Translate this page into:
Vitamin D levels in Indian children with intrathoracic tuberculosis
Reprint requests: Dr Rakesh Lodha, Additional Professor, Department of Pediatrics, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110 029, India e-mail: rlodha1661@gmail.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Deficiency of vitamin D, an immunomodulator agent, is associated with increased susceptibility to tuberculosis in adults, but only limited studies are available in the paediatric age group, especially regarding association of vitamin D with type and outcome of tuberculosis. We conducted this study to determine the baseline 25-hydroxy vitamin D levels in children suffering from intrathoracic tuberculosis and its association with type and outcome of tuberculosis.
Methods:
Children with intrathoracic tuberculosis, diagnosed on the basis of clinico-radiological criteria, were enrolled as part of a randomized controlled trial on micronutrient supplementation in paediatric tuberculosis patients. Levels of 25-hydroxy vitamin D were measured in serum samples collected prior to starting antitubercular therapy by chemiluminescent immunoassay technology.
Results:
Two hundred sixty six children (mean age of 106.9 ± 43.7 months; 57.1% girls) were enrolled. Chest X-ray was suggestive of primary pulmonary complex, progressive disease and pleural effusion in 81 (30.5%), 149 (56%) and 36 (13.5%) subjects, respectively. Median serum 25-hydroxy vitamin D level was 8 ng/ml (IQR 5, 12). One hundred and eighty six (69.9%) children were vitamin D deficient (serum 25-hydroxy vitamin D <12 ng/ml), 55 (20.7%) were insufficient (12 to <20 ng/ml) and 25 (9.4%) were vitamin D sufficient (≥ 20 ng/ml). Levels of 25-hydroxy vitamin D were similar in all three types of intrathoracic tuberculosis, and in microbiologically confirmed and probable cases. Levels of 25-hydroxy vitamin D did not significantly affect outcome of the disease. Children who were deficient or insufficient were less likely to convert (become smear/culture negative) at two months as compared to those who were 25-hydroxy vitamin D sufficient (P<0.05).
Interpretation & conclusions:
Majority of Indian children with newly diagnosed intrathoracic tuberculosis were deficient in vitamin D. Type of disease or outcome was not affected by 25-hydroxy vitamin D levels in these children. However, children who did not demonstrate sputum conversion after intensive phase of antitubercular therapy had lower baseline 25-hydroxy vitamin D levels as compared to those who did.
Keywords
Antituberculosis therapy
children
intrathoracic tuberculosis
pediatric
vitamin D
Tuberculosis (TB) continues to be a major public health problem, especially in developing countries and South East Asia Region. India alone accounted for an estimated one quarter (26%) of the global TB burden in 201012. The biologically active form of vitamin D- 1, 25-dihydroxy vitamin D has been shown to affect innate immunity by modulating macrophage function; this may enhance protection against tuberculosis infection34. Vitamin D also upregulates antimicrobial peptide cathelicidin and enhances killing of intracellular M. tuberculosis. In the absence of adequate vitamin D levels, triggering of toll-like receptors of macrophage by M. tuberculosis antigen results in impaired production of cathelicidin56.
If one considers that the deficient immuno-modulatory function in states of vitamin D deficiency increases the risk of tuberculosis, the pertinent question arises whether there is any link between the levels of deficiency and extent or severity of tubercular disease. The next relevant issue is whether vitamin D deficiency has any detrimental effect on the response and outcome of standard anti-tubercular therapy. The answers to these queries could direct us in planning vitamin D supplementation in TB patients and also in deciding whether all levels of deficiency of vitamin D need to be corrected. There are only a few studies which have addressed these issues, none so in the paediatric population.
With this background, 25-hydroxy vitamin D levels were measured in children who had been enrolled in a randomized controlled trial (RCT) to study the effect of micronutrient supplementation in paediatric intrathoracic tuberculosis. The objective of this study was to evaluate the association of low serum 25-hydroxy vitamin D levels with the types and outcome of intrathoracic tubercular disease.
Material & Methods
This study was conducted in 266 children enrolled in a placebo controlled, randomized controlled trial on micronutrient supplementation in children with intrathoracic tuberculosis. All consecutive children of either sex, between 6 months to 15 yr of age, suffering from probable pulmonary and/or pleural tuberculosis were recruited in 2009-2011 from the Paediatric TB Clinic of two tertiary care centres of New Delhi (All India Institute of Medical Sciences and Kalawati Saran Children Hospital); ethical approval was obtained from both institutions. Diagnosis of probable intrathoracic tuberculosis was based on clinico-radiological criteria7. After obtaining written informed consent from the parents, children with probable TB were enrolled in the study.
