Translate this page into:
Virulence attributes of Helicobacter pylori isolates & their association with gastroduodenal disease
*Present address: Department of Biochemistry & Molecular Biology, University of Texas Medical Branch, Galveston, TX 77555, USA
Reprint requests: Dr Kashi N. Prasad, Professor, Department of Microbiology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow 226 014, India e-mail: knprasad@sgpgi.ac.in
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives
Certain genotype(s) of Helicobacter pylori strains may play important role in the development of gastric cancer (GC) and peptic ulcer disease (PUD). This study was undertaken to investigate the association of cagA, cagA3/ region subtypes, babA2 and vacA genotypes of H. pylori with GC, PUD and non-ulcer dyspepsia (NUD) as there are no such studies from India.
Methods
A total of 348 consecutive adult patients (NUD 241, PUD 45, GC 62) undergoing upper gastrointestinal endoscopy between September 2002 and May 2007 in a tertiary referral centre at Lucknow, north India, were enrolled. H. pylori infection was diagnosed by rapid urease test, culture, histopathology and PCR. Genotyping for cagA, cagA3/ subtypes, babA2 and vacA was performed by PCR using sequence specific primers.
Results
H. pylori infection was higher in patients with PUD than with GC (80 vs. 56.5%, P < 0.01) and NUD (80 vs. 55.2%, P= 0.002). cagA positive H. pylori isolates were detected in 80 per cent in GC, 83.3 per cent in PUD and 76.7 per cent in NUD with no significant difference among them. Only A subtype of cagA3/ was detected and its distribution in GC, PUD and NUD was 68.8, 69.4 and 52.6 per cent respectively. Presence of babA2 genotype was 31.4 per cent and it had significant association with PUD when compared with NUD (52.8 vs. 26.3%, P<0.003). On univariate regression analysis, s1a allele was associated with GC (P<0.050) and s1a/m2 vacA genotype with both GC (P=0.014) and PUD (P=0.016).
Interpretation & conclusions
H. pylori infection was strongly associated with PUD with a very high proportion of patients with GC have s1a allele and s1a/m2 vacA genotype. Both s1a/m2 vacA genotype and babA2 are associated with PUD. The study shows that different virulence attributes of H. pylori are involved in different gastroduodenal disorders.
Keywords
Gastric cancer
Helicobacter pylori genotypes
peptic ulcer disease
Helicobacter pylori has been identified as a major cause of peptic ulcer disease (PUD) and a risk factor for gastric cancer (GC) and mucosa-associated lymphoid tissue (MALT) lymphoma12. On a global scale, GC is the second commonest cancer in the world. There is substantial international variation in GC incidence with the highest rates reported from China, Japan and other Eastern Asian countries. Epidemiological studies have proved that H. pylori infection is considered as a risk factor for GC, and WHO International Agency for Research on Cancer has classified this bacterium as a definite carcinogen2. While the majority of the H. pylori infected individuals develop no significant clinical disease, some develop two kinds of divergent clinical diseases, PUD and GC3. The reasons for this may be related to differences in genetic susceptibility of the host, environmental factors,and genetic diversity of H. pylori4. In this context, the relevance of specific H. pylori virulence associated genes has been extensively studied. The cytotoxin associated gene A (cagA) was the first to be identified; about 60-70 per cent of H. pylori strains in the West were found to be cagA+ and these strains were associated with duodenal ulcer (DU) and GC56. However, more than 90 per cent of H. pylori strains in Asia are cagA+ irrespective of DU and GC78. The cagA gene can be classified into type A, B, C and D based on its 3′- terminal repetitive sequences8, however, the association of these subtypes with clinical disease remains unclear. The vacuolating toxin (vacA) was subsequently discovered and its allelic variants were identified in the signal region (s1a, s1b, s1c or s2) and mid region (m1 or m2)9. Specifically, vacA s1/m1 strains have higher cytotoxic activity than s1/m2 strains, whereas s2/m2 strains have no cytotoxic activity9. Specific vacA genotypes are associated with level of toxin production and clinical diseases like PUD and GC in different part of the world9–10. Studies have also provided evidence that bacterial adherence factors may also contribute to the pathogenicity of H. pylori. The blood group antigen binding adhesin (babA) has been shown to mediate adherence of H. pylori to human blood group antigens on gastric epithelial cells11. However, the role of babA2 gene in the development of GC and PUD remains undefined. It is well established that differential cagA and vacA genetic characteristics exist in H. pylori strains isolated from different geographical regions. Therefore, using molecular techniques to study the association of H. pylori genotypes or strains with gastroduodenal diseases has become an important study area. The current study was done with an objective to identify the frequency cagA, cagA3/ region subtypes, babA2 and vacA genotypes of H. pylori isolates and their association with gastroduodenal diseases.
