Translate this page into:
Breast cancer pain management - A review of current & novel therapies
Reprint requests: Dr Sushma Bhatnagar, Professor & Head of the Department, Unit of Anaesthesiology (IRCH) Dr BRA IRCH, All India Institute of Medical Sciences, New Delhi 110 029, India e-mail: shumob@yahoo.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Breast cancer is one of the most prevalent cancers amongst women in the world. Unfortunately, even after adequate treatment, some patients experience severe pain either due to disease progression or due to treatment related side effects. The persistent pain causes a negative physical and psychosocial impact on patients’ lives. Current rational pain management is patient-centred and requires a thorough psychological assessment. Usually adequate analgesia is achieved by adopting the WHO's three step analgesic ladder. As the disease progresses, the pain experienced by the patient also increases. This necessitates the administration of opioids and adjuvant analgesics to the breast cancer patients experiencing severe pain. However, opioid use is associated with intolerable side effects like constipation, nausea, vomiting, fear of dependence, and tolerance. Concomitant medications are required to combat these unacceptable side effects. Adjuvant analgesics need to be added to provide adequate and satisfactory analgesia. These factors worsen the psychological state of patients and deteriorate their quality of life. Hence, there is a need to develop therapeutic modalities to provide adequate analgesia with minimum side effects. This review article focuses on the current treatments available for cancer pain management, their limitations, and novel targets and non-pharmacological measures under investigation which have the potential to produce a radical change in pain management measures for the breast cancer patients.
Keywords
Breast cancer
cancer pain
pain management
Introduction
The variation observed in rates of incidence as well as mortality due to breast cancer, is due to a number of contributing factors like age, race, socio-economic status, life style, reproductive history, family history, etc1. According to GLOBOCAN 2008 cancer fact sheet2, incidence of breast cancer was approximately 1.38 million (23% of all neoplasms). Developed countries (except Japan) have a higher incidence (more than 80 for every 100,000 persons) as compared to developing nations (less than 40 for every 100,000 persons)2.
As a consequence of advancements in diagnostic procedures and treatments available, the rate of survival of patients has increased. Hence, it is expected that the population susceptible to develop pain as a complication would increase3. It has been estimated that in developing nations 70 per cent of new breast cancer cases would be seen by 20204. Pain arising in advanced stage of breast cancer can cause emotional suffering and affects quality of life of patients5. As per the estimates of the International Association for the Study of Pain (IASP) the prevalence of pain in breast cancer ranges from 40-89 per cent6. It has been found that persistent pain after surgical treatment is quite common and is higher among young patients, those undergoing radiotherapy and axillary lymph node dissection37, and about 20-50 per cent women are affected by persistent neuropathic pain after their surgical treatment8.
Symptoms
Pain usually does not occur in early breast cancer. A painless lump may be the first symptom. In later stages, pain may occur due to involvement of deeper structures like muscles, ribs, etc., resulting in severe excruciating pain which increases with chest movements. Patients undergoing mastectomy may develop chronic neuropathic pain which may be either phantom breast pain, or intercostobrachial neuralgia (including post-mastectomy pain syndrome), or neuroma pain (including scar pain) or pain due to other nerve injury3. During radiotherapy, there may be active painful skin lesions at the radiation site and later cervical or brachial plexopathy may develop. Involvement of brachial plexus by tumour results in pain and Horner's syndrome, whereas sensory symptoms like paresthesia, numbness, dysesthesia and swelling and weakness of arm occur in radiation induced injury to brachial plexus9. Depending upon the measurement tool used, 2-83 per cent of breast cancer survivors suffer from lymphoedema over the chest or arm10. Breast cancer metastasis commonly involves bones, lungs, brain and liver11, which respectively results in bony pain, pain in hypochondrium, headache and other symptoms in areas of cancer invasion.
There may be sudden exacerbations of pain, termed as breakthrough cancer pain (BTcP). A patient is supposed to have BTcP only when he/she has adequately controlled background cancer pain and is still experiencing transient exacerbations of pain. It can either occur unexpectedly (idiopathic pain) with involuntary acts like coughing, or expectedly (volitional pain) with voluntary acts like walking12. The site and pathophysiology of BTcP is usually the same site as that of background pain13. It is relatively common in advanced disease, painful vertebral metastasis and pain originating from nerve plexuses14.
Aetiology
The aetiology of cancer pain is multi-factorial. It may arise due to (i) cancer itself due to release of inflammatory mediators or due to metastases to distant tissues including bones and neuronal tissue15, and (ii) cancer treatment. Sensory neurons are degenerated after chemotherapy and lead to neuropathic pain. Radiotherapy induced pain arises as a result of microvascular changes and nerve compression15. The main causes for surgery induced pain are damage to the intercostobrachial nerves and neuroma formation3. Estrogen deficiency caused by aromatase inhibitors leads to arthralgias16.
