Translate this page into:
Whole-body 18F-fluorodeoxyglucose positron emission tomography-computed tomography (18F-FDG PET/CT) for staging locally advanced breast cancer: A prospective study from a tertiary cancer centre in south India
For correspondence: Dr Narendra Hulikal, Department of Surgical Oncology, Sri Venkateswara Institute of Medical Sciences, Tirupati 517 501, Andhra Pradesh, India e-mail: drnarendrah@yahoo.co.in
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Locally advanced breast cancer (LABC) is associated with substantial risk of occult metastases. The patients with LABC have high rate of systemic relapse, suggesting inadequacy of the current conventional staging in detecting the occult metastatic spread. 18F-fluorodeoxyglucose (FDG) positron emission tomography-computed tomography (PET/CT) is a new modality in the staging of breast cancer patients. Hence, this study was conducted to evaluate the role of 18F-FDG PET/CT in initial staging of LABC and to compare it with conventional methods.
Methods:
This prospective study included biopsy-confirmed female patients diagnosed with LABC meeting the selection criteria and attending surgical, medical and radiation oncology departments of a tertiary care centre in south India, from April 2013 to December 2014. Conventional workup included serum chemistry, mammogram, bone scan, contrast-enhanced CT (CECT) chest and upper abdomen and ultrasound abdomen and pelvis. All patients following conventional workup underwent 18F-FDG PET/CT.
Results:
In this study, 61 women with LABC underwent both conventional workup and 18F-FGD PET/CT. The 18F-FDG PET/CT, in comparison to conventional workup, revealed unsuspected N3 nodal disease in 11 more patients, revealed distant metastasis in seven more patients and also detected extra sites of metastasis in five patients. The sensitivity, specificity, positive predictive value, negative predictive value and accuracy of PET/CT to detect distant metastasis were 95, 98, 95, 98 and 97 per cent, respectively, whereas the sensitivity, specificity, positive predictive value, negative predictive value and accuracy of conventional imaging to detect distant metastasis were 65, 93, 81, 84 and 84 per cent, respectively.
Interpretation & conclusions:
The 18F-FDG PET/CT was found to be more accurate than conventional imaging for staging and modified stage and treatment in 30 and 38 per cent of patients, respectively. It was particularly useful in detecting occult distant metastasis and N3 nodal disease with an added advantage of examining whole body in single session. However, CECT chest was superior over 18F-FDG PET/CT for detecting pulmonary metastasis.
Keywords
Breast neoplasms
computed tomography
distant metastasis
18F-fluorodeoxyglucose
PET/CT
Breast cancer is the most common cancer among women in the developed world. Locally advanced breast cancer (LABC) poses a significant challenge to healthcare budget in the less developed world as it contributes to anywhere between 30 and 60 per cent of the total breast cancer patients1. According to the available data, the chance of harbouring occult metastasis in this subset of breast cancer patients is around 20 per cent2. Correct staging of disease in these patients is crucial from treatment point of view, healthcare costs and prognostication. At present patients clinically diagnosed with LABC are evaluated with the conventional tools consisting of contrast-enhanced computed tomography (CECT) of the chest and abdomen, a whole-body bone scintigraphy apart from the serum chemistry3. Following this initial staging, patients who staged LABC would undergo multimodal treatment consisting of neoadjuvant chemotherapy, surgery and radiation. In such patients, the initial extent of disease, defined by clinical examination and imaging studies, is a critical determinant of subsequent loco-regional therapeutic decisions. Therefore, women with LABC require careful, comprehensive workup before initiation of multimodality treatment. Further, LABC patients have high rate of systemic relapse during follow up, so the current conventional baseline staging evaluations are likely to underestimate the extent of disease4. Consequently, there is a need for more sophisticated staging procedures to exclude patients with metastatic disease from this aggressive treatment strategy in LABC. Studies have shown that positron emission tomography-computed tomography (PET/CT) can detect extra-axillary disease as well as occult systemic spread missed by the conventional staging methods567891011. Most of these studies are from western world, with only a few from India. The aim of this study was therefore, to evaluate the utility of 18F-fluorodeoxyglucose (18F-FDG) PET/CT in initial staging of LABC and to compare it with conventional methods.
