Translate this page into:
The role of urinary fractionated metanephrines in the diagnosis of phaeochromocytoma
Reprint requests: Dr Simon Rajaratnam, Professor, Department of Endocrinology, Diabetes & Metabolism Christian Medical College, Ida Scudder Road, Vellore 632 004, India e-mail: simonrajaratnam@yahoo.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Plasma and urinary metanephrines are used as screening tests for the diagnosis of phaeochromocytoma. The recommended cut-off levels are not standardized. This study was conducted to identify a cut-off level for 24 h urinary fractionated metanephrines viz. metanephrine (uMN) and normetanephrine (uNMN) using enzyme immunoassay for the diagnosis of phaeochromocytoma.
Methods:
Consecutive patients suspected to have phaeochromocytoma were included in the study. uMN and uNMN in 24 h urinary sample were measured using a commercial ELISA kit.
Results:
Overall, 72 patients were included over a period of 18 months. Twenty patients had histopathologically confirmed phaeochromocytoma and in 52 patients phaeochromocytoma was ruled out. Using the upper limit of normal stated by the assay manufacturer as the cut-off, uMN >350 μg/day had a low sensitivity and uNMN >600 μg/day had a poor specificity. By increasing the cut-off value of uNMN to twice the upper limit, specificity increased significantly without much loss in sensitivity. Combining uMN and uNMN using a cut-off twice the upper limit improved the diagnostic performance - sensitivity (95%); specificity (92.3%); positive predictive value (PPV - 82.6%); negative predictive value (NPV - 98%). In subsets of patients with a variable pretest probability for phaeochromocytoma, the PPV correlates well with the occurred of these tumors decreased, while the NPV remained at 100 per cent.
Interpretation & conclusions:
ELISA is a simple and reliable method for measuring uMN and uNMN. The test has a good NPV and can be used as an initial screening test for ruling out phaeochromocytoma. Each hospital will have to define the cut-off value for the assay being used, choosing a proper control population.
Keywords
Adrenal tumour
catecholamines
ELISA
metanephrines
phaeochromocytoma
Screening for phaeochromocytoma is an essential part of the aetiological workup for secondary hypertension. Traditionally, urinary vanillyl mandelic acid (VMA) was used to diagnose phaeochromocytoma. However, it has a low sensitivity (60-70%)1. Later, catecholamines measurement in plasma (PCAT) and urine (UCAT) emerged as useful tests. The sensitivity of catecholamines test is limited by their episodic release from the tumour cells. The reported sensitivity ranges from 76-82 per cent for PCAT and 71-86 per cent for UCAT. The specificity ranges from 81-100 per cent for PCAT and 88-99 per cent for UCAT2.
Metanephrines are ortho-methylated metabolites of catecholamines. These are secreted continuously from the tumour cells, independent of the intermittent release of catecholamines3. The metanephrines are later metabolized by conjugation, primarily in the hepatomesentric organs4. Plasma metanephrines (pMN) are measured in the free form whereas urinary metanephrines (uMN) represent predominantly the conjugated form. Hence compared to pMN, uMN is less specific. Studies have proved that plasma free metanephrines have a sensitivity of 96-100 per cent and specificity of 85-100 per cent superior to that of uMN which has a sensitivity of 93-99.6 per cent and specificity of 71-77 per cent5.
Previous, methods using colorimetry or spectrophotometry as total MET (metanephrine + normetanephrines) which includes a combined measurement of metanephrine (MN) and normetanephrine (NMN). These methods were superseded by liquid chromatographic assays (LC) that allow individual measurement of MN and NMN. The cost involved and the need for special instruments like mass spectrometry (MS) for such assays preclude their routine clinical use. Immunoassays are now available for the measurement of metanephrines and a few studies have shown that the enzyme immunoassay compares well with HPLC measurement and is a viable alternative to HPLC assays6–8. These assays are relatively simple and are readily available in most clinical laboratories9. There is no general agreement regarding the cut-off level of urinary metanephrines for the diagnosis of phaeochromocytoma. The commonly used cut-off levels are from individual institutions which use highly sensitive HPLC assays10. The aim of the present study was to establish thresholds for urinary metanephrine (uMN) and normetanephrine (uNMN) with optimal sensitivity and specificity for the diagnosis of phaeochromocytoma, using a commercially available enzyme immunoassay.