Pain management
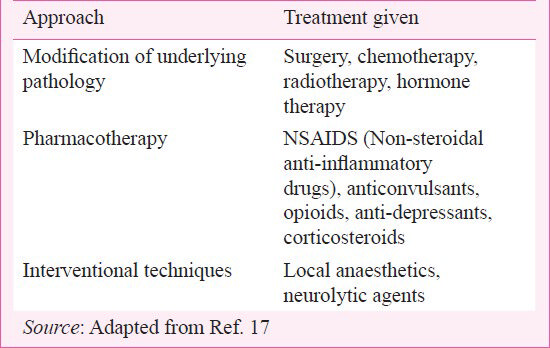
Pain management for cancer patients requires critical pain assessment and thorough patient evaluation including psychological assessment. Depending upon the aetiology of pain, the approach to pain management can be customised for the patient. Various approaches for pain management and treatment are given in Table I17. In about 85-90 per cent of the patients, the pain can be controlled by oral analgesics given according to the World Health Organization (WHO) analgesic ladder, while in others interventions may be required18.
Currently available treatments
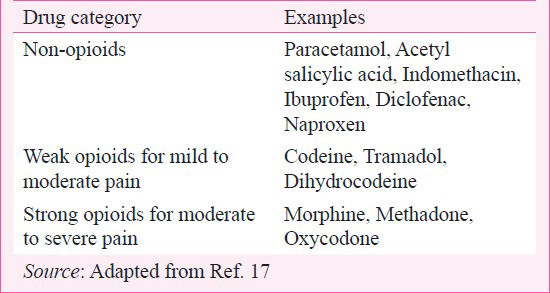
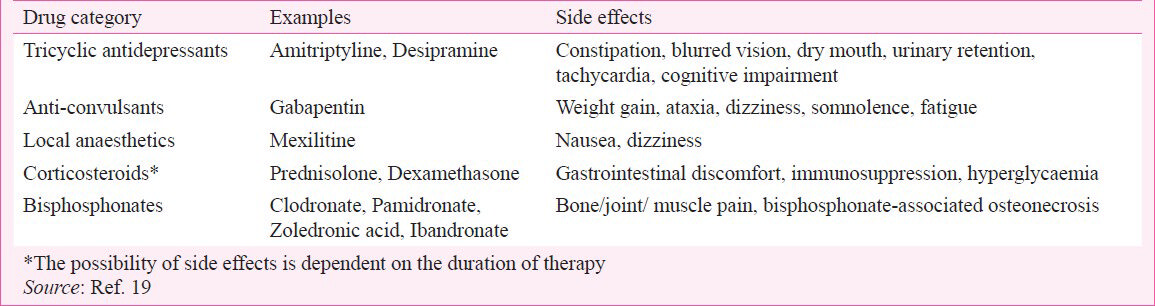
According to WHO17, pharmacotherapy constitutes the main treatment for cancer pain (Table II). The analgesics are used as per five principles: ‘by mouth’, ‘by the clock’, ‘by the ladder’, ‘for the individual’ and ‘attention to detail’. According to the WHO analgesic ladder, the treatment for cancer pain should follow a sequential order (Figure)17. It is initiated by non-opioid drugs, e.g. paracetamol, ibuprofen, which constitute Step I. If adequate analgesia is not achieved, weak opioids like codeine, tramadol should be added. If the pain is still not properly controlled, strong opioids such as morphine, oxycodone can be given (Table II), which constitute Step III of WHO analgesic ladder. Adjuvant medications for pain relief are also provided for different types of pain (Table III)19.

Amongst strong opioids, morphine is the most commonly used. Oral formulations are available as immediate release (IR) morphine and sustained release (SR) morphine sulphate or hydrochloride. Maximum analgesic effect is obtained in 1.5 to 2 h for IR preparations and 3 to 4 h for SR preparations. Usually, opioid therapy is started with IR formulations, though some physicians prefer to start with controlled release formulation, and reserve IR formulations for BTcP20. Steady state of the drug is reached only after five half lives, so dose changes are advised only after 24 h for IR and in 2-3 days for SR formulations20. There is no maximum safe dose for morphine due to absence of ceiling effect to analgesia. Wide individual variations exist to provide same endpoint of pain relief21. The recommended correct dose is the dose which relieves pain adequately without intolerable side effects22.
Opioid rotation is done when inadequate analgesia or intolerable side effects are experienced. The new opioid dose is usually reduced to 66 per cent of the calculated equivalent dose due to incomplete cross-tolerance between the two. Moreover, opioids can be discontinued if appropriate pain relief is achieved by other alternatives like radiation therapy or neurolytic blocks20. Opioids can be discontinued slowly either by decreasing the daily dose by up to 10 to 20 per cent per day or over several weeks to minimize withdrawal symptoms23.
Transdermal fentanyl (TDF) is used for managing patients with stable cancer pain who cannot take oral medications24. Patches are available with a delivery rate of 25, 50, 75 and 100 μg/h, and need to be changed after every 72 h. The dose increase is usually 30-50 per cent, but sometimes 100 per cent (from 25 to 50 μg patch)20.