Material & Methods
This prospective study was conducted at Sri Venkateswara Institute of Medical Sciences (SVIMS), Tirupati, Chittoor district, Andhra Pradesh, India from April 2013 to December 2014. The study protocol was approved by the institutional ethics committee and all participants gave written informed consent.
All consecutive female patients with the biopsy-proven, unilateral, newly diagnosed LABC [defined as those belonging to stage III, American Joint Committee on Cancer (AJCC/TNM), 7th edition, 201012 after conventional staging] presenting to surgical, medical or radiation oncology departments of SVIMS, Tirupati, during the study period were included. Those with early breast cancer, who have already received treatment elsewhere, male patients with breast cancer, and patients with LABC who did not give consent for the study, were excluded.
All patients presenting with clinical suspicion of LABC underwent initial core needle or incisional biopsy of the tumour for histological confirmation and immunohistochemistry for hormone receptor status, HER2/neu amplification and Ki-67 expression13. Tumour molecular subtype was classified as luminal-A (hormonal receptor positive, no HER2/neu overexpression and Ki-67 <14%); luminal-B (hormonal receptor positive with HER2/neu overexpression or Ki-67 >14%); HER2/neu rich (hormonal receptor negative with HER2/neu overexpression) and triple-negative [triple-negative breast cancer (TNBC)] when hormonal receptor and HER2/neu were negative14. The conventional staging included serum chemistry, mammo-sonogram of the breast, 99mTc-MDP bone scan, ultrasonography of the abdomen and pelvis and CECT chest and upper abdomen. All patients underwent whole-body 18F-FDG PET/CT (Biograph 6, Siemens, Germany). Patients were fasting for minimum 6 hours, and the blood glucose level was <160 mg/dl at the time of isotope injection. Ten milli-Curie of 18F-FDG was injected intravenously and the images were acquired after 60 minutes. No intravenous contrast was used, and 30 ml of oral contrast mixed in water was used. Imaging was done in supine position from vertex to the mid-thigh level with both the arms raised. The patients could breathe normally, and the first CT was performed with 5 mm cuts followed by PET acquisition every 2 min per bed position in three-dimensional mode. The images were fused and reviewed with TrueD Software (Siemens). The lesions were analyzed using maximum standardized uptake value (SUVmax). SUVmax was calculated using the formula based on body weight. The SUVmax was measured in breast tumour, regional lymph nodes and areas of metastasis. Extra-axillary lymph node involvement was confirmed using fine needle aspiration cytology (FNAC), and distant metastasis was confirmed with biopsy or FNAC wherever possible. When PET/CT or conventional imaging detected multiple lesions with typical appearance of metastases, such as lytic/blastic or mixed lesions in the skeleton, multiple lung nodules and multiple liver lesions, those were considered as distant metastases. When solitary lesion was detected, it was confirmed with histopathology wherever possible. Where lesion was solitary and biopsy was not possible, other sensitive imaging studies such as magnetic resonance imaging (MRI) of the spine were done.
Statistical analysis: Statistical analysis was done using IBM SPSS software version 20.0 (IBM Corp., Armonk, NY, USA). Median SUVmax and mean SUVmax were calculated. Mean SUVmax among various molecular subtypes was compared using ANOVA with post hoc analysis to look for significant association between them. Sensitivity, specificity, positive predictive value, negative predictive value and accuracy of conventional and PET/CT for staging were calculated.
Results
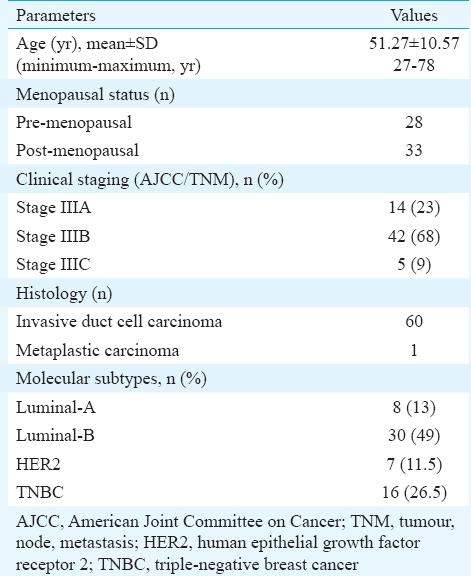
A total of 61 patients met the selection criteria and underwent both conventional staging and 18F-FDG PET/CT. The patient and tumour characteristics are given in Table I.
