Translate this page into:
Effect of zoledronic acid on bone mineral density in patients of celiac disease: A prospective, randomized, pilot study
Reprint requests: Dr Sanjay Kumar Bhadada, Associate Professor, Department of Endocrinology, Postgraduate Institute of Medical Education & Research, Chandigarh 160 012, India e-mail: bhadadask@rediffmail.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
The symptoms of celiac disease (CD) are varied and metabolic bone disease (MBD) is less recognized amongst all manifestations in CD patients. Bone disease in CD is attributed to secondary hyperparathyroidism, which in turn is associated with increased bone remodelling. Improvement in bone mineral density (BMD) with gluten free diet (GFD) is known, but the data on efficacy of bisphosphonates in CD patients are limited. Bisphosphonates being a potent inhibitor of bone resorption may be useful in patients with CD having low BMD. The aim of the present investigation was to study the effect of zoledronic acid on BMD in CD patients.
Methods:
A total of 28 CD patients were randomized to receive GFD, calcium and cholecalciferol (group A), and zoledronic acid (group B). Baseline biochemical tests and T-score by dual energy x-ray absorptiometer were done and repeated after 12 months.
Results:
The T-score showed improvement in the control arm (group A) from -3.31 ± 1.46 to -2.12 ± 1.44, a gain of 35.9 per cent (P<0.05) and in drug arm (group B) -2.82 ± 1.27 to -1.06 ± 1.84, registering a gain of 62.4 per cent (P<0.001). However, there was no difference in improvement of T-score in zoledronic acid group as compared to the control group.
Interpretation & conclusions:
Administration of zoledronic acid was not found to be better than GFD alone in increasing BMD in CD patients with low BMD in this pilot study.
Keywords
Bisphosphonates
bone mineral density
celiac disease
osteomalacia
osteoporosis
T- score
zoledronic acid
Celiac disease (CD) occurs in genetically susceptible individuals and is caused by intolerance to gluten, a protein component of wheat1. CD can present atypically, with the predominance of extraintestinal manifestations like iron deficiency anaemia, short stature23, recurrent stomatitis, infertility, metabolic bone disease or it may be detected in a patient on routine screening with other pre-existing autoimmune disease4.
CD affects almost all organ systems including skeletal system. The spectrum of metabolic bone disease (MBD) in patients with CD includes pain in bones, rickets/osteomalacia, osteopenia, osteoporosis and rarely, pathological fractures. At diagnosis, the prevalence of osteopenia and osteoporosis in CD varies widely from 36 to 100 per cent and 27 to 73 per cent, respectively5. However, the prevalence of fractures in patients with CD (low bone mineral density, BMD) is controversial. Various case control studies and population based surveys have presented contrasting evidence about the risk for fractures in CD patients678910.
Bone disease in CD is attributed to malabsorption and secondary hyperparathyroidism, which results in reduced bone mass, alteration in bone quality and increased risk of fractures1112. Bisphosphonates are most commonly used for the prevention and treatment of all forms of osteoporosis13. Bisphosphonates have been found to be useful in post-menopausal osteoporosis and secondary hyperparathyroidism, but it is not clear whether bisphosphonates are useful in younger CD patients with low BMD1415. We hypothesized that bisphosphonates being a potent inhibitor of bone resorption and increased bone remodelling, may be useful in CD patients with low BMD. The aim was to study the effect of zoledronic acid on BMD in CD patients as compared to those on standard treatment protocol.
Material & Methods
Subjects: This randomized, prospective pilot study was carried out between April 2008 and December 2009 in the Departments of Endocrinology and Gastroenterology of Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh. The study was approved by the Institute's Ethics Committee and a written consent was obtained from each participant. Newly diagnosed CD patients aged ≥18 yr were enrolled and followed prospectively for one year. Patients with symptoms suggestive of CD were tested for IgA anti-tissue transglutaminase antibody (tTGAb). Those positive for tTGAb were subjected to endoscopy; mucosal details in the descending part of the duodenum were recorded, and 2-4 biopsies were taken. Histological interpretation was done by an experienced pathologist as per modified Marsh classification16. The diagnosis of CD was based on the presence of elevated IgA anti-tissue transglutaminase antibody (tTGAb) and duodenal biopsy suggestive of villous atrophy.
