Translate this page into:
Assessment of health-related quality of life in individuals with interstitial lung diseases in a tertiary care hospital in south India
For correspondence: Dr Kavitha Venkatnarayan, Department of Pulmonary Medicine, St. Johns National Academy of Health Sciences, Bengaluru 560 034, Karnataka, India e-mail: kaviaiims@gmail.com
-
Received: ,
Accepted: ,
Abstract
Background & objectives
Interstitial lung diseases (ILD) cause progressive symptoms and decline in lung functions which impact health-related quality of life (HRQoL). Although HRQoL is gaining wider acceptance as an endpoint for disease perception, limited data is available regarding the same in Indians with ILD. Hence, this study was undertaken to assess HRQoL and its correlation with lung function parameters in individuals with ILD in a tertiary care setting in south India.
Methods
A hundred and fifty-nine consecutive patients with ILD were recruited between June 2022 to December 2023. HRQoL was assessed using the ILD specific K-BILD, generic EQ-5D-5L and an adapted version of the validated PESaM questionnaires. Correlation between various domains of the three questionnaires and lung function parameters was analyzed followed by linear regression analysis.
Results
The study population consisted predominantly of females (64.1%), with CTD-ILD being the most common ILD (40.8%). HRQoL impairment was noted, predominantly affecting the ‘breathlessness and activity’ domain and significant correlation was noted between K-BILD and EQ-5D-5L across domains. On regression analysis, FVC, 6-minute walk distance and desaturation were independent predictors of HRQoL. Type of ILD and disease duration did not have a significant association with HRQoL measures.
Interpretation & conclusions
‘Breathlessness and activity’ domain of HRQoL was affected the most in participants with ILD. Forced vital capacity, six-minute walk distance and exercise induced desaturation were independent predictors of HRQoL among individuals with ILD.
Keywords
HRQoL
interstitial lung diseases
patient reported outcomes
questionnaire
Interstitial lung diseases (ILD) are a diverse group of illnesses characterized by lung parenchymal inflammation and fibrosis. The natural course of most ILDs remains progressive with only a very few effective treatment options. The focus of clinical management and primary endpoints in research studies in ILD include monitoring periodic changes in lung function, exercise capacity and radiological findings1. Although these assessments yield meaningful information, these may fail to comprehensively capture the patients’ perspective of the disease. For instance, dyspnea and refractory cough reportedly impede the psychosocial well-being of individuals with ILD, which in turn impairs their health-related quality of life (HRQoL)2. Apart from progressive symptoms, loss of independence and reliance on caregiver for activities of daily living, financial burden of treatment and social isolation negatively impact their HRQoL. As patient reported outcomes (PRO) are reported by the patients themselves without physician interpretation, these can provide a better perspective of how an intervention impacts the patient’s condition3.
The capacity of an individual to lead a life that they deem fulfilling is known as HRQoL, and it is a critical PRO that is assessed using various questionnaires. These include generic questionnaires which assess general health status regardless of the underlying disease and are useful in comparing HRQoL across various chronic diseases and with healthy population. Disease specific questionnaires have been designed to capture the distinctive impact of ILD on HRQoL better than generic instruments. Although translations for these tools are available in various languages, adaptability of these instruments is limited due to socio-cultural differences in disease perception and differences in health literacy4.
Prioritization of HRQoL is a concurred need in clinical practice as well as research studies alike. Even though clinical trials have begun to recognize PRO as important parameters, these are generally relegated to a lower priority status as endpoints. Limited data is available on HRQoL in Indians with ILD and their relationship with disease severity. Hence, this study aimed to assess the HRQoL in individuals with ILD and their correlation with lung function parameters.
Material & Methods
This study was undertaken from June 2022 to December 2023 at the department of Pulmonary Medicine, St. John’s National Academy of Health Sciences, Bengaluru, after obtaining approval from Institutional Ethics Review Board. Individuals presenting to the pulmonary medicine outpatient and ILD clinic consecutively were recruited in this study. Consenting individuals aged >18 yr, diagnosed with ILD as per standard guidelines and multidisciplinary discussions were recruited in the study. Illiterate individuals who lacked the competence to complete the questionnaires were excluded. Pregnant women, individuals with ILDs with significant extrapulmonary manifestations which could affect HRQoL, those with an exacerbation of ILD in the preceding four weeks, and those having any terminal illness were excluded from this study.