The 18F-FDG PET/CT detected primary site of cancer in all the patients and the SUVmax ranged from 3.5 to 42.6, with a median of 13.2 with interquartile range of 9.73-16.65. The mean SUVmax of the breast tumour was 14.69. The mean SUVmax of primary breast lesion among the molecular subtypes was luminal-A: 9.18, luminal-B: 14.39, Her-2: 14.38 and TNBC: 16.56. The mean SUVmax in TNBC patients was significantly higher than luminal-A patients (P=0.022). There was no significant difference among other molecular subtypes.
Of the 60 patients with clinically palpable axillary lymph node, eight patients showed no metabolic activity in the axillary lymph node. The sensitivity and specificity of PET/CT for detecting the axillary Level I and II lymph nodes were 87 and 100 per cent, respectively. The N3 disease was seen in 19 (31%) patients, and the sites were Level III axillary lymph node (LN) (N3a) alone in six, internal mammary (IM) and Level III axillary LN (N3b) in five, supraclavicular lymph node (SCLN)±IM or Level III LN in four and SCLN (N3c) alone in four patients. Confirmation of involvement for IM and Level III LN was based on imaging and FDG activity (SUVmax) and for SCLN was done by FNAC. PET/CT detected all 19 patients with N3 disease and revealed unsuspected N3 nodal in 11 (18%) additional patients not detected on conventional imaging. Among these 11 patients, three had distant metastasis, so PET/CT upstaged eight patients with stages IIIA/B to stage IIIC.
Distant metastasis: Occult distant metastasis was detected in 20 (33%) patients (Figure). The sites of metastasis were bone - 12, distant LN - 11, lung - 9, liver - 6 and brain - 1 as shown in Table II. Conventional imaging revealed metastasis in 16 patients, of whom three were false positive. It did not detect distant metastasis in seven (11.5%) patients (false negative) and they were all picked by 18F-FDG PET/CT. Among these seven patients, one had contralateral SCLN which was confirmed by FNAC, one had multiple liver metastasis, one had lytic bone lesions and the remaining four had multiple site metastasis. Of these seven patients, three had luminal-B tumours, two had TNBC tumours and one each had luminal-A and Her2/neu-rich tumours. Three patients were premenopausal, three were aged <50 yr, one was 55 yr old, and three were >60 yr. The 18F-FDG PET/CT detected distant metastasis in 20 patients, of whom one was falsely diagnosed as lung metastasis, which turned out to be abscess on biopsy. PET/CT was false negative in one patient which was detected by bone scan and was confirmed using magnetic resonance imaging (MRI) spine. In comparison to conventional workup, PET/CT detected additional sites of metastasis in five patients. PET/CT downstaged 5 per cent (n=3) of patients from stage IV to stage III. The comparison between conventional imaging and PET/CT to detect distant metastasis is given in Table III.