Material & Methods
Study population: A total of 348 consecutive adult patients [62 GC, 45 PUD and 241 non ulcer dyspepsia (NUD)] who underwent upper gastrointestinal endoscopy at a tertiary referral center in northern India (Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow) between September 2002 and May 2007 were enrolled in this study. The diagnosis of gastroduodenal diseases was based on clinical, endoscopic and histopathological examinations. Patients with NUD were considered as controls. The ethics committee of the institute granted approval for the study protocol and the written consent was obtained from all the patients. Subjects who had received anti-microbial therapy, H2 receptor blockers, proton pump inhibitors and non-steroidal anti-inflammatory drugs in the preceding 30 days prior to endoscopy or anti-H. pylori treatment in the past were excluded.
Detection of H. pylori infection: During each endoscopy, five antral biopsies were obtained and subjected to the following tests: one biopsy for rapid urease test (RUT), one for culture, two for histopathology and one for DNA extraction and ureA PCR following the standard protocol as described earlier12. H. pylori infection was diagnosed if any of the above tests was positive.
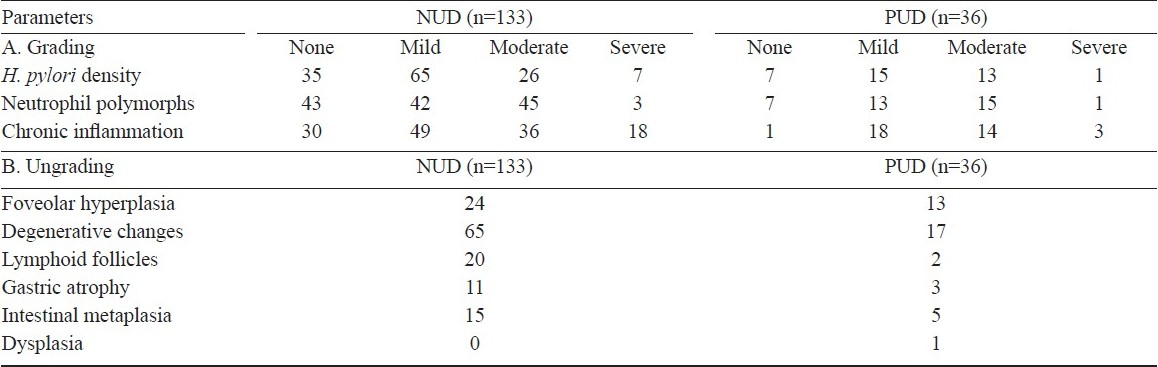
Histopathology: Sections of 5 μm were cut from formalin fixed biopsy, and embedded in paraffin wax. The sections were stained with hematoxylin and eosin for light microscopy. Patients with GC were confirmed by histopathology and classified into intestinal, diffuse and mixed according to the Lauren classification13. The different histological characteristics in patients with PUD and NUD were graded according to the updated Sydney system14.