Induced sputum and gastric lavages were collected on two consecutive days and examined for acid fast bacilli (AFB) by Ziehl-Neelsen (Z-N) staining and cultured on automated BACTEC-MGIT 960 system, (Becton, Dickinson & Company, USA). Cell count, biochemistry, Z-N stain, and culture for AFB and bacteria were performed on pleural fluid. The procedures were performed at both the sites. Pleural fluid was collected from children who had a pleural effusion.
Based on chest X-ray findings, children with probable intrathoracic tuberculosis were categorized into three categories: primary pulmonary complex (PPC), progressive pulmonary disease (PPD) and pleural effusion (PE)7. PPC included lymph node with small alveolar shadow; PPD group included consolidation, cavitatory lesion, miliary tuberculosis and multiple mediastinal adenopathy with or without parenchymal lesion.
Outcome of antitubercular therapy was measured in two groups: cured and extension of therapy. Children were declared “cured”, if there was significant resolution of radiologic findings (>2/3rd) and symptoms at six months of therapy and the treatment was discontinued. Extension of therapy included children whose category I therapy was extended or changed to category II/ second line antitubercular drugs for persistent symptoms or poor resolution of radiographic findings. Induced sputum/ gastric lavage conversion at two months was also assessed in the group of children who had a microbiological confirmation of diagnosis at baseline. All children with diagnosis of tuberculosis were treated with daily antitubercular therapy and were monitored as per standardized protocol8. Detailed history, clinical examination and anthropometric measurements were recorded for all enrolled patients.
Measurement of 25-hydroxy vitamin D: Levels of 25-hydroxy vitamin D were measured together for all samples after the RCT had ended. About 3 ml blood was collected prior to starting antitubercular therapy in plain zinc free tubes for micronutrient estimation. Serum was separated within one hour and one aliquot of 300 μl was stored at -20°C till further analysis. Similar sample collections were also performed at two and six months of therapy. Levels of 25-hydroxy vitamin D levels were measured from the stored serum samples by chemiluminescent immunoassay (CLIA) technology using Liaison® 310600 system (DiaSorin Inc; USA) following the manufacturer's protocol9. The analytical measurement range for the DiaSorin LIAISON 25-hydroxy vitamin D Total Assay is 4 to 150 ng/ml. The lowest reportable value is 4 ng/ml, based on an inter-assay precision that approximates 20 per cent CV.
Statistical analysis: Children were classified into three groups according to circulating 25-hydroxy vitamin D levels. Those with serum 25-hydroxy vitamin D level <12 ng/ml were grouped as deficient, 12 to <20 ng/ml as insufficient and ≥20 ng/ml as sufficient10. Analysis was done using the software Stata, version 9 (STATA Corp, College Station, TX, USA). Chi-squared/Fisher's exact test and ANOVA were used for categorical and continuous variables as appropriate. The baseline 25-hydroxy vitamin D levels were log transformed and then we calculated the geometric mean and 95% confidence intervals. Height-for-age (HA) and weight-for-age (WA) ‘Z’ scores were computed using the nutritional anthropometry module of Epi Info version 5 software (Centers for Disease Control and Prevention, Atlanta, US), based on the National Center for Health Statistics (NCHS) - WHO reference curves11. The association between the baseline 25-hydroxy vitamin D levels and the outcome was assessed. In the trial, 140 children received vitamin D supplementation while others did not. To adjust for the influence of other factors such as vitamin D supplementation, age, gender, M. tuberculosis positivity, weight-for-age Z-score, 25-hydroxy vitamin D levels at two and six months, the category of antitubercular therapy received (Cat I or Cat III)8 Cox's proportional hazard regression model was performed with 25-hydroxy vitamin D level as a time-dependent covariate; except in children who died, the outcome (cure) was assessed at 6 months of antitubercular therapy.
Results
Characteristics of the study population: This study included 266 children (152, 57.1% females) with probable intrathoracic tuberculosis. The mean age was 106.9 ± 43.7 months. Most children were vaccinated with BCG (75.9%); 97 (36.5%) children had positive history of contact with tuberculosis patient. Chest X-ray was suggestive of primary pulmonary complex (PPC), progressive pulmonary disease (PPD) and pleural effusion in 81 (30.5%), 149 (56%) and 36 (13.5%) subjects, respectively. Microbiological confirmation for Mycobacterium tuberculosis by positive MGIT culture was obtained in 94 (35.3%) cases.