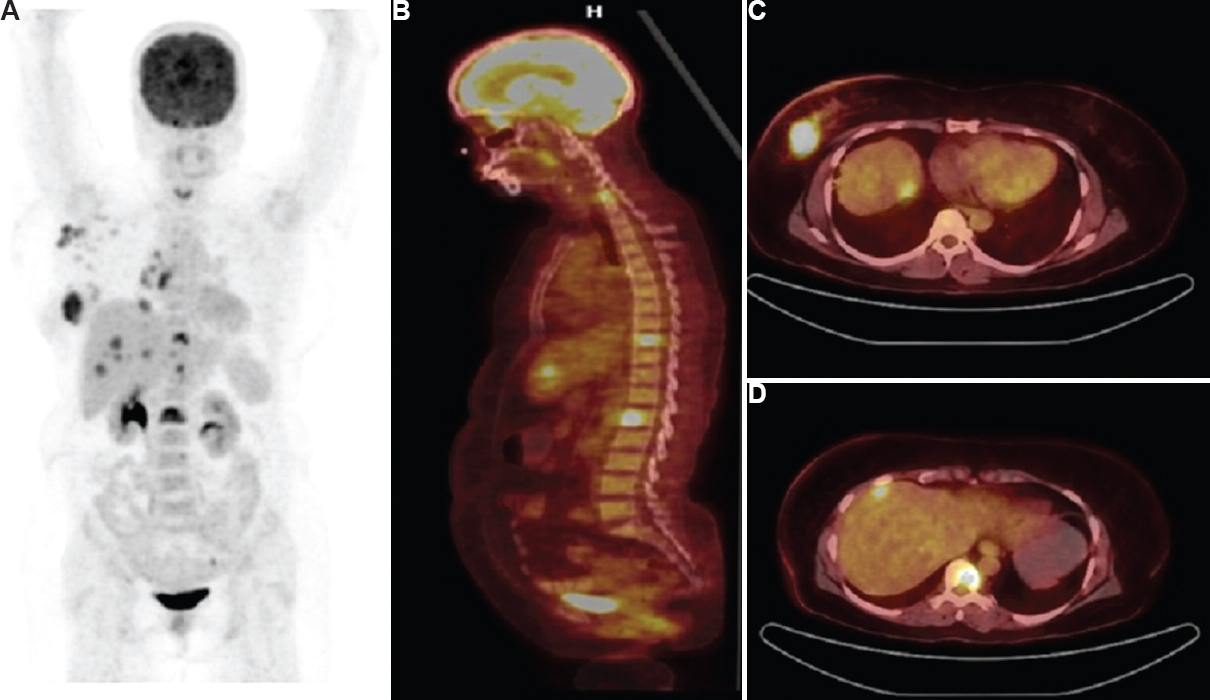
- (A) Maximal intensity projection image showing breast lesion with secondaries in spine and liver, (B) Sagittal positron emission tomography-computed tomography (PET/CT) image showing bone metastasis. Axial PET/CT images (C) showing primary in breast with liver metastasis, (D) lesion in vertebral body.
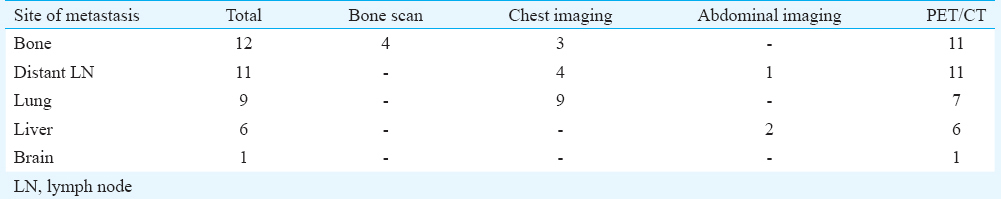

Comparison of 99mTc-MDP bone scan with 18F-FDG PET/CT: Bone was the common site of metastasis and was seen in 12 (20%) patients. Bone scan missed six patients with osteolytic and two patients with osteoblastic osseous metastasis, which were detected on 18F-FDG PET/CT. The bone scan had false-positive findings in three patients; the site of the lesion was spine in two cases and first costochondral junction in one patient. These lesions which were negative on PET/CT were further confirmed with MRI spine and CECT chest. The 18F-FDG PET/CT missed one osteoblastic metastasis, which was picked up by bone scan and further confirmed with MRI spine. The sensitivity, specificity, positive and negative predictive values and accuracy in diagnosing bone lesions were, respectively, 50, 94, 57, 85 and 82 per cent for bone scan and 92, 100, 100, 98 and 98 per cent for 18F-FDG PET/CT.