Material & Methods
Subjects: This study was performed from June 2008 to February 2010 in the Department of Endocrinology, Diabetes & Metabolism, Christian Medical College, Vellore, Tamil Nadu. Consecutive patients attending the outpatient clinic who were suspected to have a phaeochromocytoma, were included in the study. The clinical criteria for suspecting phaeochromocytoma were (i) referral as phaeochromocytoma or, (ii) age at onset of hypertension <40 yr or, (iii) paroxysmal symptoms or, (iv) resistant hypertension or, (v) adrenal mass with or without hypertension. All patients underwent 24 h urine collection for estimation of uMN and uNMN. Phaeochromocytoma was ruled out if imaging (ultrasonography/computed tomography of the abdomen and MIBG meta-idobenzylguanidine scintigraphy) was negative or if the surgically resected adrenal mass was not a phaeochromocytoma. The gold standard for confirmation of phaeochromocytoma was histopathology. All these patients were seen in a multidisciplinary clinic involving endocrinologists, nuclear medicine specialists and endocrine surgeons. Histopathology was examined by a single pathologist.
Sample collection and assay: Patients collected 24 h urine sample in containers with 15 ml of 6 M HCl, as a preservative. The volumes were measured and five ml of the urine sample was stored at -20°C until assayed. uMN and uNMN were analysed using a competitive enzyme immune assay with a commercial ELISA kit (LDN GmbH & Co. KG, Nordhorn) using microtiter plates. The analytical sensitivity of the assay specified by the manufacturer was five ng/ml for MN and 13 ng/ml for NMN. The cross reactivity of substances with similar chemical structure like catecholamines, dopamine and VMA was <0.1 per cent. Control, supplied by the manufacturer was run for each assay. The coefficients of variation for metanephrine at 100 ng/ml was 13.3 per cent and 300 ng/ml was 12.3 per cent; normetanephrine at 300 ng/ml was 12.6 per cent and 800 ng/ml was 11.5 per cent. The normal values as stated by the manufacturer were - uMN <350 μg/day and uNMN < 600 μg/day.
Statistical analysis: The quantitative data are expressed as mean ± SD or median (range). To compare the continuous variables between two independent groups which were normally distributed, the two sample t test was used and for skewed distribution, the Mann-Whitney U test was used. Sensitivity and specificity of the upper limit were calculated as given by the manufacturer. However, the reference range given by the manufacturer was based on normal ranges derived from normotensive volunteers which is known to result in excessive false positive testing. From previous studies, it is understood that the 95th percentiles in individuals being tested for pheochromocytoma as part of routine clinical practice (but who do not have the neoplasm) are approximately 50-70 per cent higher than those of normal volunteers10. Hence, the general recommendation is to consider a positive test to be a two-fold elevation above the upper limit of normal. So twice the upper limit of reference range was considered as a diagnostic cut-off. ROC (receiver operating characteristics) curves were constructed and the areas under the ROC curves (AUCROC) were calculated. The curves were employed to identify optimal diagnostic thresholds. Statistical analyses were performed with the commercially available software package (SPSS for Windows, version 10.0, SPSS, Inc., Chicago, IL). P<0.05 was considered statistically significant.