All CD patients with low BMD (T score <-1.0) were included. Postmenopausal women, pregnant women, patients taking drugs (currently or within last one year viz. steroids, anticonvulsants, anticoagulants, calcium supplements) and having diseases (chronic liver disease, chronic kidney disease, thyrotoxicosis, other malabsorptive disorders) known to affect BMD, smokers and persons consuming alcohol (≥3 drinks/day) were excluded.
Study design and randomization: Fifty subjects with proven CD were screened, of whom 16 were excluded for various reasons and the remaining 34 gave the consent to participate in the study. These subjects underwent BMD measurements at lumbar spine and those with low BMD (T<-1.0, 28 subjects) were divided into two groups (group A and B) through random allocation software (Figure). Concealment of allocation was done. The patients in group A were given calcium supplements 1000 mg/day of calcium carbonate, injection cholecalciferol 0.6 million units [if 25(OH)D <20 ng/ml)] along with gluten free diet (GFD). The group B in addition also received 4 mg zoledronic acid, administered intravenous in 100 ml of normal saline over 15-30 min. Flu-like symptoms were explained to the subjects and were advised to take paracetamol, if necessary. Patients were observed over a period of 12 wk for any acute/ sub acute side effects with zoledronic acid.
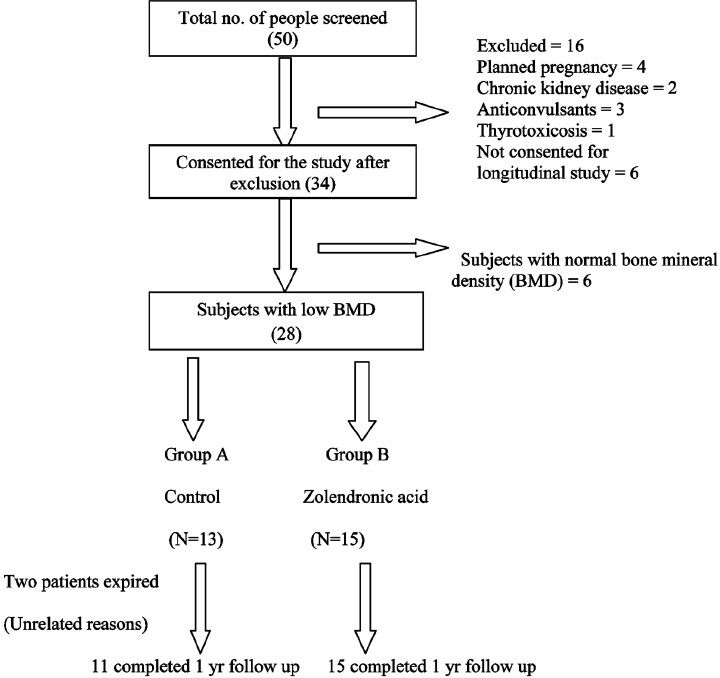
- Flow chart of randomization of study subjects.
Measurements: A detailed history was taken and physical examination was performed. The baseline investigations included haemogram, liver and renal function tests, 25(OH)D, and iPTH. 25-hydroxy vitamin D [25(OH)D] and intact parathyroid hormone (iPTH) were estimated by radioimmunoassay using Diasorin kits (DiaSorin Inc. Stillwater, Minnesota, USA). IgA tTG was done by enzyme linked immunosorbent assay, (D-tek, Blue Well, Belgium). BMD was estimated on a Norland dual energy X-ray absorptiometer (DXA) at baseline and it was repeated one year later, in similar conditions, at lumbar spine. Daily calibrations of BMD measurement were done using the phantom. The CV of DXA at lumbar spine was 0.9 per cent and inter-measurement variability was 0.35 per cent. A change in BMD should be more than 3 per cent to be able to detect appreciable change.
Outcomes: The change in BMD with zolendronic acid as compared to standard treatment group in CD patients was assessed after one year.