Comparison of CECT chest with 18F-FDG PET/CT for pulmonary metastasis: Pulmonary metastasis was present in nine (15%) patients, and all of them were diagnosed by the CECT chest. However, 18F-FDG PET/CT missed pulmonary metastasis in two patients. Since these two patients harboured additional distant visceral metastasis, this did not affect the staging. In one patient, PET/CT falsely characterized lung lesion as metastasis which was found to be abscess on biopsy. The sensitivity, specificity, positive predictive value, negative predictive value and accuracy for 18F-FDG PET/CT in diagnosing pulmonary lesions were 78, 98, 87.5, 96 and 95 per cent, respectively.
Other sites: The 18F-FDG PET/CT revealed distant lymph node involvement in 11 (18%) patients, of whom conventional imaging detected only in four (7%) patients. Mediastinal lymph node involvement was common and was seen in eight patients, contralateral axillary lymph node in five patients, cervical lymph nodes in two patients and abdominal lymph nodes in one patient. The hepatic metastasis was present in six (10%) patients. Conventional imaging showed solitary liver metastasis in two patients. The 18F-FDG PET/CT detected multiple liver lesions in these two patients, in addition to detecting liver metastasis in four more patients. The PET/CT also detected brain metastasis in one patient.
Thus, 18F-FDG PET/CT changed stage in 18 patients (30%); eight were upstaged from IIIA/B to stage IIIC, seven to stage IV and three were downstaged from stage IV to stage III. Further, 18F-FDG PET/CT changed treatment plan in 23 (38%) patients. These were 18 patients as mentioned above and another five patients, in whom PET/CT revealed additional sites of metastasis.
Discussion
The National Comprehensive Cancer Network guidelines in oncology13 recommend 18F-FDG PET/CT as category 2B option for the workup of a patient with LABC. The panel also advocates the performance of PET/CT, particularly in patients with equivocal or suspicious findings on standard staging studies13. One of the reasons for not advocating the routine use of the PET/CT is the lack of data showing clinical benefit. With the proven superiority of combined PET/CT over PET1516, the emerging data on combined PET/CT can change the future guidelines. In comparison to conventional tools, PET/CT is a sensitive tool with reported advantages of the detection of occult metastasis, extra-axillary nodal disease and incidental second primaries7891011.
In this study, significant 18F-FDG uptake was seen in all primary breast lesions with sensitivity of 100 per cent and this was comparable to the previous studies781017. There was significantly higher 18F-FDG uptake in TNBC patients when compared with luminal-A, as was evident in other studies1819. This may be because of larger size, higher proliferation and poor differentiation of TNBC tumours20. There was no significant difference in 18F-FDG uptake among other subtypes.
As already known, PET/CT had difficulty in diagnosing involved axillary lymph nodes because of micrometastases. In this study, the sensitivity and specificity for detecting axillary Level I and II lymph nodes were 87 and 100 per cent, respectively. The sensitivity was higher than the study by Fuster et al8, which showed sensitivity of 70 per cent and specificity of 100 per cent. In a meta-analysis, Cooper et al21 noted across seven studies of PET/CT (n=862) that mean sensitivity was 56 per cent (range, 44-67%) and mean specificity was 96 per cent (range, 90-99%). The reported higher sensitivity in the present study might be attributed to higher risk among LABC patients to harbour lymph nodal metastasis. PET/CT was superior to conventional imaging in detecting the extra-axillary lymph node involvement as it was evident from the previous studies781011. In our study, PET/CT upstaged 13 per cent of patients to stage IIIC. This information also helped in planning the loco-regional treatment such as altering radiation field to include infraclavicular, IM or supraclavicular area.
In LABC, detection of occult metastasis has an impact on prognosis and treatment options. The patients with metastasis can be spared of aggressive multimodality treatment, and palliative local therapy such as radiotherapy for bone metastasis or radiofrequency ablation of liver lesions can be offered. In our study, 33 per cent of the patients had distant metastasis; PET/CT revealed occult metastasis in 11.5 per cent of the patients which were missed on conventional imaging. It also showed additional sites of metastases in eight per cent of patients who were harbouring metastasis on conventional workup. In a study of 117 patients with LABC, Groheux et al10 reported that 15 (13%) cases of distant metastasis were unsuspected before FDG-PET/CT. Manohar et al11 showed the presence of distant metastasis in 10 of 43 patients, who otherwise were negative on conventional imaging. In the present study, the PET/CT down-staged three patients from stage IV to stage III. High sensitivity, specificity, positive predictive value and negative predictive values for PET/CT have been reported in earlier studies also8911.