Results
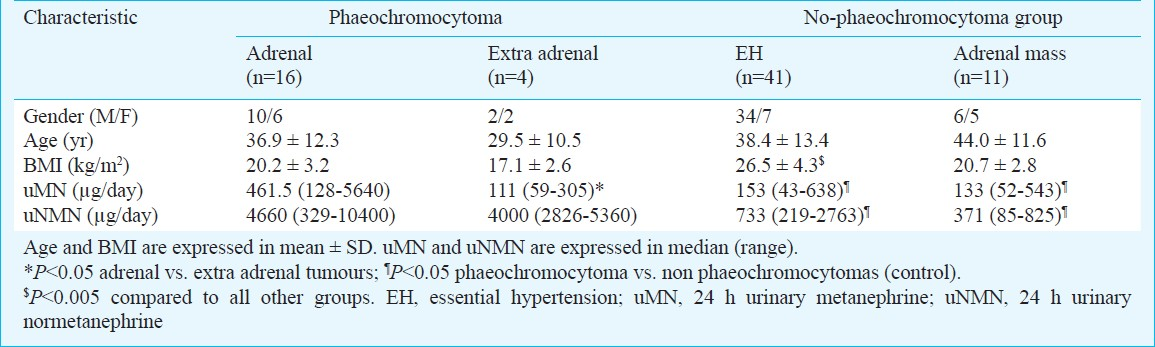
Of the 72 patients (52 men and 20 women), nine were referred as phaeochromocytoma patients, two were on follow up for metastatic phaeochromocytoma and one patient had von Hippel Lindau disease. These 12 patients had histopathologically confirmed phaeochromocytomas. In the remaining 60 patients phaeochromocytoma screening was done for the following reasons: young hypertensives (n=18), resistant hypertension (n=11), hypertension with paroxysmal symptoms (n=16), adrenal mass with hypertension (n=11) and adrenal mass without hypertension (n=4). Among the 45 patients who presented with hypertension, four were diagnosed to have phaeochromocytoma. The remaining 41 hypertensive patients with normal biochemistry, sonographically normal kidneys and renal arteries, negative abdominal imaging and negative MIBG were labelled as essential hypertension (EH). Among 15 patients who had adrenal masses, four with hypertension had histopathologically confirmed phaeochromocytoma. In the phaeochromocytoma group, 16 had adrenal tumours and four had extra-adrenal tumours. Patients with other types of adrenal masses (n=11) and with EH (n=41) formed the no-phaeochromocytoma group.
Clinical profile: The mean age of patients with phaeochromocytoma was not statistically different from that of the no-phaeochromocytoma group. There was a male preponderance in both groups. Patients with EH had a significantly higher BMI compared to the patients with phaeochromocytoma. The uMN levels were 3.5 fold (P=0.005) and uNMN levels were 6.5 fold higher (P< 0.005) in the phaeochromocytoma group compared to no-phaeochromocytoma group. It was observed that extra-adrenal phaeochromocytomas had significantly higher uNMN levels compared to those with adrenal phaeochromocytomas (P<0.05). The uMN level was not different from that of the no-phaeochromocytoma group.
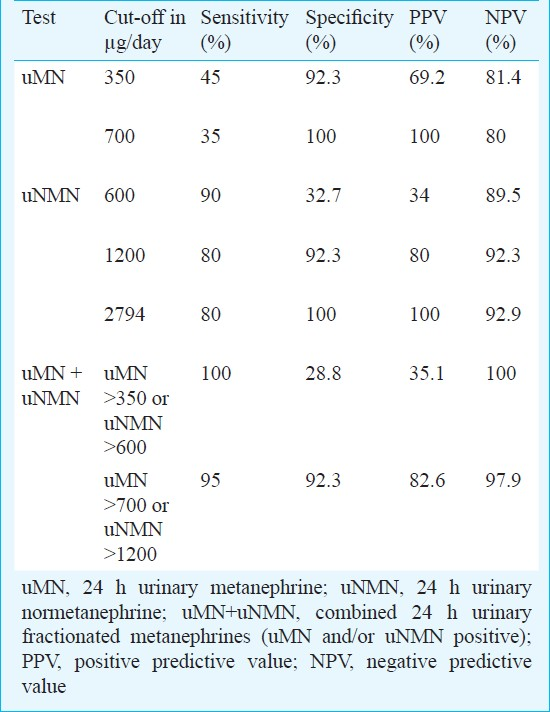
Cut-off for diagnosis of phaeochromocytoma: Using the assay manufacturer's upper limit of normal for uMN >350 μg/day, 11 of the 20 patients with phaeochromocytoma were missed (sensitivity of 45%) but the false positive rate was low (specificity of 92.3%). If the cut-off value was increased to twice the upper limit i.e. >700 μg/day, there were no false positives but the sensitivity dropped to 35 per cent (Fig. 1). No cut-off with better sensitivity and specificity was identified by ROC curve. Similarly, the sensitivity and specificity for uNMN using manufacturer's upper limit of normal >600 μg/day was 90 and 32.7 per cent, respectively. Increasing the cut-off to twice this upper limit i.e. >1200 μg/day, increased the specificity to 92.3 per cent with some loss in sensitivity to 80 per cent (Fig. 1). The AUCROC for uMN was 0.722 (0.579-0.864) and for uNMN was 0.870 (0.748-0.992). Using the ROC curve (Fig. 2), a cut-off value of 2794 μg/day resulted in 100 per cent specificity without further decrease in sensitivity.