Statistical analysis: The statistical analysis was carried out using Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, version 13.0 for Windows). All quantitative variables were estimated using measures of central location (mean, median) and measures of dispersion (standard deviation). Normality of data was checked by measures of Kolmogorov Smirnov tests of normality. For normally distributed data means were compared using Student's t-test for the two groups. For skewed data, Mann-Whitney test was applied. Qualitative or categorical variables were described as frequencies and proportions. Proportions were compared using Chi square or Fisher's exact test whichever was applicable. To see correlation between different variables, Pearson correlation coefficient and Spearman's correlation coefficient were calculated. All statistical tests were two-sided and performed at a significance level of α=0.05. Increase in bone mineral density from baseline to one year was compared using Wilcoxan signed rank test (a non-parametric version of paired t test). For analyzing the data, Chi square test was applied to find out statistical significance between the various categorical variables and BMD. Kruskal Wallis test was applied for continuous data not normally distributed. ANOVA was used to compare continuous data that is normally distributed and Post-hoc analysis was done by Bonferroni. Multivariate regression analysis was applied taking improvement in BMD T-score as a dependent variable and other parameters as independent variables.
Results
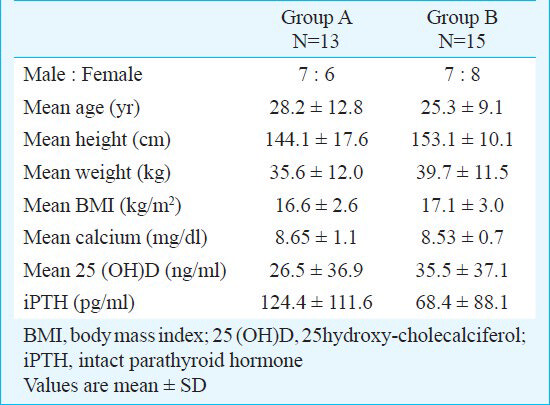
Twenty eight patients (82%) had low BMD (T score <-1) which included osteoporosis and osteopenia in 14 (41%) subjects each. These subjects were further randomized to group A (control arm, n=13) and group B (drug arm, n=15). Two subjects in group A expired because of unrelated reason during follow up and 26 subjects completed the study. Mean lag time between onset of symptoms and diagnosis of CD was 3.76 yr (range 1-10 yr). The baseline characteristics of patients in groups A and B are shown in Table I and histopathological findings on duodenal biopsy revealed Marsh type 1 in one patient, type 2 in seven patients (20.6%), type 3 a in five patients (14.7%), type 3 b in 20 patients (58.8%) and type 3 c in one patient.
Diarrhoea was the most common presenting manifestation (n=27, 79.4%), and it was the chief complaint in 21 (61.7%) patients. Short stature was present in 13 patients (38.2%). Three females (8.8%) presented with symptoms of menstrual irregularities, and secondary infertility and two males had hypogonadism. One patient presented with weight loss and poor weight gain was the presenting manifestation in 13 patients (38.2%). One patient was detected to have CD during family screening and found to have short stature.
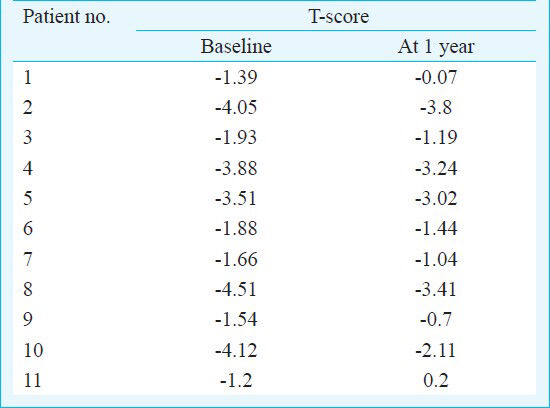
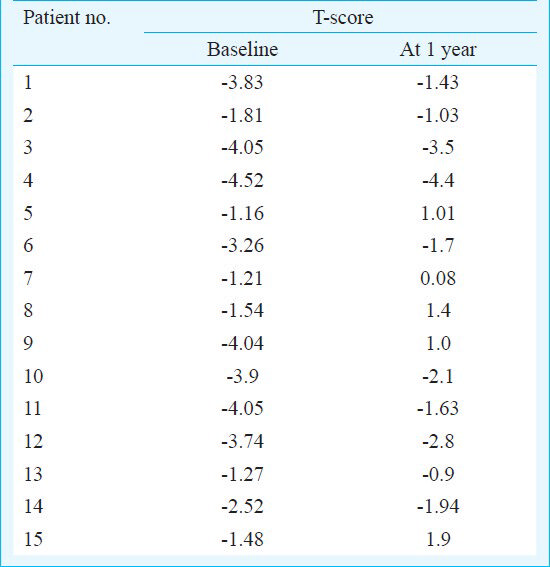
Effect of zoledronic acid: The T-score showed improvement in the control arm from -3.31 ± 1.46 to -2.12 ± 1.44, a gain of 35.9 per cent (P<0.05) (changes in individual patient's T-score are shown in Table II), and in drug arm -2.82 ± 1.27 to -1.06 ± 1.84, a gain of 62.4 per cent (P<0.001) (changes in individual patient's T-score are shown in Table III). However, no significant difference was observed on comparing the improvement in T-score between the two groups. Multivariate regression analysis revealed that only lag duration of symptoms (P=0.047) predicted the improvement in BMD T-score; but age, biochemical parameters like calcium, phosphorus, 25(OH)D3, iPTH, tTG IgA levels and initial BMD T-score did not achieve statistical significance. Fever was observed in eight patients in the zoledronic acid group within the first 3 days of administration and was managed with oral paracetamol. Tetany was observed in one patient, as he missed his calcium tablets but improved with calcium and vitamin D supplements.