Adjuvant medications
Adjuvant medications can be added at any stage of the WHO ladder. For management of cancer induced neuropathic pain antidepressants, gabapentinoids (gabapentin, pregabalin), or other anti-epileptic drugs can be used. Primary tricyclic antidepressants (TCA) like amitriptyline are more effective in neuropathic cancer pain, whereas secondary amines like nortriptyline and desipramine which produce lesser analgesia have fewer side effects. Neuroleptics like haloperidol, chlorpromazine, selective serotonin reuptake inhibitor-fluoxetine, and antiepileptic-carbamazepine are also recommended for treating neuropathic cancer pain25.
N-methyl-D-aspartate (NMDA) receptor antagonists like ketamine and amantadine provide an alternative for management of opioid resistant cancer pain25. When pain is not responding to opioids, oral ketamine can be used; only after improvement with a trial of low-dose intra venous ketamine26. However, a systematic review revealed that evidence is insufficient to determine the role of ketamine as an adjuvant to opioids for cancer pain relief27.
The 5 per cent lidocaine patch and 8 per cent capsaicin patch have been found beneficial in treating neuropathic pain. These are safe and well tolerated, and adverse events are attributed to local application of the patch25.
Corticosteroids are also used for managing neuropathic cancer pain. Longer duration of action and least mineralocorticoid effect favour dexamethasone to be frequently used. However, long term use is inhibited by adverse effects like immunosuppression, proximal muscle wasting and endocrine effects25.
Management of breakthrough cancer pain (BTcP)
BTcP can be controlled by treating the underlying aetiology, optimising around the clock medications and using specific medications. In patients with well controlled baseline pain having BTcP episodes, increase in baseline opioid dose results in better pain relief28. For BTcP episodes, about one-sixth (17%) of the daily dose of morphine can be used21.
Faster onset of action is desirable to control BTcP episodes. Effervescent morphine tablets provide faster analgesia as compared to IR oral morphine, hence, can be alternatively used29. Nasal morphine-chitosan spray is rapidly absorbed through nasal mucosa and has plasma profile similar to slow iv administration of morphine30. It provides a faster and convenient alternative than oral morphine for managing episodic pain31.
Transmucosal administration of fentanyl provides rapid onset of action via non-invasive route. Oral transmucosal fentanyl citrate (OTFC) is a fentanyl-impregnated lozenge, available in six dosage strengths (200, 400, 600, 800, 1200 and 1600 μg)29. Absorption rate and bioavailability of OTFC is greater than oral absorption and serum fentanyl levels increase linearly with dose. Intranasal fentanyl spray (INFS) has faster onset of action (at 10 min), attaining peak effect at 12-15 min. It can be self administered, is acceptable to patients with reduced salivary flow and has greater preference than OTFC29. Fentanyl buccal tablet (FBT) is an effervescent drug delivery system employed to augment the rate and extent of fentanyl absorption across the buccal mucosa. Its absolute bioavailability is greater than OTFC. Sublingual fentanyl (SLF) is rapidly absorbed due to high vascularity and permeability of sublingual mucosa. It directly reaches systemic circulation and plasma concentration increases linearly with increase in dose. Ease of administration makes it popular amongst patients29. Fentanyl buccal soluble film (FBSF) is available in strengths of 200-1200 μg. It delivers fentanyl via buccal mucosa, thereby providing fast onset of pain relief, and decrease in pain intensity persists for about 60 min32. All these formulations are more effective in reducing episodic pain. These provide faster analgesia, relieve more episodes of BTcP, are easier to use and are usually well tolerated29.
Management of disorders commonly seen with breast cancer
Brachial plexopathy: Radiotherapy is useful in relieving pain from metastatic plexopathy, whereas surgery provides pain relief in radiation plexopathy, but without any improvement in neurological deficit933. In addition, dorsal column stimulators, transdermal electrical nerve stimulation, neurolysis with omentoplasty are helpful in managing radiation plexopathy. Contrarily, metastatic plexopathy can be managed by dorsal root entry zone procedure, paravertebral nerve blocks, dorsal rhizotomy and contralateral cordotomy34.
Painful bony metastasis: Palliative radiotherapy, namely external beam radiotherapy is useful in patients with painful bony metastasis. Both single (8-10 Gy) and fractionated (20-30 Gy in 5-10 fractions) radiotherapy provide good analgesia35. Bisphosphonates like zoledronic acid, pamidronate, ibandronate, or denosumab (human monoclonal antibody) not only provide relief from bony pain but reduce the risk of skeletal complications and the need of radiotherapy. Rarely, gastrointestinal toxicity, renal toxicity, and osteonecrosis of the jaw may be seen36. Radioisotopes such as samarium153, strontium89 and rhenium186 are also used in patients with painful bony metastases37. These reduce the bony pain over one to six months, but bone marrow suppression is frequent. Therefore, these should be reserved for patients with painful bone metastases not responding to established treatments like radiotherapy, hormone therapy or bisphosphonates38.