Baseline serum 25-hydroxy vitamin D levels: Median serum 25-hydroxy vitamin D level was 8 ng/ml (IQR 5, 12). One hundred and eighty six (69.9%) children were vitamin D deficient (serum 25-hydroxy vitamin D <12 ng/ml), 55 (20.7%) were insufficient (12 to <20 ng/ml) and only 25 (9.4%) were vitamin D sufficient (≥ 20 ng/ml). The median (IQR) baseline serum 25-hydroxy vitamin D levels in girls were lower [7 (5, 11) ng/ml] as compared to boys [10 (6, 14) ng/ml]; P<0.01. The 25-hydroxy vitamin D levels were not different in the severely underweight and stunted children as compared to the well nourished ones.
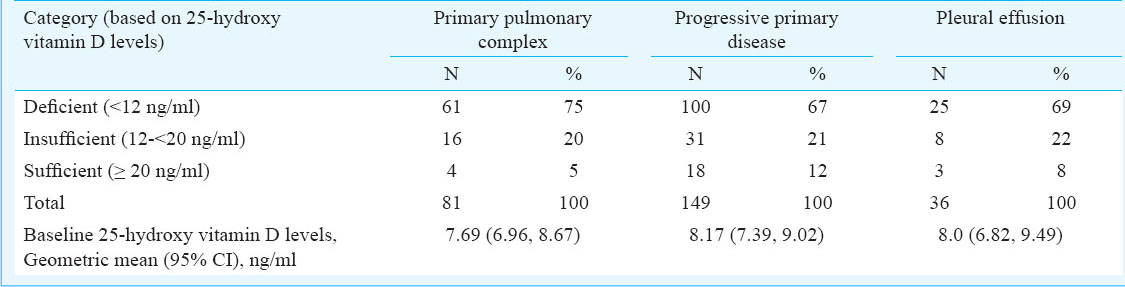
Association of baseline serum 25-hydroxy vitamin D levels with type of intrathoracic TB: Of the 81 primary pulmonary complex cases, 75 per cent had a deficient 25-hydroxy vitamin D level as compared to 67 per cent of progressive pulmonary disease cases and 69 per cent of pleural effusion cases (Table I). The geometric mean (95% CI) of baseline 25-hydroxy vitamin D levels in children with PPC, PPD and PE were 7.69 (6.96, 8.67), 8.17 (7.39, 9.02) and 8.0 (6.82, 9.49) ng/ml, respectively. There was no significant difference in 25-hydroxy vitamin D levels between microbiologically confirmed TB and probable TB cases; median (IQR) 25-hydroxy vitamin D levels in both groups being 8 (5.5, 12.5) and 8.5 (5, 12) ng/ml, respectively.
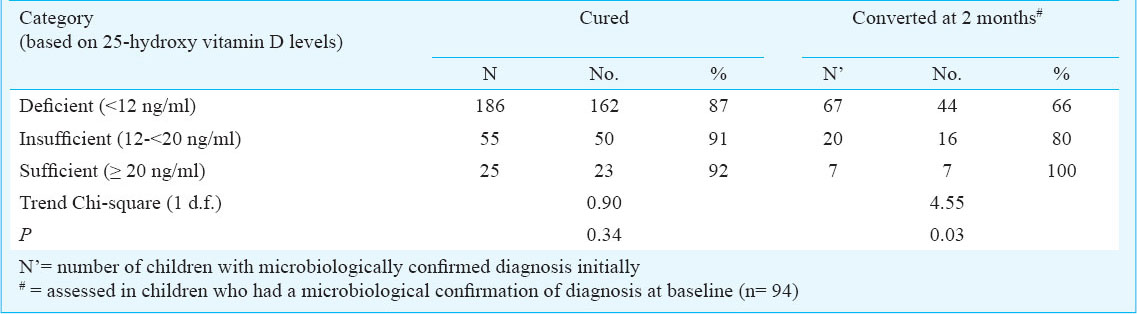
Association of baseline serum 25-hydroxy vitamin D levels with outcomes of intrathoracic TB: Thirty one children needed extension/change of therapy or died; their median (IQR) baseline 25 hydroxy vitamin D serum level was 6 (5, 11) ng/ml as compared to 8 (5, 13) ng/ml in 235 children who were cured. The children who did not demonstrate sputum conversion after intensive phase of antitubercular therapy had lower median (IQR) baseline 25-hydroxy vitamin D levels [7 (5, 9) ng/ml; n=27] as compared to those who did [9 (6, 14) ng/ml; n=67]; P<0.05. Table II shows the proportions of the patients who were cured and those who converted at two months in the three categories based on baseline 25-hydroxy vitamin D levels; children who were deficient or insufficient were less likely to convert at two months as compared to those who were 25-hydroxy vitamin D sufficient.
