Cough (95.8%) fever (96%), fever and cough (80%), sore throat, breathlessness were the most common symptoms observed. Abdominal symptoms like diarrhoea, nausea and vomiting was seen in only four (16.6%) patients. The presenting symptoms were found to be similar to that of another study8 from the same region where it was found that 88.1 per cent presented with fever and 77.2 per cent presented with fever and cough. Presence of unusual symptoms like diarrhoea, vomiting was low in both the studies. Various physiologic changes that occur during pregnancy make pregnancy a high risk group for complications due to H1N1 infection29. There is a significant fall in oncotic pressure in 3rd trimester in healthy pregnant women, therefore, pregnant women if infected with H1N1, can rapidly develop a haemodynamic imbalance, which acutely affects lung function and facilitates the development of pneumonia, acute pulmonary oedema, and other serious respiratory illnesses1011. Pregnancy also reduces the ability of women to tolerate hypoxic stress, and thus increases risk of maternal and perinatal mortality. All these complications lead to disproportionately increased incidence of hospitalizations and ICU admissions in pregnant women with H1N11011.
To assess the factors associated with critical illness a comparison (Table I) was made between patients who were not critically ill (Group A, n=19) and those who developed critical illness (Group B, n=5).
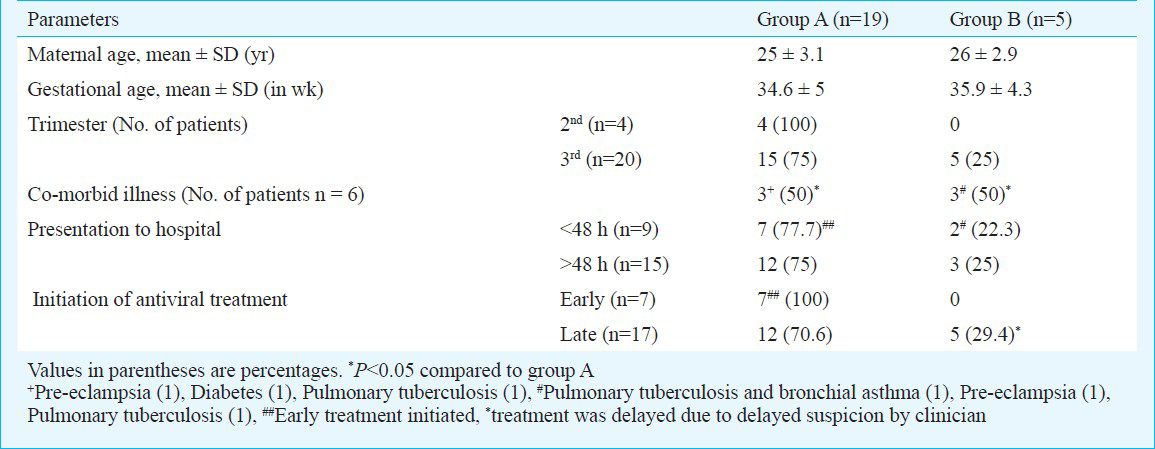
Delayed initiation of antiviral treatment is a high risk factor for development of critical illness29. This fact was supported in the present study (Table I, P<0.05). The reason for the delay was probably late presentation to health care facility. Treatment was delayed in some patients even after reporting to their physicians. The reason for this could be either H1N1 was not suspected or there was reluctance on the part of attending physician to start antivirals for fear of adverse effects on foetus. The CDC recommends immediate antiviral treatment of pregnant women with suspected or confirmed H1N1 influenza, preferably within 48 h after the onset of symptoms12. In a study, patients who received treatment 48 h or more after the onset of symptoms had a risk of ICU admission or death four times greater than patients who received treatment earlier13.
Presence of co-morbid illness is a high risk factor for development of critical illness. Incidence of co-morbid illness as high as 48.4 per cent has been reported9. Pregnancy with co-morbidities further adds to worsening of the outcome. In our study, 50 per cent of women with co-morbidities developed critical illness (Table I, P<0.05). However, small numbers limited the significance of this observation. Other studies have also reported high incidence of co-morbid illness in patients with critical illness314.
Of the 24 women, seven did not deliver (four in 2nd trimester and three in 3rd trimester). Thirteen had vaginal delivery (10 women went into spontaneous labour and 3 were induced) and three were delivered by lower segment caesarean section (LSCS). There were seven cases of adverse perinatal outcome in the present study. Three patients had premature live births, two had neonatal deaths and two had intrauterine deaths. Two maternal deaths occurred during the study period. One patient died before delivery. Maternal and perinatal outcomes of early and late treatment groups were compared. All seven mothers who had adverse perinatal outcome, were from late treatment group. However, significance of adverse perinatal outcome between early and late treatment group could not be drawn. Maternal and foetal outcome was poor in women who had critical illness and those who were in the late treatment group.
In the present study adverse perinatal outcome was seen in 29.1 per cent (7/24) cases and all these women were in their 3rd trimester. Another study reported higher (41.9%, 13/31) incidence of adverse perinatal outcome9.