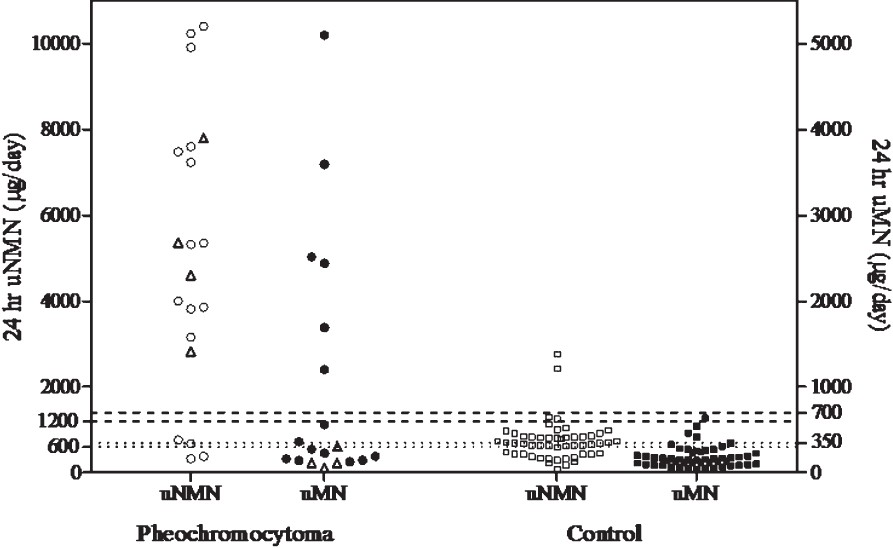
- Cut-off values for 24 h urinary metanephrine (μMN) and normetanephrine (μNMN) in μg/day. The dotted lines represent the cut-off values defined by the upper limit of normal as stated by the assay manufacturer and the broken lines twice the upper limit. In the phaeochromocytoma group, circles (O) and triangles (Δ), adrenal and extra-adrenal tumour, respectively. (□), urinary normetanephrine levels in controls. (■), urinary metanephrine levels in controls.
