Translate this page into:
Utility of p57 immunohistochemistry in differentiating between complete mole, partial mole & non-molar or hydropic abortus
Reprint requests: Dr Rakhee Kar, Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education & Research, Puducherry 605 006, India e-mail: drrakheekar@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
There is considerable inter-observer variability in the diagnosis of molar pregnancies by histomorphological examination of products of conception (POC). The p57KIP2 gene is paternally imprinted and expressed from the maternal allele. On immunohistochemistry (IHC) with p57, complete mole (CM) shows absent staining whereas hydropic abortus (HA) and partial mole (PM) show positive staining. This study was undertaken to evaluate the role of p57 IHC along with histomorphology in differentiating between CM, PM and non-molar or HA.
Methods:
This was a cross-sectional study over a period of three and a half years on archival material. Detailed histomorphological review along with p57 IHC was carried out in 28 diagnosed cases (23 CM, 4 PM and 1 molar pregnancy not categorized) and 25 controls of four normal placentas and 21 POC (8 non-hydropic and 13 HA).
Results:
In 14.8 per cent (4/27) cases, there was discordance in accurate subtyping of molar pregnancy. One case of CM showed inconsistent IHC pattern. In 15.4 per cent (2/13) HA, molar pregnancy was final diagnosis. After final review, there were 25 CM, five PM, 22 non-molar controls including 10 HA and one not assigned (PM/HA). IHC with p57 was negative in 96 per cent CM and positive in 100 and 95 per cent PM and non-molar controls, respectively.
Interpretation & conclusions:
This study showed that negative p57KIP2 immunostaining reliably identified CM and could be used in association with the histological findings to distinguish CM from its mimics.
Keywords
Complete mole
hydropic abortus
immunohistochemistry
molar pregnancy
p57
partial mole
Morphologic examination of products of conception (POC) forms the main diagnostic tool in the differential diagnosis of complete mole (CM) and partial mole (PM). However, the criteria are subjective and show considerable inter-observer variability1. With early diagnosis and evacuation of molar pregnancies, the differentiation from early non-molar placentation, especially hydropic abortus (HA), is difficult. The p57KIP2 gene encoding for p57, a cell cycle inhibitor, is strongly paternally imprinted and expressed from the maternal allele. Because CM results from fertilization of an egg that has lost its chromosomes and the genetic material is completely paternally derived, p57KIP2 immunostaining is absent whereas HA and PM show positive staining2. Thus, in equivocal cases, p57 immunohistochemistry (IHC) is an important adjunct to the diagnosis3. This study was undertaken to evaluate the role of p57 IHC along with histomorphology in differentiating between CM, PM and non-molar or HA.
Material & Methods
This was a cross-sectional study on archival material collected over three and a half years (January 2010-June 2013) done in the department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), a tertiary care hospital in Puducherry, India. All molar pregnancies reported on POC and nearly equal numbers of non-molar abortus/placental sections based on convenient sampling were taken as controls. Specimens of POC showing only decidua, fibrin or blood clot but no chorionic villi were excluded from the study. A total of 28 cases of molar pregnancies and 25 controls were included in the study.
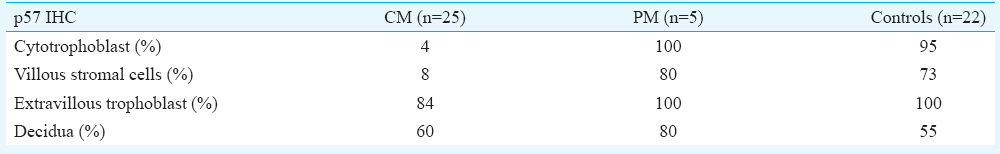
IHC for p57 was done with p57Kip2 Ab-6 (Thermo Fisher scientific, Fremont, CA, USA). Microscopic evaluation of all the haematoxylin and eosin and p57 IHC stained slides was done on a teaching microscope (Olympus BX53, Olympus Corporation, Tokyo, Japan) by a pathologist blinded to the original histopathology report. In IHC, nuclear staining for p57 was observed in the villous cytotrophoblast cells and also in villous stromal cells. Any distinct nuclear staining was taken as positive. Extravillous/implantation site trophoblastic cells and decidua served as positive internal control.