Post-mastectomy pain syndrome (PMPS): PMPS can be prevented by multimodal approaches using local anaesthetics with gabapentin and pregabalin39 and with antidepressants like amitriptyline, venlafaxine25. Stellate ganglion block has been found to be useful in some patients to treat PMPS4041.
Lymphoedema: Complex decongestive therapy and exercises like range of motion, resistance and strengthening, compression garments and weight reduction are helpful in decreasing lymphoedema. Therapies like endermologie, flexitouch, deep oscillation, acupuncture, liposuction and autologous stem cell transplant are recent treatment options10.
Brain metastasis: Single metastasis is usually treated by surgery followed by whole brain radiotherapy (WBRT), whereas multiple (2-4) metastases are treated by stereotactic surgery, with or without WBRT42.
Liver metastasis: Liver metastasis is usually treated by chemotherapeutic agents or TACE (Transarterial Chemoembolization)43.
Limitations of pharmacotherapy
Non-steroidal anti-inflammatory drugs (NSAIDS) usually are tolerable and have a few side effects like nausea, vomiting, gastric disturbances, hepatic or renal dysfunction17. These exhibit ceiling effect and should be used with caution in high risk patients including elderly; patients with gastrointestinal disorders, renal and hepatic impairment and/or those receiving other medications44.
Opioid use is associated with many side effects. The most common ones are nausea/vomiting and constipation. Tolerance does not develop to constipation. It necessitates life-long treatment with bulk laxatives, stool softeners, osmotic laxatives and stimulant laxatives. Sedation may occur at the initiation and rapid dose escalation. It can be decreased by reducing the opioid dose, opioid rotation, or using psychosomatic stimulants. Psychomotor performance is normally impaired at the start of opioid therapy, but once a stable dose is reached, it does not result in any impairment even immediately after taking the opioid dose45. Respiratory depression occurs rarely in chronic cancer pain patients receiving opioids regularly. It may occur when pain is relieved suddenly, e.g. non-titration of opioid dose after successful nerve block46. Tolerance develops to analgesic action of opioids when administered for a long time. In order to relieve the pain, the dose has to be increased4546. As a result of these side effects, there may be either under-dosing or early discontinuation of opioids leading to inadequate pain relief45.
Concerns about opioid availability and accessibility have been raised. Various regulations have been imposed for prescribing opioids. Only licensed practitioners have the authority to prescribe opioids. License is required by the pharmacies also to dispense opioids. Extensive regulatory requirements lead to reluctance on the part of pharmacists to dispense opioids47. With the collaborative efforts of the WHO Collaborating Centre at the Pain and Policy Studies Group (PPSG), and the Indian Association of Palliative Care narcotic regulations were eased in India in 1998.
The usefulness of WHO ladder has been questioned by many studies. The addition of weak opioids to NSAIDs is questionable. In one meta-analysis, the addition of weak opioids to NSAIDs resulted in no improvement of analgesia, while another review demonstrated that NSAIDs and weak opioids produce similar analgesia, when given alone or in combination4849. The role of strong opioids as step I analgesic in advanced cancer has also been put forward. A randomized trial compared pain relief in advanced cancer cases when treated either according to the WHO ladder or with strong opioids as a first line treatment50. Patients treated with strong opioids as first line treatment had considerably more relief in pain intensity, greater satisfaction and improvement in general condition as compared to the patients treated as per WHO analgesic ladder.
Non-pharmacological therapies
Apart from the conventional pharmacotherapy, many non-pharmacological measures are available to manage breast cancer pain. The prevalence of complementary or alternative therapies to improve health is increasing. Their usage amongst breast cancer survivors has been found high as compared to the general population and those suffering from other types of cancer51.
With the recognition of objective and subjective component of cancer pain, cognitive behavioural therapy is being adopted by many breast cancer patients for pain relief. It includes various techniques like relaxation training, progressive muscle relaxation, hypnosis, distraction, guided imagery, problem solving, etc52. Pre-surgery hypnotic intervention is supposed to reduce post-surgery pain in patients53. Guided imagery modulates pain and alters transmission and perception of pain stimulus by distracting attention from it54. Moore and Spiegel55 demonstrated in African-American and White women with metastatic breast cancer, that they used this technique to re-connect to the self, manage cancer pain and develop a sense of control over their lives. Individual variations in improvement in pain score by using imagery necessitate the need to customise the intervention given to the patient54. A meta-analysis conducted by Tatrow and Montgomery56 revealed that breast cancer patients receiving various cognitive behavioural therapies experienced lesser pain as compared to control groups.
Thoracic paravertebral nerve block technique reduces post-operative pain and lessens the chances of developing chronic mastectomy pain syndrome57. It helps in pain relief and improves the quality of life of breast cancer patients after surgery when combined with glucocorticoids58.