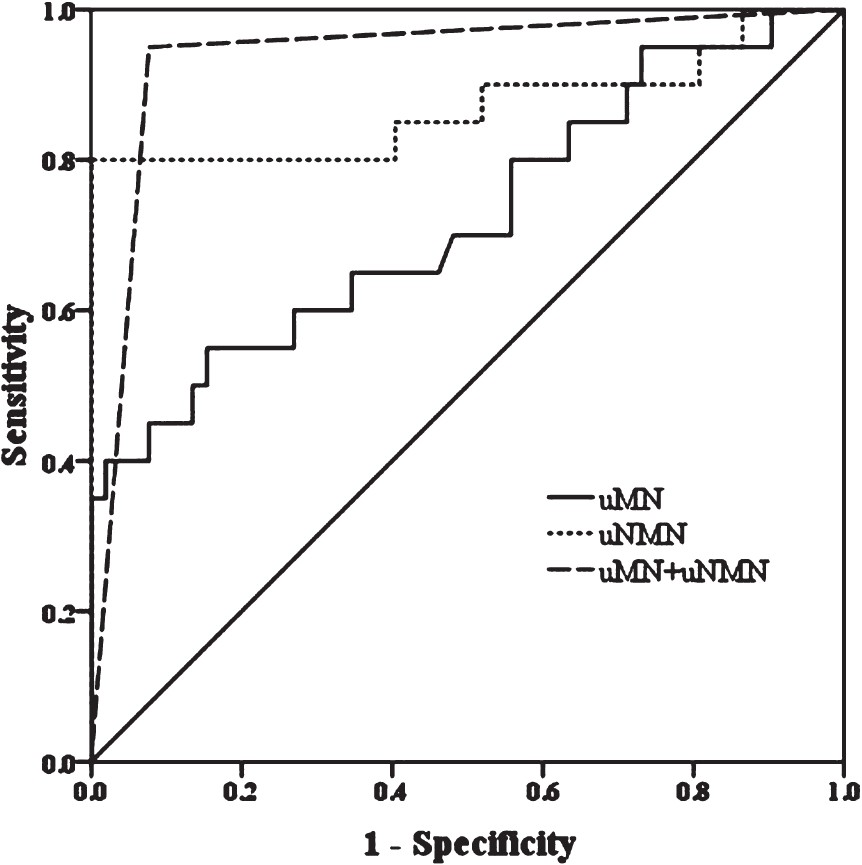
- ROC curve for the 24 h urinary metanephrine (uMN), normetanephrine (μNMN) and a combination of both (μMN+μNMN).
When uMN and uNMN (uMN+uNMN) were combined i.e. uMN > 700 μg/day and/or uNMN >1200 μg/day, the sensitivity improved to 95 per cent and specificity to 92.3 per cent. The positive (PPV) and negative predictive values (NPV) were 82.6 and 98 per cent, respectively. The AUCROC was 0.937 (0.867-1.006) which was better than that of uMN and uNMN separately (Fig. 2). Table II summarises the performance characteristics of the test using different cut-off values for either or both parameters. We divided our study population into four subsets depending on their pretest probability of diagnosing pheochromocytoma. For each of these subsets, we calculated the proportion of subjects who were finally confirmed to have pheochromocytoma. We then calculated the predictive values of uMN + uNMN in each of these subsets. In the group of patients presenting with hypertension alone, where the pretest probability is low and the occurrence of pheochromocytoma was 8 per ent (the PPV was very low). In those with adrenal mass and hypertension, where the pretest probability is high and the occurrence of pheochromocytoma was high (the PPV was 100%). Table III shows the predictive values of uMN + uNMN in these different clinical settings.

Discussion
Our observation that the uMN+uNMN test has a good sensitivity in the initial screening of a patient with suspected phaeochromocytoma is consistent with previous studies10–12. Considering uMN and uNMN separately, uMN had a good specificity but a poor sensitivity. However, four out of 11 false negatives were due to the extra-adrenal phaeochromocytomas which lack phenylethanolamine- N- methyl transferase and hence predominantly secrete norepinephrine. On the contrary, uNMN had a high sensitivity with a trade-off in the specificity leading to a large number of false positives. This was especially true when the upper limit given by the assay manufacturer was used as cut-off. When the cut-off was increased to twice the upper limit, there was a significant decrease in the number of false positives.
Phaeochromocytomas differ considerably in the type of bioamines produced, depending on factors like genetic mutation, adrenal/extra-adrenal location and tumour size. Hence, it is logical to combine both uMN and uNMN, while screening for phaeochromocytomas. In our study, considering elevation of either uMN or uNMN above twice the manufacturer's upper limit, 95 per cent sensitivity with a 92.3 per cent specificity could be achieved. The corresponding NPV was excellent (98%) and PPV (82.6%) was reasonable. However, the predictive values of any particular test will depend on the pretest probability of the disease being tested. The above predictive values apply to the present study population in a large referral center, where the phaeochromocytoma are diagnosed in a high proportion (27.7%). The test will not perform as well in a secondary hospital level when done in an unselected population with very low tumor prevalence.