The median (IQR) serum 25-hydroxy vitamin D levels at two months were comparable in children who needed extension/change of therapy [7 (5, 14) ng/ml; n=17] as compared to children who were cured [9 (6, 17) ng/ml; n=175]. However, the median (IQR) serum 25-hydroxy vitamin D levels at six months were lower in children who needed extension of therapy [5 (4, 9) ng/ml; n=15] as compared to children who were cured [9 (5- 15) ng/ml; n=175]; P<0.05.
Association of vitamin D supplementation with outcomes of intrathoracic TB: One hundred forty (52.6%) children received vitamin D supplementation in the trial. Hypovitaminosis D (25-hydroxy vitamin D < 20 ng/ml) at baseline was documented in 126 of 140 (90%) children who received vitamin D and in 114 of 126 (90.4%) who did not. The median (IQR) 6-month serum 25-hydroxy vitamin D levels were higher in the supplemented group [10 (6, 21.5) ng/ml; n=97] as compared to those who did not receive vitamin D [6 (4, 11) ng/ml; n=93]; P<0.0001. In the vitamin D supplemented group, 87 of 99 (87.9%) of the vitamin D deficient children were cured at six months as compared to 27 of 28 (96.4%) of vitamin D insufficient children and 12 of 13 (92.3%) of vitamin D sufficient children. Similarly, in children who did not receive vitamin D supplementation, 75 of 87 (86.2%) of the vitamin D deficient children were cured at six months as compared to 23 of 27 (85.1%) of vitamin D insufficient children and 11 of 12 (91.7%) of vitamin D sufficient children. There was no association between the outcome and baseline 25-hydroxy vitamin D levels in the sub-groups by supplementation.
On Cox's proportional hazard regression model, baseline 25-hydroxy vitamin D status, age, gender, M. tuberculosis positivity, weight for age Z-score, vitamin D supplementation received, the serum 25-hydroxy vitamin D level at baseline, two months and at six months as a time dependent variable, and the category of antitubercular therapy received (Cat I or Cat III) did not influence the outcome.
Discussion
Our study showed that baseline serum 25-hydroxy vitamin D levels in children with intrathoracic tuberculosis were not different in different types/ categories of disease. The children who were cured, had higher median 25-hydroxy vitamin D levels at baseline, two and six months as compared to children who needed extension/change of therapy; however, using the Cox's proportional hazard regression model, no association was observed. The children who remained positive for M. tuberculosis in respiratory samples at the end of two months of therapy had lower baseline 25-hydroxy vitamin D levels as compared to those who showed conversion.
Most of the studies conducted in adult population have suggested that 25-hydroxy vitamin D levels are lower in individuals with tuberculosis121314151617. A study done by Ho-Pham et al12 on Vietnamese population showed that prevalence of vitamin D insufficiency was 35.4 and 45.3 per cent in men and women with TB, respectively. Other studies done on Africans, Pakistani, Ugandan, Gujarati Asians in West London and immigrant population from Sub-Saharan Africa living in Australia also suggested that 25-hydroxy vitamin D levels were low in adult TB patients14151617. Studies from paediatric population are scarce, but those available show lower 25-hydroxy vitamin D levels in children with tuberculosis as compared to controls181920. A study done by Genmaa et al20 showed that 25-hydroxy vitamin D levels were low (<20 ng/ml) in Mongolian children with tuberculosis (7 ± 4 ng/ml). Likewise, another study which was done in Australia included refugee children and showed that 25-hydroxy vitamin D levels were significantly lower in children with latent tuberculosis and TB infection (64.2 and 81.8%, respectively)21.