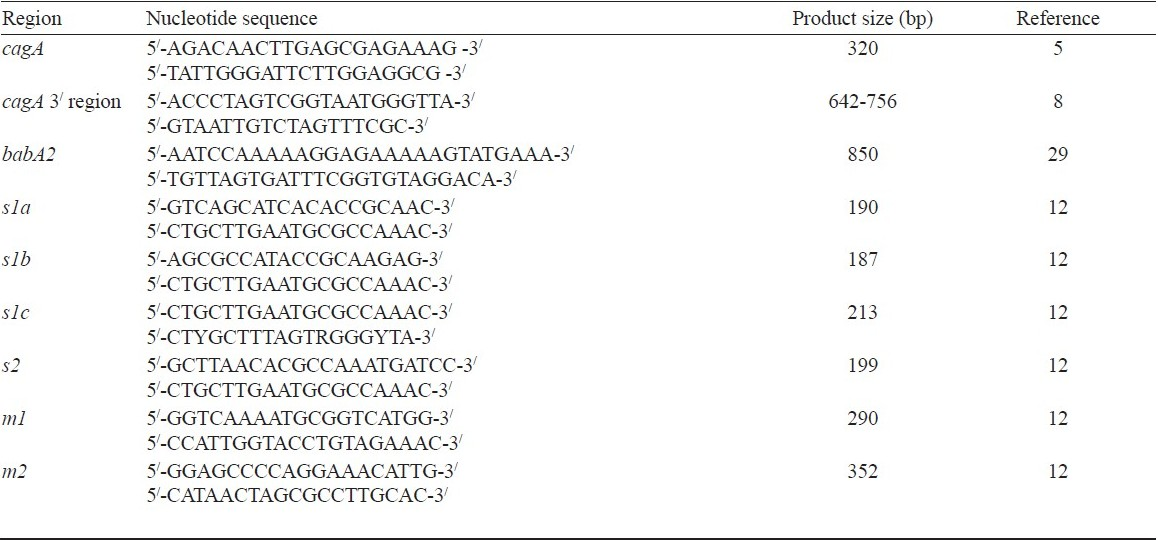
H. pylori genotyping: DNA was isolated from the bacterial growth and H. pylori positive gastric tissues using the QIAamp DNA mini kit (QIAGEN, Hilden, Germany) as per the manufacturer's instruction and subjected to PCR for the presence of cagA. Further, the detection of cagA 3/ region subtypes, babA2 and vacA genotypes of H. pylori was carried out by PCR using specific primers (Table I). PCR was performed in a 50 μl reaction volume containing 100 ng of genomic DNA, 1 X PCR buffer, 1.5 mM MgCl2, 0.2 mM each deoxynucleotide, 0.5 μM each specific primer and 1.25U of Taq DNA polymerase. PCR cycles for cagA and vacA genotypes were as follows: predenaturation at 94°C for 5 min before adding Taq DNA polymerase; 27 cycles of 94°C for 30 sec, 52°C for 30 sec and 70°C for 30 sec. PCR cycles for cagA 3/ region subtypes and babA2 genotypes were as follows: 35 cycles of 94°C for 1 min, 52°C for 1 min and 72°C for 1.30 min. Final extension was given at 72°C for 8 min. All the PCR reactions were performed using thermocycler (Perkin Elmer Cetus, USA). The amplified product was electrophoresed in 2 per cent agarose containing 0.5 μg/ml ethidium bromide and examined under transluminator (UVS Systems, Hammond, USA).
Statistical analysis: The data analysis was performed by SPSS software (Version 12.0, SPSS, Chicago, IL, USA).The association of H. pylori status in relation to gastroduodenal diseases was performed by the Chi-square test. Univariate logistic regression analysis was used to analyze various H. pylori genotypes with gastroduodenal disease. P less than 0.05 was considered significant.
Results
A total of 348 patients (mean age: 46.78 ± 15.96 yr; 216 male) were enrolled and their distributions were as follows: GC 62 (mean age: 56.60 ± 15.42 yr; 47 male), PUD 45 (mean age: 49.47 ± 17.22 yr; 31 male) and NUD 241 (mean age: 43.75 ± 14.76 yr; 138 male).
