Translate this page into:
Current status of leprosy as seen in a tertiary care hospital in north India
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Leprosy is a chronic infectious disease caused by Mycobacterium leprae, which can affect all ages and both sexes. Leprosy has been a major public health problem of India in the last century. Leprosy control programmes based on dapsone monotherapy were initiated in 1955, followed by multidrug therapy in 19821. In 1993, the National Leprosy Elimination Programme (NLEP) was initiated with the goal to decrease the prevalence rate of leprosy below 1 case/10,000 population. India has achieved elimination of leprosy as a public health problem in December 2005 by recording a prevalence rate of 0.95/10,000 population2 and subsequently, it has further declined to 0.84/10,000 population as in March 20063. Leprosy was supposed to be eliminated by World Health Organization at the global level by the end of the year 2000; however, it still remains a significant public health problem at a national level in six countries, where India alone accounts for 64 per cent of prevalence and 78 per cent of new case detection, worldwide. The global registered prevalence of leprosy at the beginning of 2006 was 219,826 cases. The number of new cases reported during 2005 was 296,4994. There are reports that the numbers of leprosy patients presenting to dermatologists in both private and teaching hospitals are increasing as peripheral surveillance activities are discontinued5. This would require a specialized focus on early diagnosis, complete treatment and detection and management of disabilities.
The Department of Microbiology, at Chhatrapati Shahuji Maharaj Medical University (CSMMU), Lucknow, in north India is a tertiary care centre providing laboratory confirmation of leprosy by slit skin smear examination6. Patients with clinical suspicion of leprosy, attending the CSMMU Hospitals are referred to the Department of Microbiology, CSMMU. Smears are prepared from six sites (nasal mucosa of both the nostrils, both the ear lobes and two of the most prominent lesions), and stained with modified Zeihl-Neelsen stain. Smear are examined under oil immersion to look for acid fast bacilli (AFB), both intra- and extra-cellular, and reported as positive or negative for AFB.
We have observed a rise in number of cases of leprosy in the last two years (Table). In 2007, a total of 29 cases with clinical suspicion of leprosy were referred for diagnosis, of whom only 2 cases were AFB positive, showing only a few bacilli in nasal smears. Smears prepared from lesions and ear lobes were AFB negative. A rise in number of referred as well as AFB positive cases was seen in 2008 and 2009 (Table). Majority of smears made from these cases had large number of bacilli even globi, irrespective of the site.
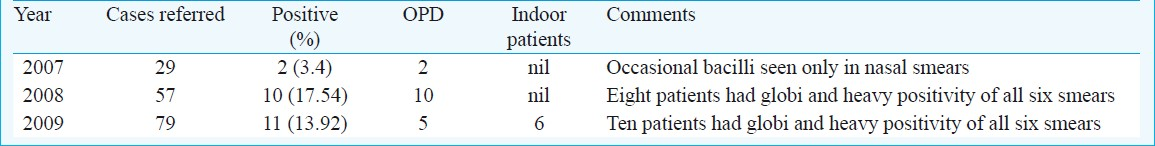
All cases seen in 2007 and 2008 were out patients, not requiring hospitalization, while six of 11 patients seen in 2009 had serious manifestations like loss of extremities and hence required hospital admission. Three of ten patients seen in 2008 and six of 11 patients seen in 2009 had depressed bridge of nose. The remaining presented with either loss of sensation and/or hypo-pigmented skin patches and/or thickening of radial nerve, in various combinations.
The end of NLEP signifies the elimination of leprosy as a public health problem in India. However, numbers of leprosy cases are increasing at other teaching hospitals as well4 probably due to discontinuation of surveillance activities, distribution of multidrug therapy, deformity prevention and management performed by leprosy workers during the NLEP phase. Specialized focus on early diagnosis, complete treatment and detection and management of disabilities is still required to keep a check on leprosy. Also, multidrug therapy should also be made available at the tertiary care centres rather than being available only at primary health centers and municipal dispensaries for prompt initiation of therapy.
References
- Recent advances in the control programs and therapy of leprosy. Indian J Dermatol Venereol Leprol. 2004;70:269-76.
- [Google Scholar]
- Special Correspondent, India achieves leprosy eradication target. 2006. The Hindu News paper. :15. Available from: col 1 www.thehindu.com
- [Google Scholar]
- National leprosy eradication programme. Available from: http://india.gov.in/sectors/health_family/national_programme.php
- [Google Scholar]
- The imperatives of leprosy treatment in the pre- and post-global leprosy elimination era: appraisal of changing the scenario to current status. J Dermatolog Treat. 2008;19:82-91.
- [Google Scholar]
- Leprosy in the era of integration. Indian J Dermatol Venereol Leprol. 2009;75:190-1.
- [Google Scholar]
- WHO. In: Laboratory techniques for leprosy. Geneva: WHO; 1987. p. :21-9. WHO/CSD/Lep/86.4
- [Google Scholar]