Discussion
In this pilot study, a high prevalence of low BMD was seen in adult patients with CD. There was a significant improvement in BMD in both the groups. The rise in BMD was higher in the drug arm compared to control group but did not achieve statistical significance.
Diarrhoea was the most common presenting manifestation (79.4%), followed by short stature (38.2%) and poor weight gain (38.2%). Other less common presentations were amenorrhoea, oligomenorrhoea, recurrent abortions (8.8%), secondary infertility and hypogonadism. Fragility fractures, dermatitis herpetiformis and diabetes mellitus were not found in any of the patients.
Low BMD is a well known consequence of CD7, MBD can be found in symptomatic as well as in asymptomatic CD patient. In the present study, the prevalence of low BMD including osteopenia and osteoporosis as measured at spine was high and was consistent with published literature14. The specific indications for treatment of osteoporosis in patients with CD are fragility fracture and low BMD with an increased risk of fracture. GFD alone has been shown to cause significant improvement in BMD and showed results similar to those achieved by bisphosphonates in the treatment of post-menopausal osteoporosis, with a reduction in bone remodelling1819. GFD is also associated with reduction in PTH levels, improvement in vitamin D levels and other biochemical parameters in CD patients2021.
The important contributing factor for low BMD in CD is secondary hyperparathyroidism which can be tackled by bisphosphonates6 and presently, bisphosphonates have been the most commonly used drug for prevention and treatment of osteoporosis13. Zoledronic acid has been shown to be efficacious in reducing vertebral, nonvertebral and hip fractures in postmenopausal women, including a few with CD13. However, there are no systematic data to assess the anti-osteoporotic efficacy of bisphosphonates in CD patients. Recently, Widjaja et al22 have reported improvement in T and Z-score in a single patient of CD with osteoporosis after 18 months of oral alendronate (dose of 10 mg/day). Zoledronic acid was chosen over other bisphosphonates in the present study because of its potency and long half life, thus, ensuring compliance. Parenteral route was preferred to circumvent the issue of oral absorption in CD.
The optimal timing for BMD measurements in CD remains to be established, but an initial measurement at the time of diagnosis, followed by repeat measurement 12 months later can detect patients with persistent osteopenia23. In the present study, there was a significant improvement in clinical, biochemical parameters and T-score after 12 months of GFD, calcium and vitamin D supplementation in CD patients in both the groups. The significant improvement in BMD within one year in our patients could be attributed to relatively young age of the patients, early diagnosis of CD, proper compliance, adherence to gluten free diet and adequate supplementation with vitamin D and calcium. However, despite the significant gain in BMD on treatment with GFD, there was residual osteopenia and osteoporosis (9 patients) at the end of one year. Various studies182021 have shown that the there is reversible component to the osteopenia present at the time of diagnosis of the CD which can be improved with GFD as observed in our study. The maximum increase occurs in the first year (average of 5%), but the final BMD remains below average, with a final Z score of approximately -1.0 for the spine24.