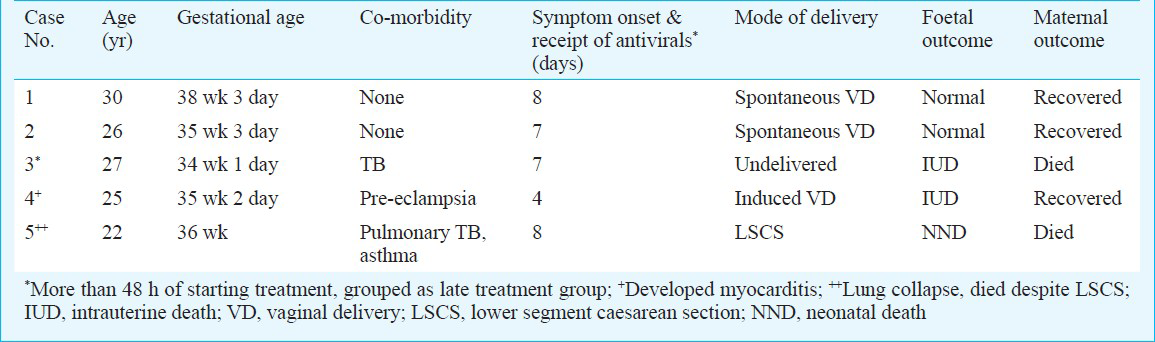
Five patients were admitted to the intensive care unit (ICU) during the course of their illness (Table II). All were in the third trimester, and presented late to the hospital, so the treatment was also initiated late. All of them needed mechanical ventilation. Three of them survived and two died. In present study, ICU admission rate was 20.8 per cent. Similar rates (14%14 and 22.6%9) have been reported in other studies. The mortality rate in the present study was 8.3 per cent; similar rates have been reported by others915. A study from Brazil reported no cases of maternal death16. In this study, 80.7 per cent patients received early antiviral medications16 in contrast to the present study where only 29 per cent patients could receive antiviral treatment within 48 h.
The most important factor that affects the outcome in influenza remains early initiation of treatment during pregnancy. Close attention should be paid to pregnant women in their second and third trimester of pregnancy and to those with co-morbid illness. This is likely to help reduce the ICU admission rates, associated morbidities and mortalities in this group of women.
References
- Ministry of Health and Family Welfare, India. Information on Swine Flu. New Delhi: MOHFW; Available from: http://www.mohfw.nic.in/swineflu.htm
- [Google Scholar]
- Royal College of Obstetricians and Gynaecologists (RCOG). Pandemic H1N1 2009 influenza: Clinical management guidelines for pregnancy. London: RCOG; 2009.
- [Google Scholar]
- Novel influenza A (H1N1) pregnancy Working Group: H1N1 2009 influenza virus infection during pregnancy in the USA. Lancet. 2009;374:451-8.
- [Google Scholar]
- Pandemic (H1N1) 2009 virus infection during pregnancy in South India. Intl J Gynaecol Obstet. 2011;113:32-5.
- [Google Scholar]
- Does delivery improve maternal condition in the respiratory-compromised gravida? Obstet Gynecol. 1998;91:108-11.
- [Google Scholar]
- Emergence of pandemic 2009 influenza A H1N1, India. Indian J Med Res. 2012;135:534-7.
- [Google Scholar]
- Obstetric, clinical, and perinatal implications of H1N1 viral infection during pregnancy. Int J Gynaecol Obstet. 2012;116:214-8.
- [Google Scholar]
- Perinatal and maternal outcomes in critically ill obstetrics patients with pandemic H1N1 influenza A. J Obstet Gynaecol Can. 2010;32:443-52.
- [Google Scholar]
- Novel influenza A (H1N1) virus among gravid admissions. Arch Intern Med. 2010;170:868-73.
- [Google Scholar]
- CDC Health Alert Network (HAN) Info Service Message: Recommendations for early empiric antiviral treatment in persons with suspected influenza who are at increased risk of developing severe disease. 2009. Atlanta, USA: Centers for Disease Control and Prevention; Available from: http://www.cdc.gov/H1N1flu/HAN/101909.htm
- [Google Scholar]
- Pandemic 2009 influenza A (H1N1) virus illness among pregnant women in the United States. JAMA. 2010;303:1517-25.
- [Google Scholar]
- Hospitalized patients with 2009 H1N1 influenza in the United States, April-June 2009. N Engl J Med. 2009;361:1935-44.
- [Google Scholar]
- Severe 2009 H1N1 influenza in pregnant and postpartum women in California. N Engl J Med. 2010;362:27-35.
- [Google Scholar]
- Outcomes for pregnant women infected with the influenza A (H1N1) virus during the 2009 pandemic in Porto Alegre, Brazil. Int J Gynaecol Obstet. 2010;111:217-9.
- [Google Scholar]