After obtaining a written informed consent, clinical, demographic information and self-reported comorbidities were collated. Spirometry was performed using Smart PFT (Peso Medicare, India) as per ATS/ ERS recommendations5 and forced vital capacity (FVC) per cent predicted was noted. A six-minute walk test (6MWT) was performed as per ATS/ ERS guidelines6, the distance walked, and desaturation were noted. HRQoL assessment was done using the ILD specific King’s Brief Interstitial Lung Disease (K-BILD) questionnaire and the generic 5-level EQ-5D version (EQ-5D-5L) questionnaire. Permission was sought from the copyright owners of these questionnaires for use in the study. We also wanted to assess the patient related experience with the treatment prescribed. The Patient Experiences and Satisfaction with Medications (PESaM) questionnaire did not have an English version. Hence after obtaining permission from the developers, an adapted version of the validated questionnaire (Dutch) was used7. This was chosen with an intent to gain a comprehensive perspective on the impact of the disease and the treatment on patients’ lives. Details of the questionnaires and the adaptations made are mentioned in the supplementary material.
Statistical analysis
Data was collected and managed on a Microsoft Excel worksheet. All the variables were assessed for normality. Continuous variables were summarized as mean (SD) or median (IQR) as appropriate. Categorical variables were summarized as frequency and percentages. Pearson’s correlation coefficient was calculated to assess the correlation between HRQoL domains and lung function parameters. The strength of correlation was assigned as follows: an r-value (Pearson’s co-efficient) of 0.8 to 1 was considered a strong correlation, 0.6 to 0.79 fairly strong, 0.4 to 0.59 moderate and less than 0.4 was considered a weak correlation respectively. Linear regression analysis was performed to find the association between the HRQoL domains and demographic and lung function parameters.
The data was analyzed using SPSS version 29 and a two-sided P value < 0.05 was considered significant.
Results
A hundred and fifty-nine individuals with ILD participated in this study were recruited, with a mean (SD) age of 53.2 (12.9) yr which predominantly included females (64.15%). The most common etiology of ILD was connective tissue disease associated ILD (40.8%) followed by hypersensitivity pneumonitis (11.3%) and idiopathic pulmonary fibrosis (10.6%). The median (IQR) duration of illness was 5 (3, 25) months. Co-morbidities were present in 105 (66%) patients with hypertension (37.1%) and diabetes mellitus (33.9%) being the commonest, followed by hypothyroidism, ischemic heart disease and obstructive airway disease. Baseline characteristics of the patients are summarized in Table I.