One of the limitations of the present study was a small number of subjects. Secondly, in this younger population group, improvement in BMD after zoledronic acid could have been depicted in terms of Z-score. We were unable to have Z score, as normative data for the Z-score of Asian Indian children and adolescents have not been established. It would be worthwhile to plan a long term study to see the effect of early administration of zoledronic acid on peak bone mass in young CD patients. The effect of zoledronic acid on biochemical markers of bone turnover could have been assessed, though we did not measure these. The risk of fracture is the critical endpoint for interventional studies in MBD; hence studies of sufficient duration and of adequate power to demonstrate outcomes in terms of fracture should be conducted.
In conclusion, GFD alone significantly improves the BMD in CD patients. Administration of zoledronic acid was not significantly better than GFD alone in increasing BMD in CD patients with low BMD.
References
- Does every short stature child need screening for celiac disease? J Gastroenterol Hepatol. 2008;23:353-6.
- [Google Scholar]
- Changing scenario in aetiological profile of short stature in India-growing importance of celiac disease: a study from tertiary care centre. Indian J Pediatr. 2011;78:41-4.
- [Google Scholar]
- Prevalence and clinical profile of celiac disease in type 1 diabetes mellitus in north India. J Gastroenterol Hepatol. 2011;26:378-81.
- [Google Scholar]
- Fracture risk in patients with celiac disease, Crohn's disease, and ulcerative colitis: a nationwide follow-up study of 16,416 patients in Denmark. Am J Epidemiol. 2002;156:1-10.
- [Google Scholar]
- Osteoporosis in a north american adult population with celiac disease. Am J Gastroenterol. 2001;96:112-9.
- [Google Scholar]
- Risk of fractures in celiac disease patients: a cross-sectional, case-control study. Am J Gastroenterol. 2000;95:183-9.
- [Google Scholar]
- Fracture experience of patients with coeliac disease: a population based survey. Gut. 2003;52:518-22.
- [Google Scholar]
- Coeliac disease and the risk of fractures - a general population-based cohort study. Aliment Pharmacol Ther. 2007;25:273-85.
- [Google Scholar]
- Prevalence and predictors of abnormal mineral bone metabolism in recently diagnosed adult celiac patients. Indian J Gastroenterol. 2012;31:165-70.
- [Google Scholar]
- Bone loss in celiac disease is related to secondary hyperparathyroidism. J Bone Miner Res. 1999;14:652-7.
- [Google Scholar]
- Once-yearly zolendronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356:809-22.
- [Google Scholar]
- Long-term use of bisphosphonates in osteoporosis. J Clin Endocrinol Metab. 2010;95:1555-65.
- [Google Scholar]
- The histopathology of celiac disease: time for a standardized report scheme for pathologists. Eur J Gastroenterol Hepatol. 1999;11:1185-94.
- [Google Scholar]
- Low bone mineral density in adult patients with coeliac disease. Endokrynologia Polska. 2012;63:270-6.
- [Google Scholar]
- Effect of treatment on bone mass, mineral metabolism and body composition in untreated celiac disease patients. Am J Gastroenterol. 1997;92:313-8.
- [Google Scholar]
- Bone recovery after gluten-free diet: a 5-year follow-up study. Bone. 1999;25:355-60.
- [Google Scholar]
- The effects of 1- year gluten withdrawal on bone mass, bone metabolism and nutritional status in newly-diagnosed adult celiac disease patients. Aliment Pharmacol Ther. 2000;14:35-43.
- [Google Scholar]
- Role of alendronate in managing osteoporosis in celiac disease - illustrative case report. Gastroenterol Res. 2011;4:26-9.
- [Google Scholar]
- Guidelines for osteoporosis in inflammatory bowel disease and coeliac disease. BSG Guidelines Gastroenterol. 2007;14:1-16.
- [Google Scholar]
- Should patients with coeliac disease have their bone mineral density measured? Eur J Gastroenterol Hepatol. 2005;17:1065-70.
- [Google Scholar]