Those cases with difference of opinion with original histopathology report or an inconsistent pattern on IHC were reviewed to assign final diagnosis. The observations were recorded, tabulated and analyzed. The study was approved by the Institute Ethics Committee (No. JIP/IEC/SC/2/363/2013).
Results
Twenty eight cases of molar pregnancies (23CM, 4PM, 1 not categorized) and 25 controls (placenta and non-molar POC) diagnosed on histomorphology were studied along with IHC. The diagnosis of CM was concordant with p57 IHC showing negative staining in cytotrophoblast in 20 cases, and also, the case not categorized was diagnosed as CM. In two diagnosed CMs, there was doubt of PM based on morphology showing lesser degree of villous oedema and more scalloping; these showed p57 positivity confirming PM. One case fitted morphologically with CM but showed p57 positivity in a proportion of villous cytotrophoblast.
Among PM, two cases had concordant IHC showing positive staining. Two cases were discordant with absent p57 positivity; morphology showed less degree of trophoblastic hyperplasia as compared to other CMs. Taking IHC into consideration, these were categorized as CM. Hence, in 14.8 per cent (4/27) cases, there was discordance in accurate subtyping of molar pregnancy. One case of CM showed inconsistent IHC pattern.
Controls included four normal placentas and 21 POC (8 non-hydropic and 13 HA). In three HAs, possibility of molar pregnancy was considered on review. All these showed fewer villi and background haemorrhage or infarction. In one of these, the villi were all hydropic (90%), avascular with the presence of trophoblastic hyperplasia. However, no cistern formation was seen. The p57 IHC showed absent staining in the villous trophoblast but was present in the extravillous site trophoblast and decidua; hence, the final diagnosis was given as CM. In two others, possibility of PM was considered based on a proportion of villi appearing avascular and hydropic (50 and 40%, respectively) and the rest appearing vascularized or infarcted, respectively. Mild trophoblastic hyperplasia was seen and IHC was positive. The former favoured PM and the latter could not be resolved with certainty between PM and HA. Hence, in 15.4 per cent (2/13) HA, molar pregnancy was final diagnosis.
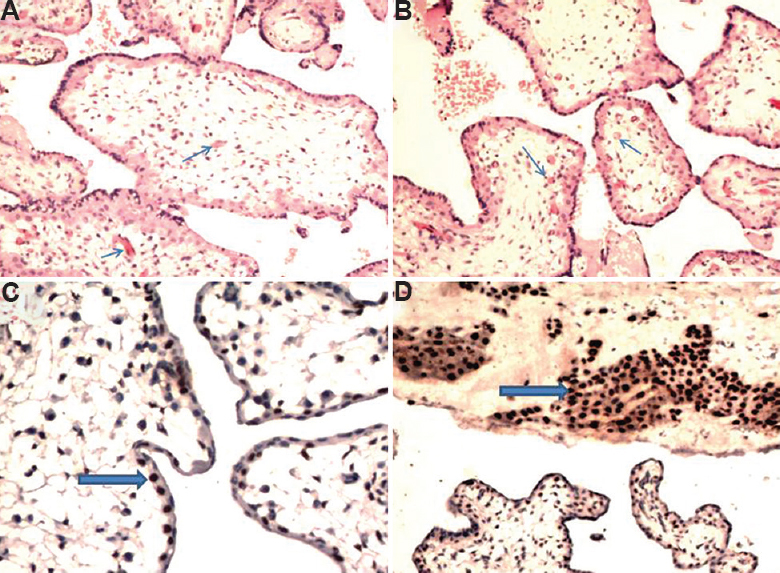
After final review, there were 25 CM, five PM, 22 non-molar controls including 10 HA and one not assigned (PM/HA). The original and final diagnosis with IHC is summarized in Table I. CMs showed large villous hydrops with cisterns, marked and circumferential trophoblastic hyperplasia, extravillous/implantation site trophoblastic proliferation with atypia in some. PMs showed two populations of villi (enlarged hydropic avascular and smaller normal), mild trophoblastic hyperplasia, marked scalloping and central cistern (Table II). Identifiable embryonic or foetal tissue was not seen. HA showed varying proportion of mildly enlarged oedematous, vascularized villi. The salient histomorphological features and IHC staining pattern in a representative case of CM, PM and HA are illustrated in Figures 1-3, respectively. IHC findings are summarized in Table III.