Novel therapies
Various forms of pharmacological and non-pharmacological treatments are being developed to aid in cancer pain relief. Some of these are described below:
Pharmacological therapies
CB2 agonist : Cannabinoid receptor 2 (CB2) agonist is a novel therapeutic target, which has proved efficacious against neuropathic pain. Low dose of delta-9-tetrahydrocannabinol (THC) produces mild analgesic effects on cancer patients, but higher dose results in side effects in the form of somnolence, dizziness, ataxia, and blurred vision59. Johnson et al60 found in a multicentric trial that tetrahydrocannabinol:cannabidiol (THC:CBD) extract is efficacious for pain relief in patients with advanced cancer pain refractory to opioids. A phase III clinical trial to determine effect of cannabinoid extract (Sativex) in reducing chemotherapy induced neuropathic pain is being conducted (ClinicalTrials.gov #NCT00872144)61.
(ii) Tetrodotoxin: Upregulation of voltage gated sodium (Na+) channels has been seen in metastatic cancers including breast cancer62. Their expression is inhibited by selective Na+ channel blocker - tetrodotoxin, which produces the analgesic effect by blocking action potential propagation or ectopic discharges. A recent trial suggests that tetrodotoxin may alleviate moderate to severe, treatment-resistant cancer pain even for prolonged periods following treatment, with acceptable toxicity63.
(iii) Botulinum toxin: Botulinum toxin has ability to suppress the release of neurotransmitters involved in transmission of pain impulses/nociception i.e. endothelin-1, substance P, and calcitonin gene related peptide (CGRP) and neuropeptide Y64. It has been used to control post-mastectomy pain65 and has potential to reduce cancer induced bone pain64.
(iv) Caffeine: Caffeine is an antagonist of adenosine receptors-A[1], A[2A], A[2B]. It has shown beneficial effects when given as an adjuvant with NSAIDs and opioids66. Clinical trials to establish the efficacy of caffeine as an adjuvant to opioids in reducing pain (ClinicalTrials.gov #NCT00879775)67 and in alleviating post-operative pain after breast surgery are being carried out (ClinicalTrials.gov #NCT00299039)68.
(v) Soy isoflavones: Some studies have shown analgesic effect of soy isoflavones in animal models6970. A clinical trial was being conducted to determine the outcome of soy isoflavones consumption as analgesic after surgery for breast carcinoma (ClinicalTrials.gov #NCT01047774)71.
Non-pharmacological therapies
(i) Gene therapy: Improved understanding of signalling pathways underlying pain generation and transmission, and significant advances in the viral vector designs have led to the development of gene based approach to modulate nociception72. Fink et al73 conducted a phase I clinical trial of NP2, a replication defective herpes simplex virus (HSV) based vector expressing human preproenkephalin (PENK) in cancer pain subjects. The intervention was well tolerated by the subjects. Phase II of this clinical trial for treating intractable pain due to malignancy is currently being carried out (ClinicalTrials.gov #NCT01291901)74.
(ii) Yoga: Yoga has shown positive results on behavioural outcomes like pain, fatigue, depression, mood and quality of life75. Galantino et al76 demonstrated that yoga could reduce joint pain due to aromatase inhibitors in breast cancer survivors. Carson et al75 demonstrated that women with metastatic breast cancer reported improvement in pain when given yoga as intervention. However, the sustainability of pain relief after yoga based intervention needs more investigation.
(iii) Music therapy: Music therapy reduces pain through physiological, psychological and socio-emotional mechanisms. Li et al77 reported that music therapy significantly reduced pain scores in breast cancer patients following mastectomy. Due to the advantage of absence of any adverse effects from music therapy, it can be combined with other interventions for pain relief to obtain maximum benefit. This non-invasive non-pharmacological intervention can be customised according to the patient's cultural background and familiarity; and can prove beneficial in not just reducing cancer induced pain but also to reduce anxiety and depression78.
(iv) Acupuncture: Analgesic activity of acupuncture is attributed to various mechanisms like discharges of polymodal receptors, increase in circulatory levels of opioid peptides, blood flow improvement and mechano-transduction-based responses79. Auricular acupuncture has been found to reduce pain intensity in subjects with neuropathic cancer pain80. Studies have demonstrated analgesic activity of acupuncture and electro-acupuncture in breast cancer survivors experiencing arthralgia due to aromatase inhibitors8182. Clinical trials investigating the role of acupuncture/electro-acupuncture in reducing taxane induced neuropathic pain in breast cancer patients are being carried out (ClinicalTrials.gov # NCT01163682, NCT01050075)8384.
(v) Scrambler therapy: Scrambler therapy is an electro-analgesic technique to regulate pain. Ricci et al85 demonstrated its safety and efficacy in controlling cancer pain in advanced cases. Chronic neuropathic pain was shown to be better relieved by scrambler therapy than standard pharmacotherapy in a pilot study conducted by Marineo et al86. The results of these preliminary studies need to be confirmed via clinical trials to be used in cancer subjects including breast cancer survivors. A phase II study to determine its effect in managing chronic chemotherapy-induced peripheral neuropathy has been conducted87.