Our study also showed that most of the children with intrathoracic tuberculosis were either vitamin D deficient (69.9%) or insufficient (20.7%). We are unable to comment whether this is because of association of low 25-hydroxy vitamin D levels with tuberculosis or simply reflects the vitamin D deficient or insufficient status of the general population. It has been reported that 75-85 per cent of Indian school-going children have vitamin D deficiency or insufficiency22.
Many studies have evaluated the association of tuberculosis with low serum vitamin level and the immunomodulatory effects of vitamin D. But there are no reports available on association of severity of vitamin D deficiency and types of tubercular disease in children. A study conducted on South Korean adults showed that baseline serum 25-hydroxy vitamin D levels were low in all patients with tuberculosis and levels did not differ between patients with pulmonary and extrapulmonary tuberculosis23. In our study, we did not observe any difference in the serum levels of 25-hydroxy vitamin D in the three types of the tuberculosis (PPC, PPD and PE).
There has been speculation on whether vitamin D supplementation can hasten the cure of tuberculosis when used in conjunction with standard antitubercular therapy. If 25-hydroxy vitamin D levels can be shown to have any correlation with the outcome of tubercular disease, this mode of intervention may be logical. In our study, a relation was observed between sputum conversion at two months with the baseline 25-hydroxy vitamin D levels. We observed lower baseline 25-hydroxy vitamin D levels in children who did not show sputum conversion than who did. There are a few other studies which have looked into this aspect of relationship between vitamin D and tuberculosis and they have also displayed a poor outcome in the 25-hydroxy vitamin D deficient population. A Japanese study conducted by Sato et al24 has suggested that low serum 25-hydroxy vitamin D level may not only increase the risk of developing active TB but may also be related to the poor treatment outcomes, which was measured by time taken to obtain three consecutive negative sputum smears or TB bacteria cultures. This study included only 38 subjects with tuberculosis and because of small sample size, results of this study cannot be extrapolated to whole population. Rathored et al25 studied 354 multidrug resistant (MDR) and 338 drug sensitive Indian TB patients and found that 25-hydroxy vitamin D concentrations were lower in MDR group than the drug sensitive TB patients. Also in MDR-TB, smear conversion time was negatively correlated with 25-hydroxyvitamin D (Spearman's ρ coefficient −0.14, P=0.03), but culture conversion time did not show any such significant relationship25. An older Indonesian study on 40 patients of pulmonary tuberculosis documented that the disease was less extensive in patients who had higher 25-hydroxy vitamin D levels26. Sputum conversion rate at two months have been considered as a predictor of relapse of tuberculosis in adults with longer time to conversion being associated with higher relapse rates2728.
Since this study was a subset of a randomized control trial, almost half of children received vitamin D as a part of micronutrient supplementation. This supplementation did not affect the outcome or influence the effect of vitamin D deficiency as demonstrated by multivariate analysis. Our children were biochemically deficient/insufficient in vitamin D, but they did not manifest as clinical rickets. None of these children were given therapeutic vitamin D supplementation as all assays were done after the completion of clinical trial and the children did not have clinical signs/symptoms of rickets.
The strengths of this study included a large sample size and the use of a sensitive technique for 25-hydroxy vitamin D level estimation. But the study had some limitations. We did not estimate vitamin D intake, duration of sun exposure and degree of skin pigmentation, all of which might have helped in explaining the low serum 25-hydroxy vitamin D levels. The study was carried out in children enrolled in a randomized controlled trial and not as an independent study. We did not enrol healthy controls, which would have helped us determine the role of low 25-hydroxy vitamin D levels in predisposing to development of tuberculosis in children. The number of children with poor outcome was small; a much larger sample size will be needed to have the appropriate power to determine the differences in vitamin D status.
In conclusion, majority of the enrolled children with microbiologically confirmed and probable intrathoracic tuberculosis demonstrated low serum levels of 25-hydroxy vitamin D (deficient and insufficient levels) and the levels were not associated with type and outcome of TB. However, children who did not demonstrate sputum conversion after intensive phase of antitubercular therapy had lower baseline 25-hydroxy vitamin D levels as compared to those who did.
Acknowledgment
Authors thank Prof. R.M. Pandey, Head, Department of Biostatistics, All India Institute of Medical Sciences, New Delhi, for his advice in statistical analysis. Funding from the Norwegian Programme for Development, Research and Education NUFUPRO-2007/10183 and the Research Council of Norway (GLOBVAC), is duly acknowledged.