| Participant characteristics | Values |
|---|---|
| Age (yr), mean ± SD | 53.2 ± 12.9 |
| Sex | n (%) |
| Females | 102 (64.1) |
| Males | 57 (35.8) |
| Duration of illness (months), median (IQR) | 5 (3,25) |
| Type of ILD | n (%) |
| IPF | 17 (10.6) |
| CTD-ILD | 65 (40.8) |
| IPAF | 14 (8.8) |
| HP | 18 (11.3) |
| NSIP | 12 (7.5) |
| Sarcoidosis | 9 (5.6) |
| Others | 24 (15) |
| Co-morbidities | n (%) |
| Hypertension | 59 (37.1) |
| Diabetes Mellitus | 54 (33.9) |
| Hypothyroidism | 22 (13.8) |
| Ischemic heart disease | 8 (5) |
| Obstructive airway disease | 5 (3.1) |
| Any comorbidity | 105 (66) |
| FVC (% predicted), mean± SD | 51.7± 13.6 |
| 6-minute walk distance (meters), mean± SD | 345.7± 126 |
| 6 MWT desaturation (%), mean± SD | 11.7± 7.6 |
FVC, forced vital capacity; 6MWT, six-minute walk test; ILD, interstitial lung disease; SD, standard deviation; IPF, idiopathic pulmonary fibrosis; NSIP, nonspecific interstitial pneumonia; CTD-ILD, connective tissue disease associated ILD; HP, hypersensitivity pneumonitis; IPAF, interstitial pneumonia with autoimmune features
The mean ± SD score for K-BILD was 55.7 ± 9.8 with the lowest mean scores for the ‘breathlessness and activity’ domain (40.1 ± 18.2) followed by ‘psychological impact’ (55.5 ± 11.7) and ‘chest symptoms’ (76.5 ± 18.8) respectively. The mean ± SD score for EQ-5D-5L was 66.2 ± 16.3 and 0.6 ± 0.3 for the EQ VAS and EQ-5D-5L index, respectively. The adapted version of the PESaM questionnaire showed that majority of the population was satisfied with medications (88.6%), thought that medications were effective (64.1%), had a positive impact on social life (61.6%), and were easy to consume (89.9%). Findings of the information provided in results of the questionnaires are summarized in Table II and the Figure. Descriptive questions of PESaM (adapted version) showed that additional cost incurred for medications was the usual reason for dissatisfaction. Common side effects mentioned were weight gain, swelling and puffiness of the face, gastric discomfort, loose stools, altered taste, decreased appetite and sleep disturbances. Participants were often found citing weight gain and change in physical appearance as being discomforting during social interactions.
| Questionnaire domain | Values |
|---|---|
| EQ-5D-5L, mean ± SD | |
| Index | 0.63 ± 0.38 |
| VAS | 66.2 ± 16.3 |
| K-BILD, mean ± SD | |
| Total | 55.7 ± 9.8 |
| Psychological impact | 55.5 ± 11.7 |
| Breathlessness and activity | 40.1 ± 18.2 |
| Chest symptoms | 76.5 ± 18.8 |
| PESaM (adapted version), n (%) | |
| Are you satisfied with the medications you are taking? | |
| Yes | 141 (88.6) |
| No | 18 (11.3) |
| Do you think the medications are effective in treating your condition? | |
| Yes | 102 (64.1) |
| Maybe | 26 (16.3) |
| No | 13 (8.1) |
| Does it have a positive impact on activities you enjoy doing? | |
| Yes | 74 (46.5) |
| Maybe | 32 (20.1) |
| No | 34 (21.3) |
| Does it have a positive impact on your social life and interpersonal relationships? | |
| Yes | 98 (61.6) |
| Maybe | 34 (21.3) |
| No | 27 (16.9) |
| Are your drugs easy to use/ consume? | |
| Yes | 143 (89.9) |
| No | 16 (10) |
| Is the dosage bothersome to you (frequency/ route of the medication)? | |
| Yes | 147 (92.4) |
| No | 12 (7.5) |
EQ-5D-5L, EuroQol 5-dimension 5-level; K-BILD, King’s brief interstitial lung disease; PESaM, patient experiences and satisfaction with medications; VAS, visual analog scale
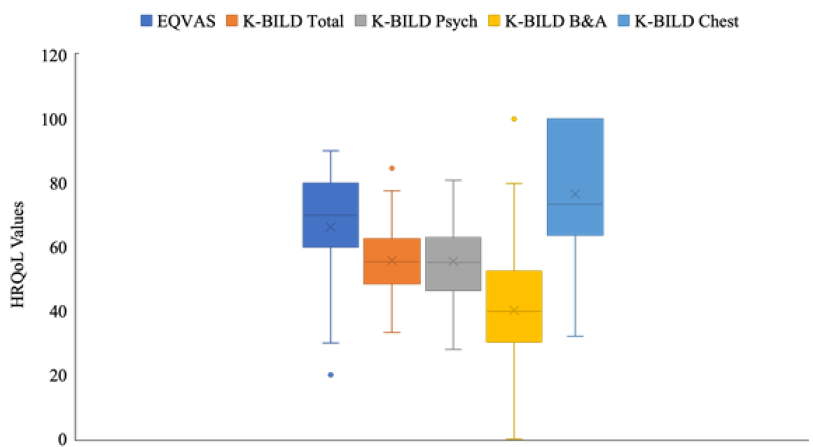
- Results of health-related quality of life questionnaires. EQ VAS, EuroQol Visual Analog Scale; K-BILD, King’s Brief Interstitial Lung Disease - B&A, breathlessness and activity domain, Chest, chest symptoms domain, Psych, Psychological domain.