Occurrence of H. pylori infection in our study population was 204 (58.6%). H. pylori infection was significantly higher in patients with PUD than with GC (80 vs 56.5%, P<0.01) and NUD (80 vs 55.2%, P<0.002). The distribution of different types of GC was as follows: intestinal type 25 (40.3%), diffuse type 37 (59.7%). None of the patients had mixed type of adenocarcinoma. As per the diagnostic criteria, 35 (56.5%) of 62 patients with GC had H. pylori infection. H. pylori infection was detected in significantly higher proportion in intestinal type than diffuse type of adenocarcinoma (18/25, 72% vs 17/37, 45.9%; P<0.05).
The histopathological characteristics of the gastric mucosa in H. pylori positive patients in PUD and NUD are shown in Table II. As per our diagnostic criteria, 133 (55.2%) patients with NUD and 36 (80%) patients with PUD had H. pylori infection.
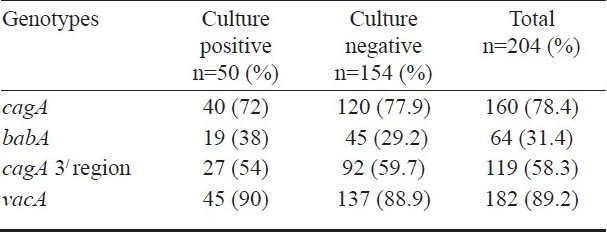
Presence of cagA, cagA 3/ subtypes, babA2 and vacA genotypes of H. pylori were determined on DNA extracted from H. pylori cultures/biopsies by PCR. Data were also compared between culture positive and negative H. pylori isolates (Table III). Overall the cagA presence in H. pylori isolates was 160/204 (78.4%); 28 (80%) of 35 isolates from GC, 30 (83.3%) of 36 from PUD, and 102 (76.7%) of 133 strains from NUD. The cagA was detected in almost equal proportions in H. pylori isolates from all the groups with no significant difference among the groups (Table IV and V).
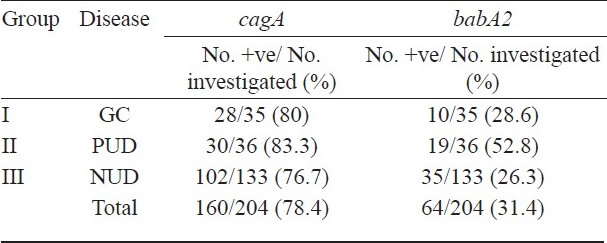
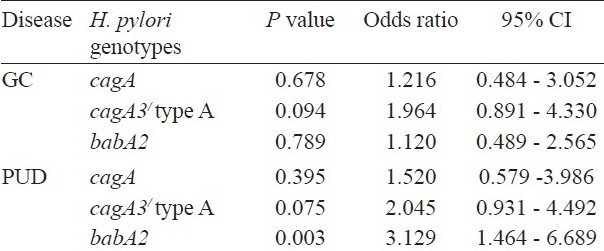
Among four subtypes (A, B, C and D) of cagA 3/ region, only subtype A was detected in 58.3 per cent (119/204) of H. pylori isolates, remaining; 41.7 per cent were untypeable for all four subtypes. Presence of subtype A in GC, PUD and NUD was 68.6 (24/35), 69.4 (25/36) and 52.6 per cent (70/133), respectively. Although the subtype A of cagA 3/ region was higher both in GC and PUD, the difference was not significant (Table V).
babA2 genotype was present in only 31.4 per cent (64/204) of H. pylori isolates. Presence of babA2 in GC, PUD and NUD was 28.6 (10/35), 52.8 (19/36) and 26.3 per cent (35/133), respectively (Table III). babA2 genotype was significantly associated with PUD (P=0.003) and not with GC (P=0.789) (Table V).