The predictive values of the test were analyzed in subsets of patients with different pretest probabilities. If we look at the subset of our patients presenting with hypertension and certain clinical symptoms suggestive of phaeochromocytoma, the prevalence was eight per cent. In this group the PPV was only 50 per cent but the NPV was 100 per cent. This implies that a negative test using the above cut-off value eliminates phaeochromocytoma as a diagnosis. On the other hand, among those with a positive test only 50 per cent would actually have the tumour. If we apply the above sensitivity and specificity Figure s to a general hypertensive population where the prevalence reported in available literature is as low as 0.5 per cent, the PPV drops to six per cent but the NPV still remains at 100 per cent. This makes this test suitable for ruling out phaeochromocytoma in the general hypertensive population with a very low pretest probability. In the subset of our patients with adrenal masses with or without hypertension, where the prevalence of phaeochromocytoma was 26 per cent, the PPV increased to 100 per cent and NPV decreased to 84.6 per cent. This suggests that in this group of patients with a high pretest probability, a cut-off value lower than the value we have selected would be appropriate.
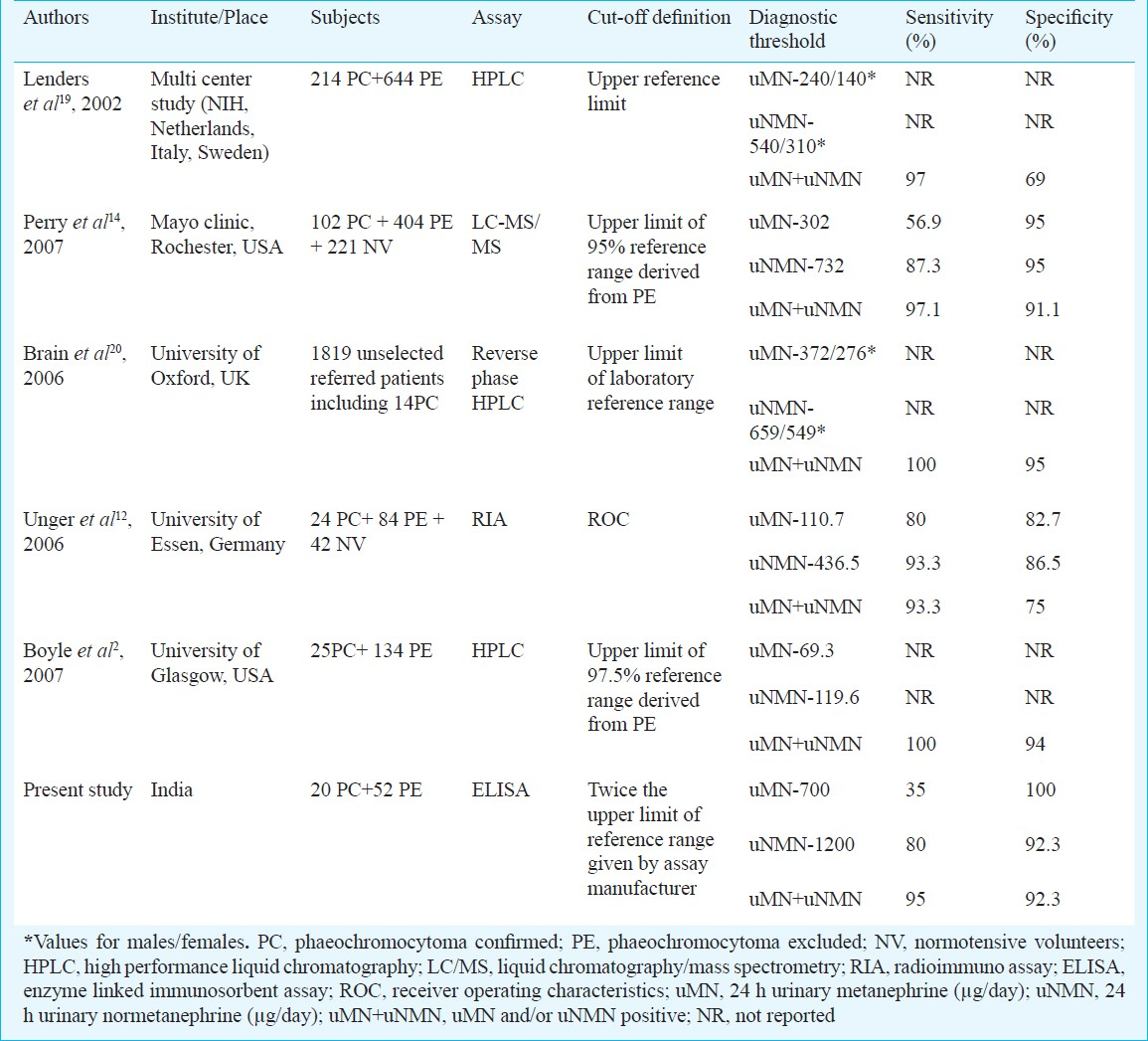
Different studies employing different methods for measuring urinary fractionated metanephrines have reported different cut-off values with varying sensitivity and specificity. However, the problem of low specificity for uMN is a common finding in all studies1314. In 2002, Lenders et al11 showed that uMN and pMN had similar sensitivity but uMN had lower specificity (69 vs 89%), however, they used different assays for urine and plasma. Later studies have proved that uMN and pMN can perform equally. Unger et al12reported similar specificity for pMN (79%) and uMN (75%), using RIA to measure the analytes in both urine and plasma. A recent study by Grouzmann et al15 concluded that in the absence of renal insufficiency both uMN and pMN perform equally. In our study, a higher specificity of 88 per cent was found by combining uMN+uNMN.
The low specificity with uMN is due to the large number of false positives caused by drugs, dietary constituents and inappropriate sampling. Drugs can alter metanephrine measurement by either directly interfering with the assay or by affecting the endogenous catecholamine metabolism. Analytical interference by drugs with a similar chemical structure is common in high performance LC-electrochemical detection but not with MS16. The immunoassays for metanephrines are also shown to be free from analytical interference