On assessing correlation of HRQoL with lung function parameters, both the questionnaires had a significant correlation with 6-min walk distance and desaturation during 6MWT. However, the correlation of all the domains was weak with FVC per cent predicted (Table III). On analyzing the correlation between EQ-5D-5L and K-BILD questionnaires, total K-BILD score had a strong correlation with the EQ-5D-5L index (r = 0.84; P<0.001) and EQ-VAS (r=0.73; P<0.001). Analysis of the correlation between different domains of both the questionnaires are presented in Table IV.
| EQ-5D-5L index | EQ VAS | K-BILD total | K-BILD psych | K-BILD B & A | K-BILD chest | FVC% predicted | 6-minute walk distance | 6MWT desaturation | |
|---|---|---|---|---|---|---|---|---|---|
| EQ-5D-5L index | 1 | ||||||||
| EQ VAS | 0.698** | 1 | |||||||
| K-BILD total | 0.842** | 0.731** | 1 | ||||||
| K-BILD psych | 0.774** | 0.706** | 0.941** | 1 | |||||
| K-BILD B&A | 0.833** | 0.609** | 0.910** | 0.761** | 1 | ||||
| K-BILD chest | 0.591** | 0.536** | 0.749** | 0.657** | 0.592** | 1 | |||
| FVC% predicted | 0.391** | 0.266** | 0.424** | 0.367** | 0.393** | 0.472** | 1 | ||
| 6-min walk distance | 0.768** | 0.548** | 0.678** | 0.607** | 0.715** | 0.428** | 0.414** | 1 | |
| 6MWT desaturation | –0.606** | –0.423** | –0.510** | –0.413** | –0.575** | –0.322** | –0.247** | –0.517** | 1 |
Correlation is significant at P**<0.01. B & A, breathlessness and activity domain; Chest, chest symptoms domain; Psych, psychological domain
| K-BILD psych | K-BILD B & A | K-BILD chest | EQ-5D-5L mobility | EQ-5D-5L self-care | EQ-5D-5L usual activity | EQ-5D-5L pain | EQ-5D-5L anxiety | |
|---|---|---|---|---|---|---|---|---|
| K-BILD Psych | 1 | |||||||
| K-BILD B&A | 0.761** | 1 | ||||||
| K-BILD chest | 0.657** | 0.592** | 1 | |||||
| EQ-5D-5L mobility | –0.730** | –0.833** | –0.596** | 1 | ||||
| EQ-5D-5L self-care | –0.691** | –0.809** | –0.544** | 0.860** | 1 | |||
| EQ-5D-5L usual activity | –0.736** | –0.829** | –0.580** | 0.850** | 0.901** | 1 | ||
| EQ-5D-5L pain | –0.496** | –0.373** | –0.489** | 0.460** | 0.394** | 0.405** | 1 | |
| EQ-5D-5L anxiety | –0.759** | –0.584** | –0.551** | 0.608** | 0.555** | 0.601** | 0.529** | 1 |
Correlation is significant at P**<0.01
Linear regression analysis was performed to assess the relationship between demographic variables, lung function parameters and HRQoL domains. Univariate analysis was initially performed to identify significant predictors of HRQoL, providing a preliminary understanding of each variable’s individual impact. Baseline characteristics such as age, sex, presence of comorbidities, duration of illness and type of ILD were not found to be significant in the univariate analysis and were excluded in the regression model.