In the evaluation of osseous metastasis, PET/CT outperformed bone scintigraphy. This can be explained by the higher pick up rate of the lytic osseous metastasis with PET/CT, which are often missed by the conventional bone scan1022. Although the blastic metastasis has lower metabolic activity and is frequently undetected on PET alone, the CT component detects sclerosis222324252627. For pulmonary parenchyma, although PET/CT efficiently detects nodules of more than 1 cm size, because of the partial volume effect and respiratory movements, PET lacks sensitivity for smaller nodules28. Further, free-breathing CT as used in the PET/CT is less efficient than the standard diagnostic thoracic CT1028 in diagnosing pulmonary metastasis. This explains our finding of superiority of CECT over PET/CT in the diagnosis of pulmonary metastasis. In 18F-FDG PET/CT, use of intravenous contrast and breath hold during acquisition of chest images may yield results equivalent to that of CECT chest and may be considered. Though 18F-FDG PET/CT detected brain metastasis in a single patient in our study, this is not the ideal tool for picking up such metastasis due to high background activity and MRI is often preferred. Further, PET/CT was superior in detecting distant lymph node involvement as was evident in other studies10. In comparison to conventional tools, 18F-FDG PET/CT identified unsuspected liver lesions in four patients and additional liver lesions in two patients diagnosed to have solitary liver metastasis.
Our study had some limitations. Though the calculated sample size was 139, during the study period, 91 patients with LABC presented, of whom only 61 patients met the selection criteria. Low sample size was the major limitation of the study. Though it is known that age and menopausal status influence the prognosis of breast cancer, these might not have impacted the results of staging, and since the number was small, the results were not specifically analysed with respect to either age or menopausal status.
In conclusion, our findings showed that 18F-FDG PET/CT was more accurate than conventional imaging for staging of cancer. It altered stage and plan of treatment in 30 and 38 per cent of patients, respectively. It was particularly useful in detecting occult distant metastasis and N3 nodal disease with an added advantage of examining whole body in a single session. With respect to detection of pulmonary metastasis, 18F-FDG PET/CT missed two of the nine lesions, all of which were picked by CECT chest.
Acknowledgment
The authors acknowledge the Prandhanam Scheme of the SVIMS-Tirumala Tirupati Devastanams, Tirupati, for providing facility for free PET/CT for patients.
Financial support & sponsorship: None
Conflicts of Interest: None.
References
- Clinical and pathological response rates of docetaxel-based neoadjuvant chemotherapy in locally advanced breast cancer and comparison with anthracycline-based chemotherapies: Eight-year experience from single centre. Indian J Cancer. 2011;48:410-4.
- [Google Scholar]
- Evaluation of patients for metastasis prior to primary therapy. In: Harris JR, Lippman ME, Morrow M, Osborne CK, eds. Diseases of the breast (4th ed). Philadelphia: Lippincott Williams & Wilkins; 2010. p. :483.
- [Google Scholar]
- Workup and staging of locally advanced breast cancer. Semin Radiat Oncol. 2009;19:211-21.
- [Google Scholar]
- Prevalence of overt metastases in locally advanced breast cancer. Clin Oncol (R Coll Radiol). 2008;20:340-4.
- [Google Scholar]
- Fluorine-18 2-deoxy-2-fluoro-D-glucose PET in the preoperative staging of breast cancer: Comparison with the standard staging procedures. Eur J Nucl Med. 2001;28:351-8.
- [Google Scholar]
- Comparison between positron emission tomography using 2-[fluorine-18]fluoro-2-deoxy-D-glucose, conventional imaging and computed tomography for staging of breast cancer. Ann Oncol. 2008;19:1249-54.
- [Google Scholar]
- Effect of (18)F-FDG PET/CT imaging in patients with clinical stage II and III breast cancer. Int J Radiat Oncol Biol Phys. 2008;71:695-704.