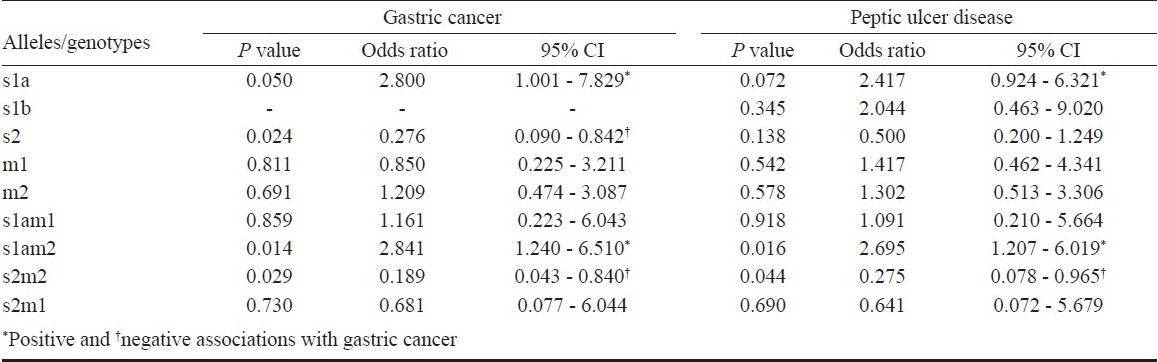
Presence of vacA gene in our H. pylori isolates was 89.2 per cent (182/204) and the frequency in different groups was as follows: GC 94.3 (33/35), PUD 97.2 (35/36) and NUD 85.7 per cent (114/133). Mixed infection was detected in 3 (8.5%) and 5 (4.4%) patients with PUD and NUD, respectively. None of the patients with GC had mixed infection.
The overall distributions of different signal sequence alleles in our patient populations were as follows: s1a 126 (69%), s1b 2 (1.09%), s2 44 (24.17%), s1a/s1b 3 (1.6%), s1a/s2 3 (1.6%), s1a/s1b/s2 2 (1.09%) and untypeable 2 (1.09%). The distribution of signal sequence in different groups of patients was as follows: in GC (n=33)- s1a 28 (84.8%), s2 04 (12.1%), untypeable 01 (3%); in PUD (n=35)- s1a 27 (77.1%), s2 05 (14.3%), s1a/s1b 01 (2.9%), s1b/s2 01 (2.9%), s1a/s1b/s2 01 (2.9%), and in NUD (n=114)- s1a 71 (62.3%), s1b 02 (1.8%) s2 35 (30.7%), s1a/s1b 02 (1.8%), s1a/s2 02 (1.8%), s1a/s1b/s2 01 (0.9%), untypeable 01 (0.9%). Majority of isolates were either s1a or s2. Out of 126 s1a positive isolates, 107 (82.6%) were found to be cagA positive and out of 44 s2 positive isolates, 29 (65.9%) were positive for cagA.
Overall, the most prevalent genotype of vacA was s1a/m2 in our patients as compared to s1a/m1, s2/m2 and s2/m1. Univariate logistic regression analysis showed that s1a allele was associated with gastric cancer (P=0.050) and s1a/m2 vacA genotype was associated with both gastric cancer (P=0.014) and PUD (P = 0.016) (Table VI), while s2/m2 genotype was detected in significantly higher proportion from NUD.
Discussion
The presence of H. pylori in patients with GC in our study was low and had no association with GC. Other tissue based study from India also failed to show an association between H. pylori infection and GC15.
A high occurrence of cagA was seen in H. pylori isolates in the present study; 80 per cent in GC, 83.3 per cent in PUD 76.7 per cent in NUD. No correlation of cagA could be established with GC and PUD, although cagA had been identified as a virulence marker and associated with increased severity of disease in some geographic regions16. High prevalence of cagA (80-90%) independent of the disease status had been reported in other Indian studies as well1718. These studies indicate that cagA cannot be considered as the sole virulence marker for determination of the disease outcome at least in India as has been reported from other geographic regions16. It is possible that some other genes of cagA-PAI are responsible for pathogenicity and disease outcome.
Since allelic variation in cagA exists and distinct H. pylori cagA subtype(s) may circulate in different regions17, differences in cagA subtypes may provide a marker for differences in virulence among cagA-positive H. pylori strains. Yamaoka et al8 reported the different structural subtypes of the cagA 3/ region (A to D) and found that 6 of the 7 type C were present in patients with GC in comparison to non cancer patients8. Overall, subtype A had been more frequently detected in patients with different gastroduodenal diseases including GC78. Subtype A was the most frequent type encountered in Brazil (81%)7. Among four types (A, B, C and D) of cagA 3/ region, only A subtype was found in our study population that was neither associated with GC nor with PUD. The present study suggests that cagA 3/ region variants are not involved in gastric carcinogenesis and PUD. A total of 41.7 per cent isolates were found untypable with selected primers.