References
- WHO. World Health Organization TB Report, 2011; Global tuberculosis control. Geneva: WHO; 2011.
- [Google Scholar]
- World Health Organisation, Tuberculosis Control in the South-East Asia Region. The Regional Report. New Delhi: WHO SEARO; 2012.
- [Google Scholar]
- Cutting edge: Vitamin D-mediated human antimicrobial activity against Mycobacterium tuberculosis dependent on the induction of cathelicidin. J Immunol. 2007;179:2060-3.
- [Google Scholar]
- Vitamin D, vitamin D receptor, and cathelicidin in the treatment of tuberculosis. Vitam Horm. 2011;86:307-25.
- [Google Scholar]
- Essentials of tuberculosis in children. (3rd ed). New Delhi: Jaypee Brothers Medical Publishers; 2011.
- [Google Scholar]
- Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare. Management of pediatric tuberculosis under the Revised National Tuberculosis Control Program (RNTCP) Indian Pediatr. 2004;41:901-5.
- [Google Scholar]
- Liaison® lab manual. Available from: http://labmed.ucsf.edu/labmanual/db/resource/proc-25OHVitDTotal.pdf
- [Google Scholar]
- Institute of Medicine. Dietary reference intakes for calcium and vitamin D. Washington DC, USA: National Academies Press; 2011.
- [Google Scholar]
- Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data 2005-2006. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2006.
- [Google Scholar]
- Association between vitamin D insufficiency and tuberculosis in a Vietnamese population. BMC Infect Dis. 2010;10:306.
- [Google Scholar]
- Vitamin D and calcium levels in Ugandan adults with human immunodeficiency virus and tuberculosis. Int J Tuberc Lung Dis. 2011;15:1522-7.
- [Google Scholar]
- Prevalence of vitamin D deficiency in adult tuberculosis patients at a central hospital in Malawi. Int J Tuberc Lung Dis. 2011;15:408-10.
- [Google Scholar]
- Vitamin D deficiency and tuberculosis progression. Emerg Infect Dis. 2010;16:853-5.
- [Google Scholar]
- Influence of vitamin D deficiency and vitamin D receptor polymorphisms on tuberculosis among Gujarati Asians in west London: a case-control study. Lancet. 2000;355:618-21.
- [Google Scholar]
- Vitamin D deficiency is associated with tuberculosis and latent tuberculosis infection in immigrants from Sub-Saharan Africa. Clin Infect Dis. 2008;46:443-6.
- [Google Scholar]
- Low serum vitamin D levels and tuberculosis: a systematic review and meta-analysis. Int J Epidemiol. 2008;37:113-9.
- [Google Scholar]
- Vitamin D deficiency and insufficiency in children with tuberculosis. Pediatr Infect Dis J. 2010;27:941-2.
- [Google Scholar]
- Vitamin D, tuberculin skin test conversion, and latent tuberculosis in Mongolian school-age children: a randomized, double-blind, placebo-controlled feasibility trial. Am J Clin Nutr. 2012;96:391-6.
- [Google Scholar]
- Vitamin D and tuberculosis status in refugee children. Pediatr Infect Dis J. 2012;31:521-3.
- [Google Scholar]
- Vitamin D status in India - its implication and remedial measures. J Assoc Physicians India. 2009;57:40-8.
- [Google Scholar]
- Vitamin D deficiency and changes in serum vitamin D levels with treatment among tuberculosis patients in South Korea. Respir. 2012;17:808-13.
- [Google Scholar]
- The relationship between 25-hydroxyvitamin D levels and treatment course of pulmonary tuberculosis. Respir Investig. 2012;50:40-5.
- [Google Scholar]
- Risk and outcome of multidrug-resistant tuberculosis: vitamin D receptor polymorphisms and serum 25(OH)D. Int J Tuberc Lung Dis. 2012;16:1522-8.
- [Google Scholar]
- A study of vitamin D levels in Indonesian patients with untreated pulmonary tuberculosis. Tubercle. 1985;66:187-91.
- [Google Scholar]
- Predictive factors for recurrence of pulmonary tuberculosis in Tunisia: a retrospective study. Rev Mal Respir. 2012;29:412-8.
- [Google Scholar]
- Should we take a history of prior treatment, and check sputum status at 2-3 months when treating patients for tuberculosis? Int J Tuberc Lung Dis. 1998;2:52-5.
- [Google Scholar]