- [Google Scholar]
- Preoperative staging of large primary breast cancer with [18F]fluorodeoxyglucose positron emission tomography/computed tomography compared with conventional imaging procedures. J Clin Oncol. 2008;26:4746-51.
- [Google Scholar]
- 18F-2-fluoro-2-deoxy-d-glucose positron emission tomography in staging of locally advanced breast cancer. J Clin Oncol. 2004;22:1253-9.
- [Google Scholar]
- 18F-FDG PET/CT in staging patients with locally advanced or inflammatory breast cancer: Comparison to conventional staging. J Nucl Med. 2013;54:5-11.
- [Google Scholar]
- Role of 18F-FDG PET/CT in identifying distant metastatic disease missed by conventional imaging in patients with locally advanced breast cancer. Nucl Med Commun. 2013;34:557-61.
- [Google Scholar]
- Edge SB, Byrd DR, Compton CC, Fritz AG, Greene F, Trotti A, eds. AJCC Cancer Staging Manual (7th ed). New York: Springer; 2010. p. :347.
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Breast Cancer, V 2.2016. Available from: https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf
- Strategies for subtypes - dealing with the diversity of breast cancer: Highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22:1736-47.
- [Google Scholar]
- Initial experience with FDG-PET/CT in the evaluation of breast cancer. Eur J Nucl Med Mol Imaging. 2006;33:254-62.
- [Google Scholar]
- Performance of 2-deoxy-2-[F-18]fluoro-D-glucose positron emission tomography and integrated PET/CT in restaged breast cancer patients. Mol Imaging Biol. 2005;7:369-76.
- [Google Scholar]
- The role of (18)F-FDG PET/CT in initial staging of patients with locally advanced breast carcinoma with an emphasis on M staging. Hell J Nucl Med. 2011;14:135-9.
- [Google Scholar]
- Comparison of triple-negative and estrogen receptor-positive/progesterone receptor-positive/HER2-negative breast carcinoma using quantitative fluorine-18 fluorodeoxyglucose/positron emission tomography imaging parameters: A potentially useful method for disease characterization. Cancer. 2008;112:995-1000.
- [Google Scholar]
- Correlation of high 18F-FDG uptake to clinical, pathological and biological prognostic factors in breast cancer. Eur J Nucl Med Mol Imaging. 2011;38:426-35.
- [Google Scholar]
- Characteristics and outcomes according to molecular subtypes of breast cancer as classified by a panel of four biomarkers using immunohistochemistry. Breast. 2012;21:50-7.
- [Google Scholar]
- Positron emission tomography (PET) for assessment of axillary lymph node status in early breast cancer: A systematic review and meta-analysis. Eur J Surg Oncol. 2011;37:187-98.
- [Google Scholar]
- Detection of bone metastases in breast cancer by 18FDG PET: Differing metabolic activity in osteoblastic and osteolytic lesions. J Clin Oncol. 1998;16:3375-9.
- [Google Scholar]
- Comparison of FDG PET and SPECT for detection of bone metastases in breast cancer. AJR Am J Roentgenol. 2005;184:1266-73.
- [Google Scholar]
- Additional value of PET-CT in staging of clinical stage IIB and III breast cancer. Breast J. 2010;16:617-24.
- [Google Scholar]
- The role of 18F-fluoride PET-CT in the detection of bone metastases in patients with breast, lung and prostate carcinoma: A comparison with FDG PET/CT and 99mTc-MDP bone scan. Jpn J Radiol. 2013;31:262-9.
- [Google Scholar]
- Comparison of FDG-PET/CT and bone scintigraphy for detection of bone metastases in breast cancer. Acta Radiol. 2011;52:1009-14.
- [Google Scholar]
- Integrated positron emission tomography/computed tomography may render bone scintigraphy unnecessary to investigate suspected metastatic breast cancer. J Clin Oncol. 2010;28:3154-9.
- [Google Scholar]
- Performance of FDG PET/CT in the clinical management of breast cancer. Radiology. 2013;266:388-405.
- [Google Scholar]