Conclusion
The life expectancy of breast cancer patients is increased due to effective treatment options available today. Nonetheless, persistent chronic pain of oncologic origin has depreciated the quality of life in advanced stage breast cancer survivors after treatment. A range of analgesics and adjuvant medications are accessible to the patients. These medicines provide satisfactory analgesia but are allied to a number of side effects. Hence, more effective ways for managing breast cancer pain are needed. However, further studies are needed for the novel therapies and agents to assure fast and adequate pain relief with minimum side effects.
References
- The global breast cancer burden: variations in epidemiology and survival. Clin Breast Cancer. 2005;6:391-401.
- [Google Scholar]
- GLOBOCAN 2008, Cancer Fact Sheet. Breast Cancer Incidence and Mortality Worldwide in 2008. Available from: http://globocan.iarc.fr/factsheets/cancers/breast.asp
- [Google Scholar]
- Neuropathic pain following breast cancer surgery: proposed classification and research update. Pain. 2003;104:1-13.
- [Google Scholar]
- International Association for the Study of Pain, Psychosocial Interventions for Cancer Pain. Available from: http://www.iasp- pain.org/AM/Template.cfm?Section=Home&Template=/CM/ContentDisplay.cfm&ContentID=8703
- [Google Scholar]
- The problem of pain in outpatients with breast cancer. Oncol Nurs Forum. 1995;22:791-7.
- [Google Scholar]
- International Association for the Study of Pain. Epidemiology of Cancer Pain. Available from: http://www.iasppain.org/AM/Template.cfm?Section=Home&Template=/CM/ContentDisplay.cfm&ContentID=7395
- [Google Scholar]
- Prevalence of and factors associated with persistent pain following breast cancer surgery. JAMA. 2009;302:1985-92.
- [Google Scholar]
- Chronic neuropathic pain in women after breast cancer treatment. Pain Manag Nurs. 2009;10:197-205.
- [Google Scholar]
- Brachial plexus lesions in patients with cancer: 100 cases. Neurology. 1981;31:45-50.
- [Google Scholar]
- Breast cancer action. Management of secondary lymphedema related to breast cancer. Can Fam Physician. 2010;56:1277-84.
- [Google Scholar]
- Breast cancer: metastatic patterns and their prognosis. South Med J. 1988;81:1109-12.
- [Google Scholar]
- Science Committee of the Association for Palliative Medicine of Great Britain and Ireland. The management of cancerrelated breakthrough pain: recommendations of a task group of the Science Committee of the Association for Palliative Medicine of Great Britain and Ireland. Eur J Pain. 2009;13:331-8.
- [Google Scholar]
- Breakthrough pain: definition, prevalence and characteristics. Pain. 1990;41:273-81.
- [Google Scholar]
- Breakthrough pain, the pain emergency and incident pain. In: Kopf A, Patel NB, eds. Guide to pain management in low-resource settings. Seattle: International Association for the Study of Pain; 2010. p. :277-82.
- [Google Scholar]
- International Association for the Study of Pain, Mechanisms of Cancer Pain. Available from: http://www.iasp-pain.org/AM/Template.cfm?Section=Fact_Sheets1&Template=/CM/ContentDisplay.cfm&ContentID=7186
- [Google Scholar]
- Patterns and risk factors associated with aromatase inhibitor-related arthralgia among breast cancer survivors. Cancer. 2009;115:3631-9.
- [Google Scholar]
- WHO. Cancer pain relief: with a guide to opioid availability. (2nd ed). Geneva: World Health Organization; 1996.
- [Google Scholar]
- The evolving role of interventional pain management in oncology. J Support Oncol. 2004;2:491-500. 503
- [Google Scholar]
- National Cancer Institute, Pharmacologic Management. Available from: http://www.cancer.gov/cancertopics/pdq/supportivecare/pain/HealthProfessional/Page3#Section_169
- [Google Scholar]
- Pain - Analgesics. In: Downing GM, Wainwright W, eds. Medical care of the dying (4th ed). Victoria, British Columbia Canada: Victoria Hospice Society Learning Centre for Palliative Care; 2006. p. :189-251.
- [Google Scholar]
- Morphine and alternative opioids in cancer pain: the EAPC recommendations. Br J Cancer. 2001;84:587-93.
- [Google Scholar]
- Hospice Education Institute. Morphine. Available from: http://www.hospiceworld.org/book/morphine.htm
- [Google Scholar]
- Pain. In: Yarbro CH, Frogge MH, Goodman M, eds. Cancer symptom management (3rd ed). Sudbury, Massachusetts: Jones and Bartlett; 2004. p. :83-7.
- [Google Scholar]
- Transdermal fentanyl: an updated review of its pharmacological properties and therapeutic efficacy in chronic cancer pain control. Drugs. 2001;61:2289-307.
- [Google Scholar]
- Pharmacological treatment of neuropathic cancer pain: a comprehensive review of the current literature. Pain Pract. 2012;12:219-51.
- [Google Scholar]
- Ketamine in chronic pain management: an evidence-based review. Anesth Analg. 2003;97:1730-9.
- [Google Scholar]
- Ketamine as an adjuvant to opioids for cancer pain. Cochrane Database Syst Rev. 2003;1:CD003351.