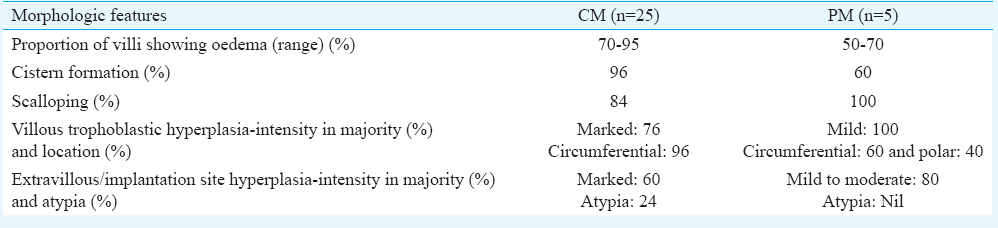
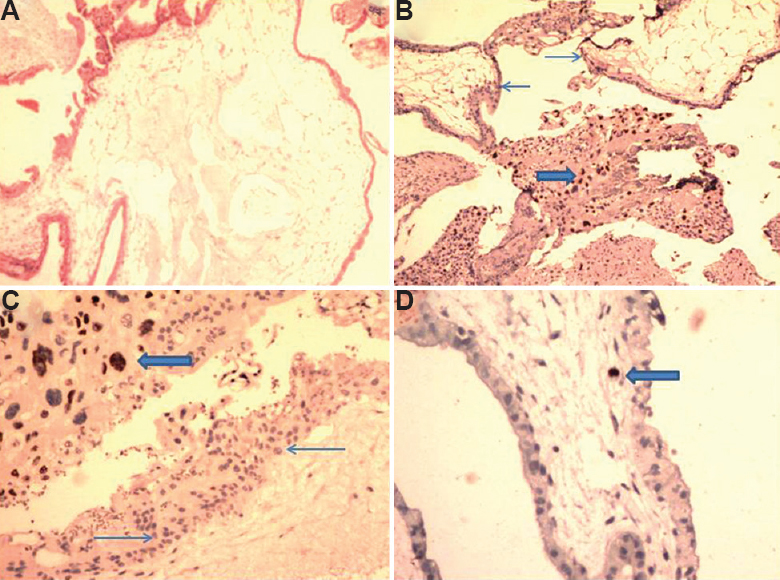
- A case of complete mole showing (A) villous oedema with cistern formation (H & E, ×40); (B and C) p57 negativity in cytotrophoblast (thin arrows) with positivity in extravillous site (thick arrow; IHC, ×40 and ×100 respectively); (D) occasional stromal macrophage showing positivity (thick arrow; IHC, ×200).

- A case of partial mole showing (A) villous oedema with scalloping (H & E, ×40); (B) mild trophoblastic hyperplasia (thin arrow; H & E, ×100); (C) p57 positivity in cytotrophoblast(thick arrows; IHC, ×200); (D) case of hydropic abortus reclassified as partial mole showing a proportion of hydropic avascular villi (thick arrow) and a few normal appearing villi (thin arrows; H & E, ×40); inset showing p57 positivity in cytotrophoblast (thick arrow; IHC, ×200).