by the commonly used drugs (cross reactivity <3) which have structural similarity to metanephrines17. However, nonspecific/alpha 2 blockers and beta blockers can cause false positive elevation by inhibiting noradrenaline uptake in the sympathetic nerve terminals or by attenuating the feedback inhibiton of its release. Selective alpha 1 blockers do not cause this problem. There are no recommendations on dietary restrictions for testing uMN. de Jong et al18 showed that a catecholamine rich diet can increase deconjugated normetanephrines upto 2 fold but not the metanephrines in plasma and urine. In our study, false positive elevations were more common with uNMN compared to uMN in patients without any drug or dietary restriction. This may indicate that exogenous factors influence uNMN more commonly than uMN. This does not disqualify uMN+uNMN as an initial screening test.
There is no universally accepted threshold for uMN and uNMN which can differentiate phaeochromocytomas from patients without the disease. Table IV summarizes the results of previous studies done on urinary fractionated metanephrines. Our cut-off levels differ from the previous studies indicating that the assay used and the reference population influence the clinical cut-off. Our study confirms the previous findings that the upper limit derived by studying normotensive healthy controls is of insufficient discriminatory value. It would be preferable to define the cut-off using a group of subjects suspected to have phaeochromocytoma in whom the diagnosis was excluded.
The major strength of our study was inclusion of a clinically relevant reference population and histopathologically proven phaeochromocytomas cases. The limitation of the study was that the exclusion of phaeochromocytoma in our study was done by imaging. Another limitation was that the adequacy of urine collection was not assessed by concurrent urine creatinine excretion.
In conclusion, urinary metanephrines measured by ELISA have adequate specificity to be used as an initial screening test for ruling out phaeochromocytoma. However, one cannot use the upper limit stated by the manufacturer derived from normotensive subjects as the cut-off, as there are many false positives. Increasing the cut-off to twice this upper limit improves the specificity and negative predictive value, to the extent that it can be used for ruling out phaeochromocytoma in a hypertensive population. Each hospital needs to define the cut-off by using its own assay and by choosing a proper control population. In patients with adrenal or extra-adrenal mass with hypertension, even milder elevations of urinary metanephrines may suggest the presence of phaeochromocytoma.