- [Google Scholar]
- Optimization of opioid therapy for preventing incident pain associated with bone metastases. J Pain Symptom Manage. 2004;28:505-10.
- [Google Scholar]
- The use of rapid onset opioids for breakthrough cancer pain: the challenge of its dosing. Crit Rev Oncol Hematol. 2011;80:460-5.
- [Google Scholar]
- Pilot study of nasal morphine-chitosan for the relief of breakthrough pain in patients with cancer. J Pain Symptom Manage. 2002;24:598-602.
- [Google Scholar]
- Fentanyl buccal soluble film (FBSF) for breakthrough pain in patients with cancer: a randomized, double-blind, placebo-controlled study. Ann Oncol. 2010;21:1308-14.
- [Google Scholar]
- Diagnosis and management of brachial plexus lesions in cancer patients. Oncology (Williston Park). 1995;9:756-60.
- [Google Scholar]
- Palliative radiotherapy for bone metastases: an ASTRO evidence-based guideline. Int J Radiat Oncol Biol Phys. 2011;79:965-76.
- [Google Scholar]
- Treatment of bone metastases in patients with advanced breast cancer. Breast Care (Basel). 2012;7:92-8.
- [Google Scholar]
- Radionuclide treatment of painful bone metastases in patients with breast cancer: a systematic review. Cancer Treat Rev. 2012;38:164-71.
- [Google Scholar]
- Radioisotopes for metastatic bone pain. Cochrane Database Syst Rev. 2011;7:CD003347.
- [Google Scholar]
- Multimodal analgesia with gabapentin and local anesthetics prevents acute and chronic pain after breast surgery for cancer. Anesth Analg. 2005;101:1427-32.
- [Google Scholar]
- Comparing the effect of stellate ganglion block and gabapentin on the post mastectomy pain syndrome. Rawal Med J. 2008;33:22-5.
- [Google Scholar]
- Fluoroscopic stellate ganglion block for postmastectomy pain: a comparison of the classic anterior approach and the oblique approach. Clin J Pain. 2011;27:207-13.
- [Google Scholar]
- Radiosurgery alone or in combination with whole-brain radiotherapy for brain metastases. J Clin Oncol. 1998;16:3563-9.
- [Google Scholar]
- Liver metastases: neoadjuvant downsizing with transarterial chemoembolization before laser-induced thermotherapy. Radiology. 2003;229:457-64.
- [Google Scholar]
- Analgesic effects of nonsteroidal anti-inflammatory drugs in cancer pain due to somatic or visceral mechanisms. J Pain Symptom Manage. 1999;17:351-6.
- [Google Scholar]
- Problems of opioid availability and accessibility across Europe: ESMO tackles the regulatory causes of intolerable and needless suffering. Ann Oncol. 2006;17:885-7.
- [Google Scholar]
- Efficacy and safety of nonsteroidal antiinflammatory drugs for cancer pain: a meta-analysis. J Clin Oncol. 1994;12:2756-65.
- [Google Scholar]
- Nonsteroidal anti-inflammatory drugs, alone or combined with opioids, for cancer pain: a systematic review. J Clin Oncol. 2004;22:1975-92.
- [Google Scholar]
- Use of strong opioids in advanced cancer pain: a randomized trial. J Pain Symptom Manage. 2004;27:409-16.
- [Google Scholar]
- Complementary and alternative medicine use among women with breast cancer: a systematic review. Clin J Oncol Nurs. 2010;14:E45-55.
- [Google Scholar]
- Nonpharmacological interventions with chronic cancer pain in adults. Cancer Control. 2000;7:157-64.
- [Google Scholar]
- Brief presurgery hypnosis reduces distress and pain in excisional breast biopsy patients. Int J Clin Exp Hypn. 2002;50:17-32.
- [Google Scholar]
- A pilot study to predict success with guided imagery for cancer pain. Pain Manag Nurs. 2003;4:112-23.
- [Google Scholar]
- Uses of guided imagery for pain control by African-American and white women with metastatic breast cancer. Integr Med. 2000;2:115-26.
- [Google Scholar]
- Cognitive behavioral therapy techniques for distress and pain in breast cancer patients: a meta-analysis. J Behav Med. 2006;29:17-27.
- [Google Scholar]
- Paravertebral block: new benefits from an old procedure. Curr Opin Anaesthesiol. 2007;20:316-8.
- [Google Scholar]
- Radiofrequency treatment of the thoracic paravertebral nerve combined with glucocorticoid for refractory neuropathic pain following breast cancer surgery. Pain Physician. 2009;12:E277-83.
- [Google Scholar]
- The analgesic properties of delta-9-tetrahydrocannabinol and codeine. Clin Pharmacol Ther. 1975;18:84-9.
- [Google Scholar]
- Multicenter, double-blind, randomized, placebo-controlled, parallel-group study of the efficacy, safety, and tolerability of THC:CBD extract and THC extract in patients with intractable cancer-related pain. J Pain Symptom Manage. 2010;39:167-79.