- A case of hydropic abortus showing (A and B) villous oedema involving almost all villi; however, villi are vascularized (thin arrows) and do not show trophoblastic hyperplasia (H & E, ×100); (C) p57 positivity in cytotrophoblast (thick arrow; IHC, ×200); (D) p57 positivity in decidua (thick arrow; IHC, ×100).
Discussion
IHC with p57 was negative in 96 per cent CM and positive in 100 and 95 per cent PM and non-molar controls, respectively. The morphologic findings were in conjunction with reported literature456. There was discordance in accurate sub-typing of moles in four cases and two cases were underdiagnosed as POC only which were accurately resolved with IHC. This constraint in accurate diagnosis has been reported in another study with comparable groups and numbers of cases where correct diagnosis on morphology alone was possible in 82 per cent of HA specimens, 33 per cent of PMs, and 67 per cent of CMs4. In our study, correct diagnosis on morphology alone was 84 per cent for CM, 40 per cent for PM and 100 per cent for HA.
IHC has certain limitations as it cannot distinguish between PM and HA as was seen in one control sample. Also, one case morphologically consistent with CM showed positive p57 staining. The finding of positive staining has been reported in repeated molar gestations possibly due to some other pathogenesis, especially in recurrent moles which may be biparental in genotype7, and also due to trisomy of chromosome 11 (retained maternal allele), accounting for the aberrant p57 expression8. In such cases ploidy analysis would have a role. However, IHC has the advantage of differentiating HA from CM, a distinction not made by ploidy analysis2.
Our study had some limitations. The proportion of HA found to be molar pregnancy on review may not be truly representative due to convenient sampling of controls. Ploidy analysis was not done and the number of PMs was less and clinical association was not available for the cases.
In conclusion, the results of our study show that negative p57KIP2 immunostaining may reliably identify CM and may be used in association with the histological findings to distinguish CM from its mimics.
Acknowledgment
The first author (AS) acknowledges the Indian Council of Medical Research, New Delhi, India for rendering partial financial support for this project under the Short Term Studentship programme (ICMR-STS)-2013.
Conflicts of Interest: None.
References
- Interobserver and intraobserver variability in the diagnosis of hydatidiform mole. Am J Surg Pathol. 2005;29:942-7.
- [Google Scholar]
- p57KIP2 immunohistochemistry in early molar pregnancies: Emphasis on its complementary role in the differential diagnosis of hydropicabortuses. Am J Surg Pathol. 2009;33:805-17.
- [Google Scholar]
- p57KIP2 immunohistochemical expression: A useful diagnostic tool in discrimination between complete hydatidiform mole and its mimics. Arch Gynecol Obstet. 2011;283:743-8.
- [Google Scholar]
- Comparison of fluorescence in situ hybridization, p57 immunostaining, flow cytometry, and digital image analysis for diagnosing molar and nonmolar products of conception. Am J Clin Pathol. 2010;133:196-204.
- [Google Scholar]
- Audit of partial and complete hydatidiform moles in tertiary care hospital in rural inhabitants of India. Indian J Health Sci. 2014;7:104-7.
- [Google Scholar]
- Gestational trophoblastic disease: A prospective study of 82 cases and utility of p57 immunohistochemistry in differentiating complete and partial mole. J Evol Med Dent Sci. 2014;3:13407-14.
- [Google Scholar]
- Diagnosis of hydatidiform moles using p57 immunohistochemistry and HER2 fluorescent in situ hybridization. Am J Clin Pathol. 2008;129:749-55.
- [Google Scholar]
- Diagnosis and subclassification of hydatidiform moles using p57 immunohistochemistry and molecular genotyping: Validation and prospective analysis in routine and consultation practice settings with development of an algorithmic approach. Am J Surg Pathol. 2009;33:805-17.
- [Google Scholar]