There is inconsistency in the prevalence and association of babA2 genotype with the gastric diseases. However we reported 31.4 per cent prevalence of babA2 in our population and found significant association with PUD when compared with NUD (P=0.003). Studies from China and four European countries reported the prevalence of babA2 25 and 30 - 60 per cent, respectively and found no correlation with clinical disease1920. Recently, a study from Thailand reported 92 per cent positivity of babA2 gene and found no significant association with clinical outcome21. However, a significant association of babA2 genotype with duodenal ulcer (DU) and GC was observed in Brazil and Germany2223.
We showed that s1a allele had significant association with GC and it was more frequently present in patients with PUD. The prevalence of vacAs2 strain in our population was approximately 25 per cent, which is similar to our previous report of 27 per cent in children24, but is discordant with other Indian studies where the prevalence of vacAs2 strain ranged from 2 to 10 per cent1725. We also found very high number of cagA positive vacAs2 strain (65.9%) in our patient population. This is the first study that reports high prevalence of cagA positive in vacAs2 strains. These differences may be geographical and because of high frequency of cagA positive strains in our population with no significant difference between disease and control populations. Excluding the mixed infection and combining the groups, we observed that vacA s1a/m2 was frequently found in our study population, which is similar to several other findings26. Univariate regression analysis in our patients showed that s1a/m2 vacA genotype was associated with both gastric cancer (P=0.014) and PUD (P=0.016). These findings are markedly different from those reported association of s1a/m1 vacA genotype with PUD and GC2728.
In contrary to this, few studies had found no correlation of vacA genotypes with clinical outcome. However, Bulent et al found that the presence of vacA genotype was not a predictive marker for peptic ulcer and non-ulcer dyspepsia28.
In conclusion, H. pylori infection is strongly associated with PUD. cagA and cagA3/ region subtypes of H. pylori have no association with GC and PUD in the study. A significantly higher proportion of patients with GC have s1a allele and s1a/m2 vacA genotype. Besides s1a/m2 vacA genotype, babA2 is also associated with PUD. The study suggests that different virulence attributes of H. pylori are involved in differential outcome of gastric disorders.
The study was supported by Council of Science and Technology, Government of Uttar Pradesh, India, through grant no. CST/SERPD/D-3402. The first two authors (AS, SS) acknowledge the financial assistance received from Indian Council of Medical Research (ICMR) and Department of Biotechnology (DBT), Government of India, New Delhi, through senior research fellowship (grant no. 80/512/2004-ECD-I) and junior research fellowship (grant no. DBT-JRF/07-08/631), respectively.
References
- Progression of chronic atrophic gastritis associated with Helicobacter pylori infection increases risk of gastric cancer. Int J Cancer. 2004;109:138-43.
- [Google Scholar]
- International Agency for Research on Cancer. Schistosomes, liver flukes and Helicobacter pylori. IARC Monogr Eval Carcinog Risk Hum. 1994;61:177-241.
- [Google Scholar]
- Gastric cancer and H. pylori: Host genetics open the way. Gastroenterology. 2001;121:1002-4.
- [Google Scholar]
- The role of the HLA-DQA1 gene in resistance to atrophic gastritis and gastric adenocarcinoma induced by Helicobacter pylori infection. Cancer. 1998;82:1013-8.
- [Google Scholar]
- Molecular characterization of the 128-kDa immunodominant antigen of Helicobacter pylori associated with cytotoxicity and duodenal ulcer. Proc Natl Acad Sci USA. 1993;90:5791-5.
- [Google Scholar]
- Risk for gastric cancer in people with CagA positive or CagA negative Helicobacter pylori infection. Gut. 1997;40:297-301.
- [Google Scholar]
- Consensus and variable region PCR analysis of Helicobacter pylori 3′ region of cagA gene in isolates from individuals with or without peptic ulcer. J Clin Microbiol. 2001;39:606-12.