- [Google Scholar]
- ClinicalTrials.gov. Sativex for treatment of chemotherapy induced neuropathic pain. Available from: http://clinicaltrials.gov/ct2/show/NCT00872144?term=cannabinoids+and+cancer+pain&rank=2
- [Google Scholar]
- Molecular pharmacology of voltage-gated sodium channel expression in metastatic disease: clinical potential of neonatal Nav1.5 in breast cancer. Eur J Pharmacol. 2009;625:206-19.
- [Google Scholar]
- A multicentre open-label safety and efficacy study of tetrodotoxin for cancer pain. Curr Oncol. 2011;18:e109-16.
- [Google Scholar]
- A novel use of botulinum toxin to ameliorate bone cancer pain. Ann Surg Oncol. 2008;15:1259-60.
- [Google Scholar]
- Botulinum toxin infiltration for pain control after mastectomy and expander reconstruction. Ann Surg. 2004;240:608-13.
- [Google Scholar]
- ClinicalTrials.gov. Efficacy of caffeine injection as an adjuvant to opioid therapy in cancer pain. Available from: http://clinicaltrials.gov/ct2/show/NCT00879775
- [Google Scholar]
- ClinicalTrials.gov. T3AI-Pain after breast surgery. Available from: http://clinicaltrials.gov/ct2/show/NCT00299039
- [Google Scholar]
- Effects of soy diet on inflammation-induced primary and secondary hyperalgesia in rat. Eur J Pain. 2010;14:792-8.
- [Google Scholar]
- Analgesic effects of a soy-containing diet in three murine bone cancer pain models. J Pain. 2004;5:104-10.
- [Google Scholar]
- ClinicalTrials.gov. The Effect of Soy Protein on post-breast cancer surgery pain. Available from: http://clinicaltrials.gov/ct2/show/NCT01047774
- [Google Scholar]
- Gene therapy: a potential approach for cancer pain. Pain Res Treat. 2011;2011:987597.
- [Google Scholar]
- Gene therapy for pain: results of a phase I clinical trial. Ann Neurol. 2011;70:207-12.
- [Google Scholar]
- ClinicalTrial.gov. NP2 Enkephalin for Treatment of Intractable Cancer Pain. Available from: http://clinicaltrials.gov/ct2/show/NCT01291901?term=NCT01291901&rank=1
- [Google Scholar]
- Yoga for women with metastatic breast cancer: results from a pilot study. J Pain Symptom Manage. 2007;33:331-41.
- [Google Scholar]
- A qualitative exploration of the impact of yoga on breast cancer survivors with aromatase inhibitor-associated arthralgias. Explore (NY). 2012;8:40-7.
- [Google Scholar]
- Effects of music therapy on pain among female breast cancer patients after radical mastectomy: results from a randomized controlled trial. Breast Cancer Res Treat. 2011;128:411-9.
- [Google Scholar]
- Effect of music therapy for patients with cancer pain. Int J Biol Med Res. 2010;1:79-81.
- [Google Scholar]
- Randomized, blinded, sham-controlled trial of acupuncture for the management of aromatase inhibitor-associated joint symptoms in women with early-stage breast cancer. J Clin Oncol. 2010;28:1154-60.
- [Google Scholar]
- Analgesic effect of auricular acupuncture for cancer pain: a randomized, blinded, controlled trial. J Clin Oncol. 2003;21:4120-6.
- [Google Scholar]
- Pilot study of acupuncture for the treatment of joint symptoms related to adjuvant aromatase inhibitor therapy in postmenopausal breast cancer patients. J Cancer Surviv. 2007;1:283-91.
- [Google Scholar]
- Feasibility trial of electroacupuncture for aromatase inhibitor--related arthralgia in breast cancer survivors. Integr Cancer Ther. 2009;8:123-9.
- [Google Scholar]
- ClinicalTrials.gov. Acupuncture study for the prevention of taxane induced myalgias and neuropathy. Available from: http://clinicaltrials.gov/ct2/show/NCT01163682?term=acupuncture+and+cancer&recr=Open&cond=breast+cancer&rank=9
- [Google Scholar]
- ClinicalTrials.gov. Acupuncture in treating nerve pain in patients with stage I, stage II, or stage III breast cancer who are receiving paclitaxel. Available from: http://clinicaltrials.gov/ct2/show/NCT01050075?term=acupuncture+and+cancer&cond=breast+cancer&rank=1
- [Google Scholar]
- Safety and efficacy of Scrambler therapy for cancer pain. J Clin Oncol. 2010;28(Suppl):e19591.
- [Google Scholar]
- Scrambler therapy may relieve chronic neuropathic pain more effectively than guideline-based drug management: results of a pilot, randomized, controlled trial. J Pain Symptom Manage. 2012;43:87-95.
- [Google Scholar]
- National Cancer Institute. Phase II Pilot study of electrical stimulation therapy using the MC5-A scrambler in reducing peripheral neuropathy caused by chemotherapy. Available from: http://www.cancer.gov/clinicaltrials/MCV-MCC-12110
- [Google Scholar]