A multivariate analysis was then conducted to assess the association between lung function parameters and HRQoL. The analysis was adjusted to account for the potential confounding effects of different lung function parameters on each other, ensuring that the association between each parameter and HRQoL was examined independently. In multivariate analysis, it was found that FVC per cent predicted was significantly associated with the K-BILD ‘chest symptom’ domain; six-min walk distance was significantly associated with EQVAS, K-BILD total, ‘psychological’ and ‘breathlessness and activity’ domains; and desaturation during 6MWT with EQVAS, K-BILD and K-BILD ‘breathlessness and activity’ domain (Table V).
| Univariate analysis | EQ-5D-5L Index | EQ-VAS | K-BILD Total | K-BILD Psych | K-BILD B & A | K-BILD Chest |
|---|---|---|---|---|---|---|
| Age (yr) | 0.043 | 0.129 | 0.054 | 0.056 | 0 | 0.107 |
| Sex | -0.002 | 0.080 | 0.022 | 0.085 | -0.032 | 0.062 |
| Duration of illness (months) | -0.026 | -0.102 | -0.097 | -0.111 | -0.034 | -0.152* |
| Presence of comorbidity | 0.021 | 0.008 | 0.019 | 0.002 | 0.038 | -0.014 |
| Type of ILD | 0.048 | -0.067 | 0.035 | 0.072 | 0.007 | -0.064 |
| FVC % Predicted | 0.067 | 0.023 | 0.153* | 0.121 | 0.105 | 0.339** |
| 6-min walk distance (m) | 0.593** | 0.427** | 0.496** | 0.475** | 0.523** | 0.210* |
| 6MWT desaturation (%) | -0.271** | -0.210* | -0.219** | -0.140 | -0.279** | -0.146 |
| Multivariate analysis | EQ-5D-5L Index | EQ-VAS | K-BILD Total | K-BILD Psych | K-BILD B & A | K-BILD Chest |
| FVC % predicted | ||||||
| Unadjusted | 0.01** | 0.32* | 0.3** | 0.32** | 0.5 | 0.65** |
| Adjusted | 0.002 | 0.05 | 0.12 | 0.12 | 0.14 | 0.48** |
| 6-min walk distance (m) | ||||||
| Unadjusted | 0.02** | 0.71** | 0.05** | 0.05** | 0.1** | 0.06** |
| Adjusted | 0.02** | 0.06* | 0.3** | 0.05** | 0.08** | 0.32 |
| 6MWT Desaturation (%) | ||||||
| Unadjusted | -0.03** | -0.91** | -0.67** | -0.64** | -1.3** | -0.8** |
| Adjusted | -0.01 | -0.41** | -0.27* | -0.19 | -0.7** | -0.3 |
P* ≤0.05, ** ≤0.001. FVC, forced vital capacity; 6MWT, six min walk test
Discussion
The measurement of one’s own subjective well-being that is impacted by an illness or its treatment is known as health-related quality of life (HRQoL)8. Interstitial lung diseases (ILD) are a group of chronic respiratory diseases typified by progressive dyspnea and cough. Current treatment options depend on the type of ILD and essentially include steroids, immunosuppressants and antifibrotics. Although progress has been made in the last decade with newer therapies, a significant proportion of affected individuals continue to experience progressive decline in lung functions, disturbing symptoms and become dependent for activities of daily living. Treatment for ILD also has financial implications and as the disease progresses, the requirement of long-term oxygen therapy further limits activities. All the above result in social isolation and have a psychological impact which affects the HRQoL9.
High quality clinical care can only be delivered by employing a patient-centric approach. It has been increasingly agreed upon by clinicians, researchers, and patients that disease management and research studies should focus on patient related outcomes (PROs) as an important endpoint3. PROs are patient-reported outcomes that are not interpreted by a clinician and address how an illness or treatment affects a person’s quality of life10. HRQoL is difficult to evaluate owing to its subjective and dynamic nature with multiple domains and varying perception among patients with similar disease severity. These idiosyncrasies are augmented by social, cultural, and religious differences which affect the value ascribed to each domain.