- [Google Scholar]
- Variants of the 3′ region of the cagA gene in Helicobacter pylori isolates from patients with different H. pylori-associated diseases. J Clin Microbiol. 1998;36:2258-63.
- [Google Scholar]
- Mosaicism in vacuolating cytotoxin alleles of Helicobacter pylori. Association of specific vacA types with cytotoxin production and peptic ulceration. J Biol Chem. 1995;270:17771-7.
- [Google Scholar]
- Clinical and pathological importance of heterogeneity in vacA, the vacuolating cytotoxin gene of Helicobacter pylori. Gastroenterology. 1997;112:92-9.
- [Google Scholar]
- Attachment of Helicobacter pylori to human gastric epithelium mediated by blood group antigens. Science. 1993;262:1892-5.
- [Google Scholar]
- Genotypes of Helicobacter pylori in children with upper abdominal pain. J Gastroenterol Hepatol. 2003;18:1018-23.
- [Google Scholar]
- The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand. 1965;64:31-49.
- [Google Scholar]
- Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis. Houston 1994. Am J Surg Pathol. 1996;20:1161-81.
- [Google Scholar]
- Helicobacter pylori and gastric carcinoma: evidence for the link. Natl Med J India. 2000;13:329.
- [Google Scholar]
- Infection with Helicobacter pylori strains possessing cagA is associated with an increased risk of developing adenocarcinoma of the stomach. Cancer Res. 1995;55:2111-5.
- [Google Scholar]
- Distinctiveness of genotypes of Helicobacter pylori in Calcutta, India. J Bacteriol. 2000;182:3219-27.
- [Google Scholar]
- UreC PCR based diagnosis of Helicobacter pylori infection and detection of cagA gene in gastric biopsies. Indian J Pathol Microbiol. 2002;45:31-7.
- [Google Scholar]
- Relationship between iceA1, iceA2 and babA2 genes of Hp in Xi’an and gastroduodenal diseases. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi. 2007;23:520-2.
- [Google Scholar]
- Correlation of the Helicobacter pylori adherence factor BabA with duodenal ulcer disease in four European countries. FEMS Immunol Med Microbiol. 2005;44:151-6.
- [Google Scholar]
- Prevalence of Helicobacter pylori vacA, cagA, cagE, iceA and babA2 genotypes in Thai dyspeptic patients. Int J Infect Dis. 2008;12:30-6.
- [Google Scholar]
- babA2- and cagA-positive Helicobacter pylori strains are associated with duodenal ulcer and gastric carcinoma in Brazil. J Clin Microbiol. 2003;41:3964-6.
- [Google Scholar]
- Clinical relevance of the Helicobacter pylori gene for blood-group antigen-binding adhesin. Proc Natl Acad Sci USA. 1999;96:12778-83.
- [Google Scholar]
- Helicobacter pylori infection, histopathological gastritis and gastric epithelial cell apoptosis in children. Acta Paediatr. 2006;95:732-7.
- [Google Scholar]
- Virulence genes in Helicobacter pylori strains from West Bengal residents with overt H. pylori-associated disease and healthy volunteers. J Clin Microbiol. 2002;40:2622-5.
- [Google Scholar]
- Genotypic characterization of Helicobacter pylori cagA and vacA from biopsy specimens of patients with gastroduodenal diseases. Mt Sinai J Med. 2006;73:622-6.
- [Google Scholar]
- Distribution of vacA alleles and cagA status of Helicobacter pylori in peptic ulcer disease and non-ulcer dyspepsia. Clin Microbiol Infect. 2004;10:1102-4.
- [Google Scholar]
- Association of CagA and VacA presence with ulcer and non-ulcer dyspepsia in a Turkish population. World J Gastroenterol. 2003;9:1580-3.
- [Google Scholar]
- Relationship between Helicobacter pylori babA2 status with gastric epithelial cell turnover and premalignant gastric lesions. Gut. 2002;51:480-4.
- [Google Scholar]