References
- Choice of biochemical test for diagnosis of pheochromocytoma: validation of plasma metanephrines. Curr Hypertens Rep. 2002;4:250-5.
- [Google Scholar]
- Comparison of diagnostic accuracy of urinary free metanephrines, vanillyl mandelic Acid, and catecholamines and plasma catecholamines for diagnosis of pheochromocytoma. J Clin Endocrinol Metab. 2007;92:4602-8.
- [Google Scholar]
- Understanding catecholamine metabolism as a guide to the biochemical diagnosis of pheochromocytoma. Rev Endocr Metab Disord. 2001;2:297-311.
- [Google Scholar]
- Free or total metanephrines for diagnosis of pheochromocytoma: what is the difference? Clin Chem. 2001;47:988-9.
- [Google Scholar]
- A systematic review of the literature examining the diagnostic efficacy of measurement of fractionated plasma free metanephrines in the biochemical diagnosis of pheochromocytoma. BMC Endocr Disord. 2004;4:2.
- [Google Scholar]
- Plasma and urinary metanephrines determined by an enzyme immunoassay, but not serum chromogranin A for the diagnosis of pheochromocytoma in patients with adrenal mass. Exp Clin Endocrinol Diabetes. 2012;120:494.
- [Google Scholar]
- Performance of plasma fractionated free metanephrines by enzyme immunoassay in the diagnosis of pheochromocytoma and paraganglioma in children. Endocr Pract. 2012;18:694.
- [Google Scholar]
- Evaluation of an enzyme immunoassay for plasma-free metanephrines in the diagnosis of catecholamine-secreting tumors. Eur J Endocrinol. 2009;161:131.
- [Google Scholar]
- The value of immunoassays for metanephrines in the biochemical diagnosis of pheochromocytomas. Horm Metab Res. 2009;41:676-9.
- [Google Scholar]
- Advances in metanephrine testing for the diagnosis of pheochromocytoma. Clin Lab Med. 2004;24:85-103.
- [Google Scholar]
- New advances in the biochemical diagnosis of pheochromocytoma: moving beyond catecholamines. Ann N Y Acad Sci. 2002;970:29-40.
- [Google Scholar]
- Diagnostic value of various biochemical parameters for the diagnosis of pheochromocytoma in patients with adrenal mass. Eur J Endocrinol. 2006;154:409-17.
- [Google Scholar]
- The diagnostic efficacy of urinary fractionated metanephrines measured by tandem mass spectrometry in detection of pheochromocytoma. Clin Endocrinol (Oxf). 2007;66:703.
- [Google Scholar]
- A comparison of biochemical tests for pheochromocytoma: measurement of fractionated plasma metanephrines compared with the combination of 24-hour urinary metanephrines and catecholamines. J Clin Endocrinol Metab. 2003;88:553.
- [Google Scholar]
- Diagnostic accuracy of free and total metanephrines in plasma and fractionated metanephrines in urine of patients with pheochromocytoma. Eur J Endocrinol. 2010;162:951-60.
- [Google Scholar]
- Advances in Biochemical Screening for Pheochromocytoma using Biogenic Amines. Clin Biochem Rev. 2009;30:3-17.
- [Google Scholar]
- Freedom from drug interference in new immunoassays for urinary catecholamines and metanephrines. Clin Chem. 1999;45:2216-23.
- [Google Scholar]
- Dietary influences on plasma and urinary metanephrines: implications for diagnosis of catecholamine-producing tumors. J Clin Endocrinol Metab. 2009;94:2841-9.
- [Google Scholar]
- Biochemical diagnosis of pheochromocytoma: which test is best? JAMA. 2002;287:1427-34.
- [Google Scholar]
- Measurement of urinary metanephrines to screen for pheochromocytoma in an unselected hospital referral population. Clin Chem. 2006;52:2060-4.
- [Google Scholar]