Traditionally treatment of ILD has focused on tangible outcomes like change in lung function, exercise capacity and radiological findings. Although HRQoL is being included as an important endpoint in therapeutic decision making and research studies, it is still given a low priority11. HRQoL in individuals with ILD was initially assessed using questionnaires validated in other chronic diseases like St. George Respiratory questionnaire (SGRQ)12. However, these questionnaires may not capture the nuances which are unique to ILD. Hence, ILD specific questionnaires were developed including King’s Brief Interstitial Lung Disease (K-BILD), A Tool to Assess Quality of life in Idiopathic Pulmonary Fibrosis (ATAQ-IPF), Living with IPF (L-IPF) and Chronic Hypersensitivity Pneumonitis Health Related Quality of Life (CHP-HRQoL).
Impaired HRQoL in individuals with ILD has been reported in studies using various questionnaires. Many of these studies have been done on individuals with idiopathic pulmonary fibrosis (IPF). HRQoL assessed by SGRQ was reported to be impaired in IPF and disease duration, co-morbidities, FVC and need for long term oxygen therapy were the prime drivers of the impairment13. A systematic review reported that IPF had a negative impact on HRQoL by predominantly affecting the physical health domains. Various instruments were used to assess the same and standardization of these tools could harmonize the findings and make comparisons possible across the globe14.
K-BILD questionnaire was developed as a disease specific tool to assess HRQoL in individuals with ILD. The questionnaire has previously been translated and validated in European and South American countries15,16. It has been found to be a useful tool in assessing HRQoL in ILDs and is responsive to interventions17-19. The ‘breathlessness and activity’ subscale of K-BILD was found to have high internal consistency and reliability and is recommended as the best PRO measure for dyspnea in individuals with ILD20.
Representation of Asians is reportedly <20 per cent in literature14 with infinitesimal data available from Indians. In our study, we chose to use a combination of generic (EQ-5D-5L) and ILD specific (K-BILD) questionnaires as per recommendations to assess the HRQoL comprehensively among Indians 21. Since we believed that treatment offered also influences HRQoL, we also used an adapted version of the PESaM questionnaire to assess patient experience and satisfaction with the treatment. Our study population predominantly included females with CTD-ILD. Compared to other studies our participants had a lower mean FVC per cent predicted indicating a more severe spectrum of ILD. In concordance with the other studies, the mean K-BILD scores were comparable with ‘breathlessness and activity’ domain affected more than ‘psychological’ and ‘chest symptoms’ domain18,22.
Consistent with other studies, a strong correlation was found between the questionnaires specifically in the ‘breathlessness and activity’ domain. Our study showed a weak correlation between the HRQoL measures and FVC per cent predicted. This reinforces the fact that physiological testing may not completely capture the impact of the disease. The 6MWT, being a submaximal exercise testing, showed a strong correlation with HRQoL. Since most of the activities of daily living are performed at submaximal levels of exertion, it may reflect the exercise capacity better and thus correlate better with the health status6.
Results of the adapted version of the PESaM questionnaire provide insights into effects and side-effects of medications prescribed and stress the importance of considering patient experience-related outcomes as well.
This study was not without limitations. As it is a single-center study, with a small sample size, the results cannot be generalized. The population included had varied subtypes of ILD and owing to smaller numbers, a subgroup analysis of the HRQoL based on the type of ILD could not be performed. Illiterate individuals had to be excluded due to the self-administered nature of most of the questionnaires. Interview based assessment of these questionnaires still needs validation. We were unable to perform a comprehensive lung function testing including diffusion capacity and lung volumes in all patients. The appropriateness of the treatment offered and the effect of each medication on HRQoL was not analyzed. It also remains to be seen if these measures are sensitive to changes with treatment during follow up.
It was also found during the study that aspects like disturbing cough, poor sleep quality and financial burden were not adequately captured by these questionnaires. Many of our participants found it difficult to comprehend and answer a few questions and required assistance for the same. Though symptom and domain specific questionnaires are available, it is the need of the hour to have a comprehensive tool which can evaluate all aspects of HRQoL relevant to patients with ILD in the right social and cultural framework to enable them to handle their disease better.
Overall, the findings of this study suggest that FVC, six-min walk distance and exercise induced desaturation were independent predictors of HRQoL in patients with ILD.
Acknowledgment
Authors acknowledge Surinder Birring for permitting us to use the K-BILD questionnaire. We would like to thank Dr ML Kimman for providing the validated Dutch version of the PESaM questionnaire from which questions for the current study were adapted. EuroQol group is also acknowledged for granting permission to use the EQ-5D-5L questionnaire. Details of the questionnaires used, and the adaptation made are provided in the supplementary material.
Financial support & sponsorship
None.
Conflicts of Interest
None.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- Patients’ perceptions and patient-reported outcomes in progressive-fibrosing interstitial lung diseases. Eur Respir Rev. 2018;27:180075.
- [Google Scholar]
- Patient-reported outcomes in idiopathic pulmonary fibrosis research. Chest. 2012;142:291-97.
- [Google Scholar]
- Health related quality of life in interstitial lung disease: Can We Use the same concepts around the world? Front Med (Lausanne). 2021;8:745908.
- [Google Scholar]
- ATS statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111-7.
- [Google Scholar]
- Validity of the patient experiences and satisfaction with medications (PESaM) Questionnaire. Patient. 2019;12:149-62.
- [Google Scholar]
- Health, health-related quality of life, and quality of life: What is the difference? Pharmacoeconomics. 2016;34:645-9.
- [Google Scholar]
- Health-related quality of life in idiopathic pulmonary fibrosis: Where are we now? Curr Opin Pulm Med. 2013;19:474-9.
- [Google Scholar]
- Patient-reported outcomes (PROs) and Patient-reported outcome measures (PROMs) Health Serv Insights. 2013;6:61-8.
- [Google Scholar]
- Outcome measures for clinical trials in interstitial lung diseases. Curr Respir Med Rev. 2015;11:163-174.
- [Google Scholar]
- Assessment of health-related quality of life in patients with interstitial lung disease. Chest. 1999;116:1175-82.
- [Google Scholar]
- Health related quality of life in patients with idiopathic pulmonary fibrosis in clinical practice: Insights-IPF registry. Respir Res. 2017;18:139.
- [Google Scholar]
- Health-related quality of life of patients with idiopathic pulmonary fibrosis: A systematic review and meta-analysis. Eur Respir Rev. 2020;29:200154.
- [Google Scholar]
- The development and validation of the King’s brief interstitial lung disease (K-BILD) health status questionnaire. Thorax. 2012;67:804-10.
- [Google Scholar]
- Translation and validation of the King’s brief interstitial lung disease (K-BILD) questionnaire in French, Italian, Swedish, and Dutch. Chron Respir Dis. 2017;14:140-150.
- [Google Scholar]
- King’s brief interstitial lung disease questionnaire: Responsiveness and minimum clinically important difference. Eur Respir J. 2019;54:1900281.
- [Google Scholar]
- Quality of life assessment in interstitial lung diseases: a comparison of the disease-specific K-BILD with the generic EQ-5D-5L. Respir Res. 2018;19:101.
- [Google Scholar]
- The psychometric properties of the King’s brief interstitial lung disease questionnaire and thresholds for meaningful treatment response in patients with progressive fibrosing interstitial lung diseases. Eur Respir J. 2022;59:2101790.
- [Google Scholar]
- Patient-reported outcomes to assess dyspnoea in interstitial lung disease and pulmonary hypertension: A systematic literature review of measurement properties. Eur Respir Rev. 2022;31:220091.
- [Google Scholar]
- Patient-centered outcomes research in interstitial lung disease: an official american thoracic society research statement. Am J Respir Crit Care Med. 2021;204:e3-e23.
- [Google Scholar]
- Health-related quality of life in a multiracial Asian interstitial lung disease cohort. J Thorac Dis. 2022;14:4713-24.
- [Google Scholar]






